Warfarin-NSAID Risk Calculator
Warning: Combining warfarin with NSAIDs significantly increases bleeding risk. This tool shows the relative risk increase based on medical studies. Always consult your doctor before making changes to your medication.
Relative Bleeding Risk Increase
This means your bleeding risk is -- times higher than taking warfarin alone.
Combining warfarin and NSAIDs isn’t just a minor caution-it’s a recipe for serious, sometimes deadly, bleeding. If you’re on warfarin for atrial fibrillation, a mechanical heart valve, or deep vein thrombosis, and you reach for ibuprofen or naproxen for a headache or sore knee, you’re putting yourself at risk. This isn’t theoretical. It’s backed by decades of research, hospital data, and real-world outcomes. The combination doesn’t just slightly raise the chance of bleeding-it can more than quadruple your risk.
How Warfarin Works (And Why It’s Already a Tightrope Walk)
Warfarin is an old drug, first approved in the 1950s, but it’s still widely used because it’s effective and cheap. It works by blocking vitamin K, which your body needs to make clotting factors II, VII, IX, and X. Without those, your blood can’t form clots as easily. That’s the point-it prevents dangerous clots from forming in your heart or legs.
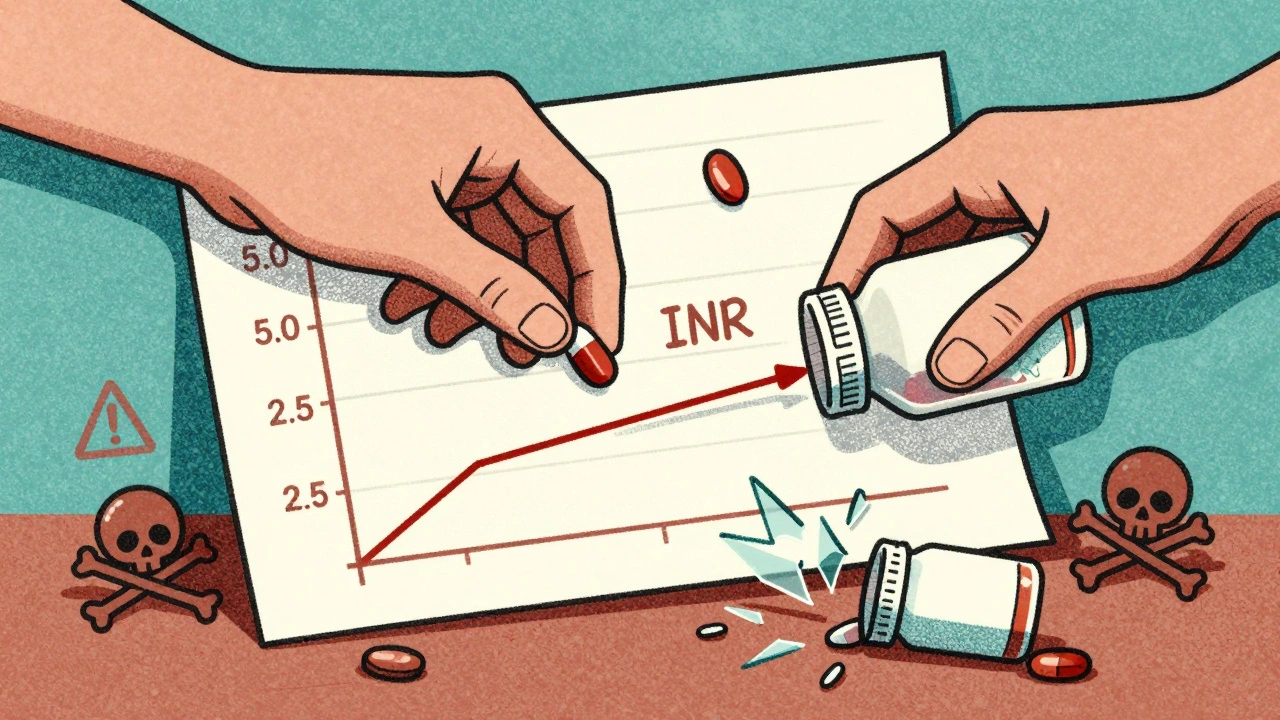
But here’s the catch: warfarin’s effect is delicate. Too little, and you’re at risk for a stroke or clot. Too much, and you bleed internally-sometimes without warning. Doctors track this balance using a blood test called INR (International Normalized Ratio). A normal INR is around 1.0. For most people on warfarin, the target is between 2.0 and 3.0. Anything above 4.0 is considered dangerous.
