When someone says they’re ‘just trying to eat healthier,’ it’s easy to miss the warning signs. But for 1 in 10 people in the U.S., an eating disorder isn’t a phase-it’s a life-threatening illness that hides in plain sight. Anorexia nervosa, bulimia nervosa, and binge eating disorder aren’t about willpower or vanity. They’re complex mental illnesses with real physical consequences, and the treatments that work are backed by decades of research-not Instagram trends or quick-fix diets.
What Anorexia and Bulimia Really Look Like
Anorexia nervosa isn’t just about being thin. It’s a brain disorder where the fear of gaining weight overrides hunger signals. People with anorexia often have a body weight far below what’s medically safe, yet still see themselves as overweight. The mortality rate? Higher than almost any other mental illness. One in five people with anorexia dies within 20 years of diagnosis-not from starvation alone, but from heart failure, organ damage, or suicide.
Bulimia nervosa doesn’t always show on the scale. People with bulimia may be normal weight or even overweight. The cycle is hidden: binge eating followed by purging-vomiting, laxatives, excessive exercise. One in ten people with bulimia develops swollen cheeks from repeated vomiting, a sign doctors call ‘chipmunk cheeks.’ It’s not a choice. It’s a neurological response to restriction and shame.
Here’s the part most people get wrong: less than 6% of people with eating disorders are underweight by medical standards. That means most aren’t visibly sick. A teenager hiding food, an athlete skipping meals, a parent avoiding family dinners-these aren’t quirks. They’re red flags.
The Hidden Costs: Physical and Mental Damage
Eating disorders don’t just affect your mind. They break your body. Electrolyte imbalances from vomiting can trigger cardiac arrest. Bone density drops so fast in anorexia that a 17-year-old might have the bones of a 70-year-old. Stomach ulcers, kidney failure, dental erosion from stomach acid-these aren’t side effects. They’re direct results of the behaviors.
Mental health takes a hit too. Over 75% of people with bulimia also struggle with depression. Nearly a third of those with anorexia have attempted suicide. Substance abuse is common-half of all people with eating disorders misuse alcohol or drugs, often to numb emotional pain or suppress appetite. And the longer it goes untreated, the harder it becomes to recover.
One study found that people with eating disorders are 11 times more likely to attempt suicide than those without symptoms. The risk spikes when treatment is delayed. That’s why waiting six months for therapy isn’t just frustrating-it’s dangerous.
What Actually Works: Evidence-Based Care
Not all therapy is created equal. Talk therapy alone doesn’t cut it for anorexia or bulimia. The gold standard treatments are specific, structured, and proven.
For teens with anorexia, Family-Based Treatment (FBT) is the most effective approach. Parents take charge of meals-yes, even if the teen resists. They supervise eating, prevent purging, and help restore weight. After 12 months, 40-50% of teens recover fully with FBT. Compare that to individual therapy alone, where only 20-30% recover. FBT works because it treats the illness as a family issue, not just an individual one.
For bulimia and binge eating disorder, Enhanced Cognitive Behavioral Therapy (CBT-E) is the top choice. It’s not about ‘thinking positive.’ It’s about breaking the cycle: identifying triggers, replacing binge-purge rituals with coping skills, and rebuilding a healthy relationship with food. After 20 sessions, 60-70% of people stop bingeing and purging. The key? Starting early. If treatment begins within three years of symptoms, remission rates jump to 65%.
In 2023, the FDA approved lisdexamfetamine (Vyvanse) for binge eating disorder-the first medication ever approved for any eating disorder. In clinical trials, it cut binge episodes in half compared to placebo. It’s not a magic pill, but it’s a tool that works alongside therapy.

The Broken System: Why People Don’t Get Help
There are 30 million Americans living with eating disorders. But there are only about 1,200 specialized treatment beds nationwide. That’s less than 0.004% of people getting the care they need each year.
Insurance is the biggest barrier. In a 2022 survey, 68% of people reported at least one insurance denial for eating disorder treatment. Some got denied 10 times. One woman raised $78,000 on GoFundMe to pay for 90 days of residential care. Another waited 27 months for treatment after being diagnosed with a BMI of 14.5-critically low.
