Drug Interaction: What You Need to Know to Stay Safe
When you take more than one medication—or even a herbal tea with your pill—you’re risking a drug interaction, a harmful or reduced effect when two or more substances affect each other in the body. Also known as medication interaction, it’s not just about pills clashing—it’s about what you eat, drink, or take naturally changing how your drugs work. This isn’t rare. One in five people on multiple meds experience an interaction, and some can land you in the hospital overnight.
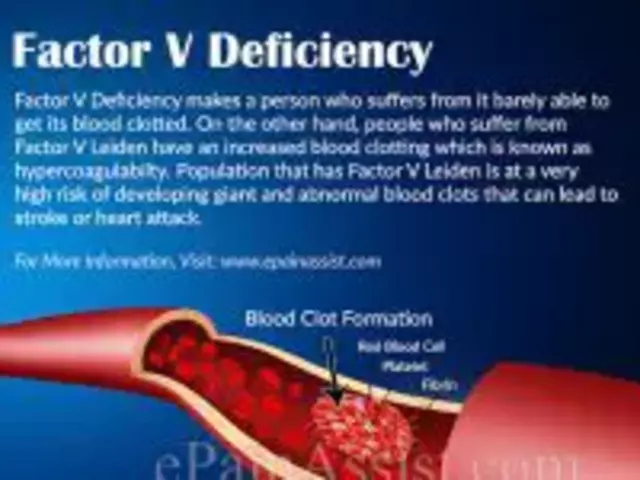
Take hypertensive crisis, a sudden, life-threatening spike in blood pressure. It doesn’t just happen out of nowhere. It’s often triggered by mixing common antidepressants like venlafaxine with decongestants, or even aged cheese and red wine if you’re on an MAOI. Or consider herbal teas, natural remedies that can interfere with blood thinners, birth control, or statins. Green tea might lower your cholesterol, but it can also make warfarin useless. Chamomile might calm you, but it can cancel out your birth control. These aren’t myths—they’re documented cases.
Even your diabetes meds can play dirty. Insulin and sulfonylureas can drop your blood sugar too low if you add certain antibiotics or alcohol. And it’s not always obvious. You might feel fine until your heart races, your vision blurs, or you pass out. Older adults are especially at risk because their bodies process drugs slower, and they often take five or more meds a day. That’s why a simple change—like switching from a brand to a generic—can throw off your balance if the fillers or coatings differ slightly. And yes, that’s why some people report side effects from generics that they never had with the brand.
You don’t need to be a pharmacist to protect yourself. You just need to know what’s in your medicine cabinet, what you’re eating, and what your doctor didn’t tell you. The posts below cover real cases: how a missed refill led to a hypertensive emergency, how a cup of tea caused a stroke, how a generic pill made someone dizzy for weeks, and how a diabetic almost died from a common cold medicine. These aren’t edge cases. They’re everyday mistakes. And they’re preventable.
Below, you’ll find clear, no-fluff guides on how to spot dangerous combinations, what to ask your pharmacist, how to read labels that hide risks, and what alternatives actually work when your meds don’t play nice. No theory. No jargon. Just what you need to keep yourself—and your loved ones—safe.

- Dec 5, 2025
- Posted by Cillian Osterfield
Warfarin and NSAIDs: Why Combining Them Increases Bleeding Risk
Combining warfarin and NSAIDs can more than quadruple your risk of serious bleeding. Learn why this interaction is dangerous, which painkillers are safest, and what to do if you need pain relief while on blood thinners.
Categories
- Health and Wellness (72)
- Medications (70)
- Health and Medicine (28)
- Pharmacy Services (12)
- Mental Health (9)
- Health and Career (2)
- Medical Research (2)
- Business and Finance (2)
- Health Information (2)
Latest Posts
©2026 heydoctor.su. All rights reserved