Even small changes in diet, other medications, or illness can push your INR out of range. That’s why regular testing is required. And when you add an NSAID into the mix, it doesn’t just nudge your INR-it can slam it.
How NSAIDs Make Things Worse
NSAIDs-like ibuprofen, naproxen, diclofenac, and even aspirin-are common pain relievers. But they don’t just block pain signals. They also interfere with platelets, the blood cells that start the clotting process. They do this by inhibiting an enzyme called COX-1, which reduces thromboxane A2, a chemical that tells platelets to stick together.
Think of it like this: warfarin slows down the entire clotting system. NSAIDs disable the first responders-the platelets. Together, they create a double hit. Your blood can’t clot properly from the start, and even if it tries, the platelets can’t do their job.
On top of that, NSAIDs damage the stomach lining. They reduce protective prostaglandins, which normally shield your stomach from acid. This makes ulcers more likely. When you combine that with warfarin’s thinning effect, even a small stomach ulcer can turn into a major bleed.
The Numbers Don’t Lie: How Much Risk Are We Talking?
Studies have measured this risk precisely. One major analysis found that people taking both warfarin and an NSAID were 2.09 times more likely to have a serious bleed than those taking warfarin alone.
But not all NSAIDs are equal:
- Naproxen: 4.1 times higher risk
- Diclofenac: 3.3 times higher risk
- Ibuprofen: 1.79 times higher risk
That means if you take naproxen with warfarin, you’re over four times more likely to bleed than if you were just on warfarin. And the bleeding isn’t just in your stomach. Brain bleeds (intracranial hemorrhage) jump by 3.22 times. Lung bleeds go up by 36%. Urinary tract bleeds rise by 57%. And you’re nearly three times more likely to develop anemia from blood loss.
One study of 98 patients on warfarin found that nearly 40% had a spike in their INR by 15% or more after starting an NSAID. That’s not a small fluctuation-it’s enough to push someone into a dangerous zone.
Who’s Most at Risk?
Not everyone on warfarin who takes an NSAID will bleed. But some people are far more vulnerable:
- Those taking more than 40 mg of warfarin per week-higher doses mean less room for error.
- People with low baseline INR-meaning their blood was already clotting closer to normal, so any extra thinning hits harder.
- Patients on multiple other medications-polypharmacy increases the chance of hidden interactions.
- Those using meloxicam-a specific NSAID linked in studies to significant INR spikes.
Age matters too. Older adults are more likely to be on warfarin and more likely to take NSAIDs for arthritis. They also have thinner blood vessel walls and less reserve to handle blood loss. That’s why this interaction is especially dangerous for people over 65.
It’s Not Just Warfarin-DOACs Are Risky Too
You might think switching to a newer blood thinner like apixaban or dabigatran (DOACs) makes this safer. It doesn’t. Studies show NSAIDs still raise bleeding risk with DOACs. One study found that among patients on dabigatran, NSAID use led to higher rates of major bleeding, hospitalization, and GI bleeding-even if the relative risk wasn’t as high as with warfarin.
The absolute risk is still there. And for people on DOACs, the bleeding is often harder to reverse. Unlike warfarin, which can be undone with vitamin K or fresh frozen plasma, DOACs need expensive, specialized antidotes that aren’t always available.
