Imagine waking up one morning and your heart starts pounding like you’ve just run a marathon-even though you’re lying still. Your chest tightens. You can’t catch your breath. You think you’re having a heart attack. Then, out of nowhere, you feel like you’re losing control, or worse, that you’re about to die. This isn’t a dream. It’s a panic attack. And for about 4.7% of U.S. adults, this isn’t a one-time event. It’s a recurring reality.
What Exactly Is a Panic Attack?
A panic attack isn’t just feeling nervous. It’s a sudden, overwhelming surge of fear that hits like a wave, peaking within minutes. Symptoms include a racing heart (reported in 98% of cases), sweating, trembling, shortness of breath, dizziness, chest pain, nausea, and a terrifying sense that something catastrophic is happening-even when there’s no real danger. You might feel like you’re choking, going crazy, or dying. These aren’t exaggerations. They’re real physical reactions. Your body’s fight-or-flight system fires off without warning. Heart rates can spike past 120 beats per minute. Breathing becomes shallow and fast. Your muscles tense. Your mind races with worst-case scenarios. Most attacks last between 5 and 20 minutes. Some stretch to an hour, but they always fade. The problem isn’t the attack itself-it’s what happens after. Once you’ve had one, your brain starts scanning for the next one. You begin to dread the next episode. That’s when panic disorder takes root.How Panic Disorder Turns Into Agoraphobia
Panic disorder becomes more than just attacks when it starts controlling your life. That’s when agoraphobia shows up. It’s not just fear of open spaces. It’s fear of being trapped somewhere you can’t escape or where help isn’t available if you panic. People with agoraphobia avoid:- Public transportation (62% avoid buses or trains)
- Crowded places like malls or concerts (59%)
- Being outside alone (72%)
- Enclosed spaces like elevators or small rooms (48%)
- Open spaces like parking lots or bridges (55%)
Why Does This Happen? The Science Behind Panic
Panic disorder doesn’t come from being “weak” or “overreacting.” It’s rooted in biology, genetics, and learned patterns. Your brain’s alarm system-the amygdala-is overly sensitive. Brain scans show it activates 25% more in people with panic disorder when they see threatening images, even if the threat is fake. Your body’s stress chemicals, especially norepinephrine, are running too high. In 70% of cases, this system fires off without a trigger. Genetics play a role too. If a close family member has panic disorder, your risk increases by 30-48%. Twin studies confirm this isn’t just coincidence-it’s inherited. Life stress often sparks the first attack. 65% of people who develop panic disorder report a major life event-job loss, breakup, illness, or death-in the six months before their first attack. Then there’s anxiety sensitivity: the fear of fear itself. People with high anxiety sensitivity believe physical symptoms like a racing heart mean they’re about to collapse or die. They’re not wrong to feel that way-the symptoms are real. But their brain misreads them as life-threatening. This belief fuels the cycle.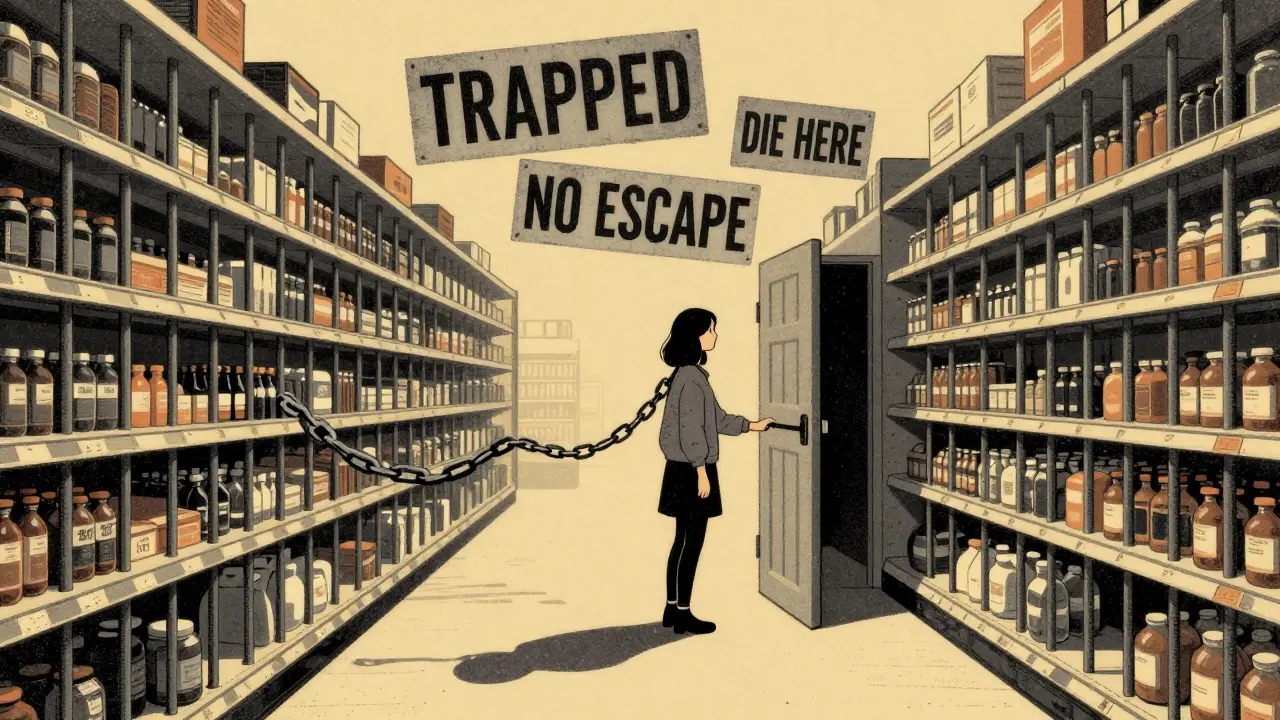
Effective Treatments: What Actually Works
The good news? Panic disorder is one of the most treatable anxiety disorders. And you don’t need to live in fear forever. The gold standard is cognitive behavioral therapy (CBT). Studies show 70-80% of people see major improvement after 12-15 weekly sessions. CBT doesn’t just calm you down-it rewires how you think about panic. Here’s how it works:- Cognitive restructuring: You learn to challenge thoughts like “My heart is racing-I’m having a heart attack.” Instead, you reframe it: “This is panic. My body is reacting to fear, not danger.”