Even when care is approved, wait times are brutal. The guidelines say outpatient care should start within two weeks. In reality, the average wait is 68 days for outpatient and over four months for intensive programs. For a teenager spiraling into anorexia, those extra weeks can mean irreversible damage.
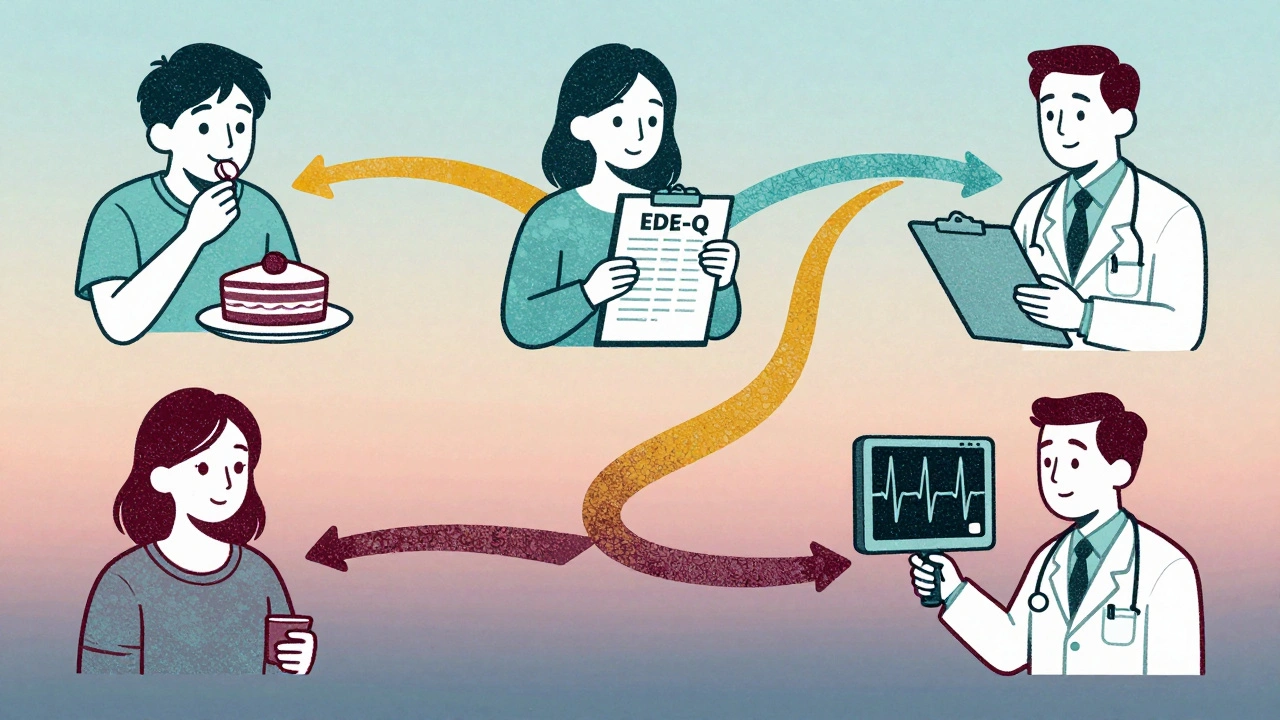
And it’s not just access-it’s quality. Only 38% of treatment centers meet basic standards for clinical documentation. Only 12% use standardized tools like the Eating Disorder Examination Questionnaire (EDE-Q) to track progress. That means some people are getting therapy that isn’t even being measured for effectiveness.
What Recovery Really Looks Like
Recovery isn’t about reaching a target weight. It’s about regaining control over your life. One woman on a recovery forum shared that after seven years of bulimia, 12 sessions of CBT-E reduced her binge-purge episodes from 14 times a week to just two. That’s not a miracle. That’s science.
Recovery means being able to eat a birthday cake without guilt. It means going on a hike without counting calories. It means sleeping through the night without checking your reflection. It means trusting your body again.