What Should You Do Instead?
If you’re on warfarin and need pain relief, you have better options:
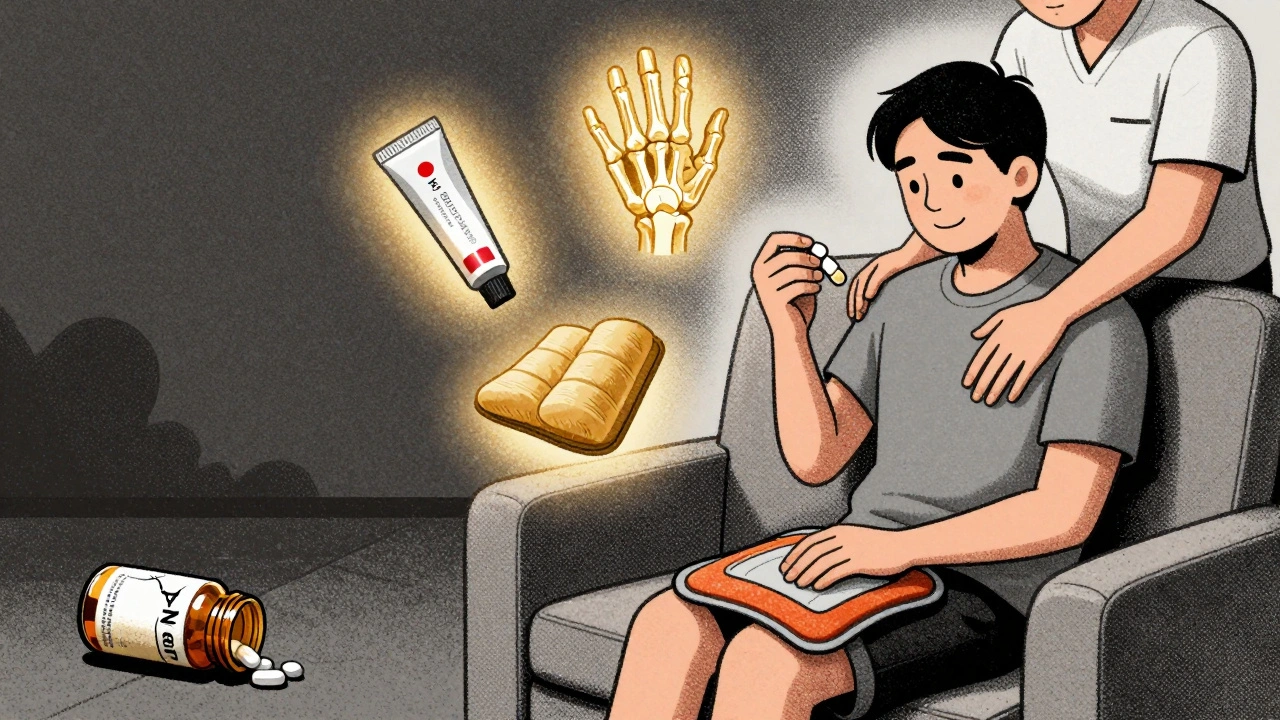
- Acetaminophen (Tylenol): Up to 3,000 mg per day is generally safe for most people on warfarin. It doesn’t affect platelets or the stomach lining. It’s the first-line recommendation from major medical guidelines.
- Topical pain relievers: Creams or patches with lidocaine, menthol, or diclofenac (applied to the skin) avoid systemic absorption and are much safer.
- Physical therapy and heat/cold therapy: For joint or muscle pain, these can reduce reliance on pills entirely.
- Low-dose aspirin: Only if you’re already on it for heart protection. Never start aspirin on your own-it’s still an NSAID and can interact.
If your doctor insists you need an NSAID-for severe arthritis, for example-they should prescribe the lowest possible dose for the shortest time. And they should pair it with a proton pump inhibitor (PPI) like pantoprazole to protect your stomach. Even then, your INR must be checked within 3 to 5 days of starting the NSAID, then weekly while you’re on both drugs.
Why Do Doctors Still Prescribe This Combo?
It shouldn’t happen. But it does. A 2022 study found that nearly 29% of people on warfarin got at least one NSAID prescription in a year. That’s not a small number-it’s a systemic failure.
Doctors are busy. Patients ask for Advil. Pharmacists don’t always catch the interaction. Electronic health records don’t always flag it clearly. And many patients don’t realize that a “common” painkiller can be dangerous with their blood thinner.
This isn’t about blame. It’s about awareness. You need to be your own advocate. If you’re on warfarin, don’t take any new medication-including over-the-counter ones-without checking with your doctor or pharmacist.
Signs You Might Be Bleeding
If you’re on both drugs, watch for these red flags:
- Bright red or black, tarry stools
- Unexplained bruising, especially large or painful ones
- Bleeding gums when brushing teeth
- Nosebleeds that won’t stop
- Headaches, dizziness, confusion (possible brain bleed)
- Dark urine or blood in urine
- Severe abdominal pain
- Unusual fatigue or shortness of breath (signs of anemia from blood loss)
If you notice any of these, stop the NSAID and call your doctor immediately. In some cases, you may need to go to the ER.
Bottom Line
Warfarin and NSAIDs don’t mix. The risk isn’t small. It’s large, well-documented, and preventable. The safest choice is to avoid NSAIDs entirely. Use acetaminophen. Try physical therapy. Use topical creams. If you absolutely must use an NSAID, do it under strict medical supervision-with close INR monitoring and stomach protection.
There’s no shortcut here. Your life depends on it.
Can I take ibuprofen with warfarin if I only use it once in a while?
Even occasional use of ibuprofen with warfarin can spike your INR and increase bleeding risk. Studies show a 1.79-fold increase in bleeding even with short-term use. It’s not safe to assume a single dose is harmless. Always check with your doctor before taking any NSAID, even once.
Is naproxen worse than ibuprofen with warfarin?
Yes. Naproxen carries a 4.1-fold higher risk of bleeding compared to warfarin alone, while ibuprofen raises the risk by 1.79-fold. Naproxen lasts longer in your system and has a stronger effect on platelets, making it one of the riskiest NSAIDs to combine with warfarin.