- Interoceptive exposure: Your therapist guides you to safely recreate panic symptoms-spinning in a chair to feel dizzy, breathing through a straw to feel short of breath. You learn these sensations aren’t dangerous. They’re just uncomfortable.
- In vivo exposure: You slowly face avoided situations. Start with standing near a bus stop. Then ride one for two stops. Then five. Then a full route. Each step proves you can handle it.
Medication: When and How It Helps
Medication isn’t a cure, but it can be a bridge-especially when panic is severe or agoraphobia has taken hold. SSRIs like sertraline and paroxetine are first-line choices. They take 6-12 weeks to work, but 60-75% of people see improvement. Side effects? Nausea, fatigue, weight gain (about 40% of users report this), and emotional numbness. These often fade after a few weeks. Benzodiazepines like alprazolam work fast-within hours. But they’re risky. 30-40% of long-term users become dependent. They’re best for short-term use during crisis, not daily management. A newer option? d-cycloserine, a drug taken before therapy sessions. It helps your brain learn faster during exposure. One 2022 study showed it boosted CBT success by 28%. The most powerful approach? Combining CBT with SSRIs. People on both treatments have 85% remission rates-much higher than either alone.





10 comments
Alec Stewart Stewart
Man, this hit home. I had my first panic attack in a Walmart back in 2019. Thought I was dying. Turned out I just needed to breathe and stop fighting it. Now I do the straw breathing thing when I feel it coming. It’s wild how your body betrays you like that. 😅
Demetria Morris
It’s irresponsible to frame panic disorder as something that can be 'fixed' with therapy alone. Many people need medication. Some of us have tried CBT for years and still can’t leave the house. Don’t romanticize recovery like it’s just a mindset.
Geri Rogers
OMG YES!! 🙌 I’m a therapist and I’ve seen this over and over-CBT + SSRIs is the golden combo. One client went from hiding in her apartment for 18 months to hiking in the Rockies in 9 months. No magic, just science. And d-cycloserine? Game changer. If you’re stuck, don’t give up. You’re not broken-you’re just waiting for the right tools. 💪❤️
Samuel Bradway
I used to think panic attacks were just anxiety gone wild. Then my sister had one in front of me. She wasn’t dramatic. She was terrified. And honestly? The part about the brain blaming the place, not the panic-that clicked for me. I get it now. It’s not about being weak. It’s biology.
Justin Fauth
This is why America’s getting soft. Back in my day, we just sucked it up. No therapy, no apps, no excuses. You had a panic attack? Walk it off. Drink some water. Stop being a baby. We don’t need coddling-we need grit.
Lorena Druetta
It is of paramount importance to underscore that the efficacy of cognitive behavioral therapy, when administered with fidelity and under the supervision of a licensed clinician, yields statistically significant outcomes in the majority of cases. Furthermore, the integration of pharmacological intervention demonstrates a synergistic effect that cannot be overstated. One must approach this condition with both scientific rigor and compassionate accountability.
Zachary French
LMAO so this is what happens when you let therapists run the show. I had a panic attack once. Didn’t do CBT. Didn’t take pills. Just yelled at my brain like, "Dude, chill the F out." And guess what? It did. 🤷♂️ I’m basically a zen master now. Also, I’ve read 37 papers on COMT genes. You’re welcome.
Daz Leonheart
Hey, if you’re reading this and you’re struggling-you’ve already taken the hardest step: looking for answers. That’s courage. You don’t need to be fixed. You just need to keep showing up. One step. One breath. One day at a time. I believe in you. You’ve got this.
Coy Huffman
It’s funny how fear becomes a self-fulfilling prophecy. We’re afraid of panic, so we avoid everything, which makes panic stronger. But what if panic isn’t the enemy? What if it’s just a misfired alarm? Like a smoke detector going off because you burned toast. The alarm isn’t wrong-it’s just confused. Maybe the goal isn’t to silence it, but to teach it what’s real. 🤔
Amit Jain
As someone from India, I can say this: here, panic disorder is still hidden. People think it’s "ghost problem" or "weak mind." But the science here is same. CBT works. I’ve helped three patients with exposure therapy. One started by standing at bus stop. Now he travels alone. No magic. Just patience.