But recovery needs support. The most successful outcomes happen when treatment includes medical monitoring, nutritional counseling, and psychological therapy-all working together. A dietitian helps rebuild eating patterns. A therapist helps untangle the thoughts. A doctor watches for heart risks. No single piece works alone.
Where to Start If You or Someone You Love Is Struggling
If you’re worried about yourself or someone else, don’t wait. Here’s what to do now:
- See a doctor-even if you feel fine. Get bloodwork, an EKG, and a BMI check. Physical complications can develop fast.
- Find a specialist-look for providers trained in FBT or CBT-E. The Academy for Eating Disorders has a directory.
- Document everything-keep a log of eating behaviors, purging, and mood changes. This helps clinicians make faster decisions.
- Challenge insurance denials-file appeals. The Mental Health Parity Act requires equal coverage for mental and physical health. Many denials are illegal.
- Use digital tools-apps like Recovery Record help track meals and emotions. One study showed they improve outcomes by 32%.
You don’t need to be underweight to deserve help. You don’t need to be ‘bad enough’ to be treated. Eating disorders don’t care about your size-they care about your silence.
What’s Changing for the Better
There’s progress. The NIH is tracking 7,500 children from birth to find early signs of eating disorders. Telehealth is expanding access in rural areas. Military bases now screen for eating disorders because rates are 2.3 times higher among service members.
But the system is still failing too many. We need more beds. More trained therapists. More insurance accountability. More public awareness that this isn’t a ‘girl problem’-it affects men, nonbinary people, older adults, and children as young as eight.
By 2030, experts predict a 25% drop in deaths if we act now. But that won’t happen without funding, policy change, and people speaking up.








10 comments
Andrea DeWinter
Been working in eating disorder recovery for 12 years and I can’t tell you how many times I’ve seen someone dismissed because they weren’t ‘thin enough’
It’s insane how the system ignores the majority of cases because they don’t fit the stereotype
FBT works because it stops blaming the kid and starts empowering the family
And CBT-E isn’t just ‘thinking positive’-it’s rewiring the brain’s fear response to food
People don’t realize how much trauma is buried under the binge-purge cycle
Recovery isn’t about willpower-it’s about safety, structure, and feeling seen
I’ve had patients who couldn’t eat in front of anyone for years and now they’re cooking dinner with their siblings
It’s messy, it’s hard, but it’s possible
And yes, insurance denials are criminal
But you’re not alone if you’re fighting this-reach out, keep pushing, we’ve got your back
Nikhil Pattni
Yo I’m from India and let me tell you this is 100% real here too
People think eating disorders are a ‘western problem’ but nope
My cousin was bingeing and purging for 3 years and her family thought she was just ‘being dramatic’
They told her to ‘eat more roti’ and ‘stop being weak’
She finally got help after collapsing at college and the doc said her potassium was at 2.8
That’s life threatening
And yeah the waitlist here is like 18 months for any specialist
And guess what? The only clinic that does CBT-E charges $800 a session
Most families can’t afford that
But the real issue? No one talks about it
Men? They think it’s ‘for girls’
Older people? ‘Too old for this nonsense’
And kids? ‘Just going through a phase’
We need awareness, not judgment
And stop saying ‘just eat’
It’s not that simple bro
🥺
Elliot Barrett
This whole post is just performative wokeness.
People have been eating weird since cavemen.
Why is this suddenly a ‘life-threatening illness’?
Maybe if you stopped obsessing over food, you wouldn’t have problems with it.
My grandma survived the Depression eating boiled rice and lard-she didn’t need a therapist.
Just eat a damn burger and move on.
Andrea Petrov
Actually, I’ve been following the research and I think this whole narrative is being manipulated by Big Pharma and the therapy-industrial complex
Did you know Vyvanse was originally developed for ADHD?
And now it’s being pushed as a ‘solution’ for binge eating?
There’s a 2021 leaked email from a pharmaceutical exec saying ‘we need to rebrand eating disorders as pharmacologically treatable’
And don’t get me started on CBT-E-how many people have been sold on this ‘evidence-based’ lie?