What painkiller is safest with warfarin?
Acetaminophen (Tylenol) is the safest option for pain relief while on warfarin. It doesn’t affect platelets or the stomach lining and doesn’t interfere with INR levels. Stick to no more than 3,000 mg per day unless your doctor says otherwise.
Should I stop taking NSAIDs if I’m on warfarin?
Yes, unless your doctor specifically says otherwise and has a plan to monitor you closely. Most guidelines recommend avoiding NSAIDs entirely for people on warfarin. Safer alternatives like acetaminophen, physical therapy, or topical treatments are preferred.
Can I take aspirin with warfarin?
Aspirin is an NSAID and can increase bleeding risk with warfarin. If you’re taking low-dose aspirin for heart protection, don’t stop without talking to your doctor. But don’t start aspirin on your own. Even low-dose aspirin adds to the bleeding risk and should only be used if there’s a clear medical reason.
How often should my INR be checked if I must take an NSAID?
If you must take an NSAID while on warfarin, your INR should be checked within 3 to 5 days after starting the NSAID. Then, weekly while you’re taking both. Once you stop the NSAID, check your INR again in a few days to make sure it returns to your target range.






7 comments
Chris Park
Let’s be real-this whole warfarin-NSAID thing is a pharmaceutical industry scam to keep you coming back for more INR tests and PPI prescriptions. They don’t want you to know that vitamin K2 supplements can reverse any ‘bleeding risk’-but the FDA won’t let you hear that. You think they care about your stomach? No. They care about your monthly lab fees. The real danger? Doctors who don’t even know how warfarin metabolism works. It’s not about platelets-it’s about CYP2C9 polymorphisms. And no one’s talking about that. Because the truth doesn’t sell.
Geraldine Trainer-Cooper
so like… just don’t take ibuprofen? wow. mind blown. i’ve been taking it for my back since 2018 and my INR’s been fine. maybe the real problem is doctors who don’t listen? 🤷♀️
Kenny Pakade
Ugh. Another ‘medical authority’ telling people what to do. You know what’s really dangerous? Trusting some guy in a white coat who got his degree from a state school. I’ve been on warfarin for 12 years and I take Advil every time my knee acts up. My doctor’s fine with it. You want to live in fear? Go ahead. I’ll be living. And yeah, I’m American-we don’t need your European overcaution.
brenda olvera
thank you for writing this. i’m 71 and on warfarin for afib. my knee’s been killing me but i’ve been too scared to ask my dr about painkillers. now i know to ask for tylenol and a physical therapist. also i’m gonna try that topical diclofenac cream. you made me feel less alone. we got this 💪
Myles White
It’s fascinating how this interaction is so well-documented yet still so pervasive in clinical practice. The pharmacokinetic and pharmacodynamic overlap between warfarin and NSAIDs isn’t just additive-it’s synergistic, and that’s why the risk multiplier is so high. The fact that even low-dose, short-term use can cause clinically significant INR spikes speaks to how delicate the therapeutic window is. And the fact that this isn’t just a warfarin issue but extends to DOACs as well? That’s a systemic problem in pain management for anticoagulated patients. We need better education at every level-from pharmacy techs to attending physicians. And we need decision support tools that don’t just flag the interaction but offer immediate, actionable alternatives with dosing guidance. This isn’t just about avoiding harm-it’s about designing systems that make the safe choice the easy choice.
Brooke Evers
I’ve been a nurse for 22 years, and I’ve seen too many patients come in with GI bleeds because they thought ‘it’s just Advil’ and didn’t tell their doctor. I’ve held hands in the ER while someone’s INR was 8.5 and they were bleeding into their abdomen. This isn’t theoretical. It’s real. And it’s preventable. I wish every patient on warfarin could read this. Please, if you’re on this med, don’t be embarrassed to ask. Don’t assume it’s ‘just a painkiller.’ Your doctor isn’t mind-reading. Tell them everything-even the stuff you think is ‘too small’ to mention. You’re not being a burden. You’re saving your own life.
Nigel ntini
This is exactly the kind of clarity we need in patient education. The data is overwhelming, the alternatives are clear, and the risks are not speculative. What’s more concerning is how normalized this dangerous combination has become-not just among patients, but among prescribers. I’ve seen GPs in the UK still write NSAID prescriptions for anticoagulated patients without a second thought. It’s not negligence-it’s ignorance. And that’s why public awareness campaigns like this one matter. Let’s not wait for another tragedy to fix it. Share this. Talk about it. Make it impossible to ignore.