It’s all just a way to monetize suffering
And the ‘family-based treatment’? That’s just control dressed up as care
Parents shouldn’t be policing their kids’ meals
It’s psychological abuse wrapped in a clinical label
Wake up people-this isn’t healing, it’s institutionalization
precious amzy
One must ask: if the body is a temple, then who is the priest? And if the temple is in ruins, is it the fault of the worshipper, or the architecture of the sacred space itself?
Is recovery a restoration of the self, or merely the reconditioning of the subject to conform to the norms of a pathological society?
The medicalization of hunger is a colonial project disguised as compassion.
One cannot heal what one has not first deconstructed.
Perhaps the real illness is the belief that food must be regulated at all.
And yet-how many have been sold this lie, and how many have been silenced by the clinical tongue?
Recovery, as it is currently conceived, is merely a rebranding of obedience.
Evelyn Pastrana
Okay but imagine being 14 and your mom makes you eat a cookie after school because ‘you need energy’ and you feel like you’re gonna throw up but you’re also terrified of being called ‘ungrateful’
That’s not ‘willpower’-that’s trauma
And yeah I’ve seen people with bulimia who are ‘normal weight’ and everyone says ‘you look fine’
But they’re crying in the bathroom after every meal
And no one asks why
And then there’s the guy who lost 40 pounds and got praised for ‘getting fit’
Meanwhile his heart’s about to give out
It’s messed up
But here’s the good part-people are starting to talk
And that’s how change happens
Not with perfect words
Just with real ones
And you’re not alone
Really
Arun Kumar Raut
My brother had anorexia when he was 19
He wasn’t skinny at first, people said he was just ‘into fitness’
Then he stopped talking, stopped sleeping, started running 10 miles a day
We didn’t know what to do
Found a therapist who used CBT-E and it changed everything
Not because she told him what to eat
But because she asked him why he felt he had to
He cried for the first time in a year that day
Now he’s working as a peer support counselor
And yes, insurance denied him 5 times
But we appealed and got through
Don’t give up
Help is out there
Even if it’s slow
Even if it’s hard
It’s worth it
Katherine Chan
I’m 38 and I just started recovery last year
Had binge eating disorder for 15 years
Never thought I deserved help because I wasn’t underweight
My doctor said ‘you’re not thin enough to care’
So I went private
Therapy + dietitian + Recovery Record app
Now I eat pizza on Sundays and don’t hate myself after
It’s not perfect
Some days I still spiral
But I know now it’s not about food
It’s about feeling safe in my own skin
And if you’re reading this and you’re struggling
Don’t wait for someone to validate your pain
You already deserve help
Just take one step
Then another
You’ve got this
Tim Tinh
Just wanted to say I’m a dude who struggled with ED and it’s so lonely
People think it’s a ‘girl thing’
But I was hiding food, skipping meals, doing 2 hour workouts just to feel ‘in control’
My dad told me ‘men don’t have eating disorders’
So I suffered in silence for 6 years
Finally found a male therapist who got it
CBT-E saved me
Now I coach other guys through it
It’s not weak to ask for help
It’s the bravest thing you can do
And yeah the system sucks
But you’re not broken
You’re just healing
And I see you
❤️
Carina M
The entire framework presented herein is predicated upon a reductive biomedical model that pathologizes normative human behaviors under the auspices of clinical authority.
One must interrogate the epistemological foundations of ‘evidence-based treatment’-a phrase that functions as a rhetorical shield for institutional hegemony.
The very notion of ‘recovery’ presupposes a pathological baseline, thereby reinforcing the normative tyranny of the idealized body.
Is not the pursuit of ‘normalcy’ the most insidious form of control?
And who, pray tell, defined the parameters of ‘health’?
Pharmaceutical corporations? Insurance actuaries?
The elevation of CBT-E to gold-standard status is less a triumph of science than a triumph of capital.
Recovery, as it is currently conceived, is merely the assimilation of the self into the machine.
One must ask: what is being healed-and at what cost to the soul?