When you’re taking blood pressure medication, what you eat can be just as important as the pill you swallow. Many people don’t realize that foods rich in potassium-like bananas, spinach, and sweet potatoes-can interact with common prescriptions in ways that are either helpful or dangerously risky. This isn’t about avoiding healthy foods. It’s about understanding how your body responds when potassium meets your meds.
Why Potassium Matters for Blood Pressure
Potassium doesn’t just help your muscles work. It’s a natural counterbalance to sodium, the mineral that often spikes blood pressure. When you get enough potassium, your kidneys flush out more sodium and relax your blood vessel walls. That’s why people who eat more potassium-rich foods tend to have lower blood pressure. Studies show a daily intake of 3,500 to 5,000 mg can drop systolic pressure by over 5 mm Hg-roughly the same effect as some first-line medications.The American Heart Association has backed this for years. But here’s the catch: if you’re on certain blood pressure drugs, your body holds onto potassium differently. That’s where things get tricky.
Which Blood Pressure Medications Raise Potassium Risk?
Not all blood pressure meds interact with potassium the same way. The big three to watch for are:- ACE inhibitors (like lisinopril, enalapril)
- ARBs (like losartan, valsartan)
- Potassium-sparing diuretics (like spironolactone, eplerenone)
These drugs work by blocking hormones that cause blood vessels to tighten and kidneys to hold onto salt. But they also reduce how much potassium your body gets rid of. So if you’re eating a lot of potassium-rich foods on top of these meds, your levels can creep up-sometimes without warning.
About 40% of people with high blood pressure are prescribed one of these medications. And in those patients, even small dietary changes can push potassium into dangerous territory.
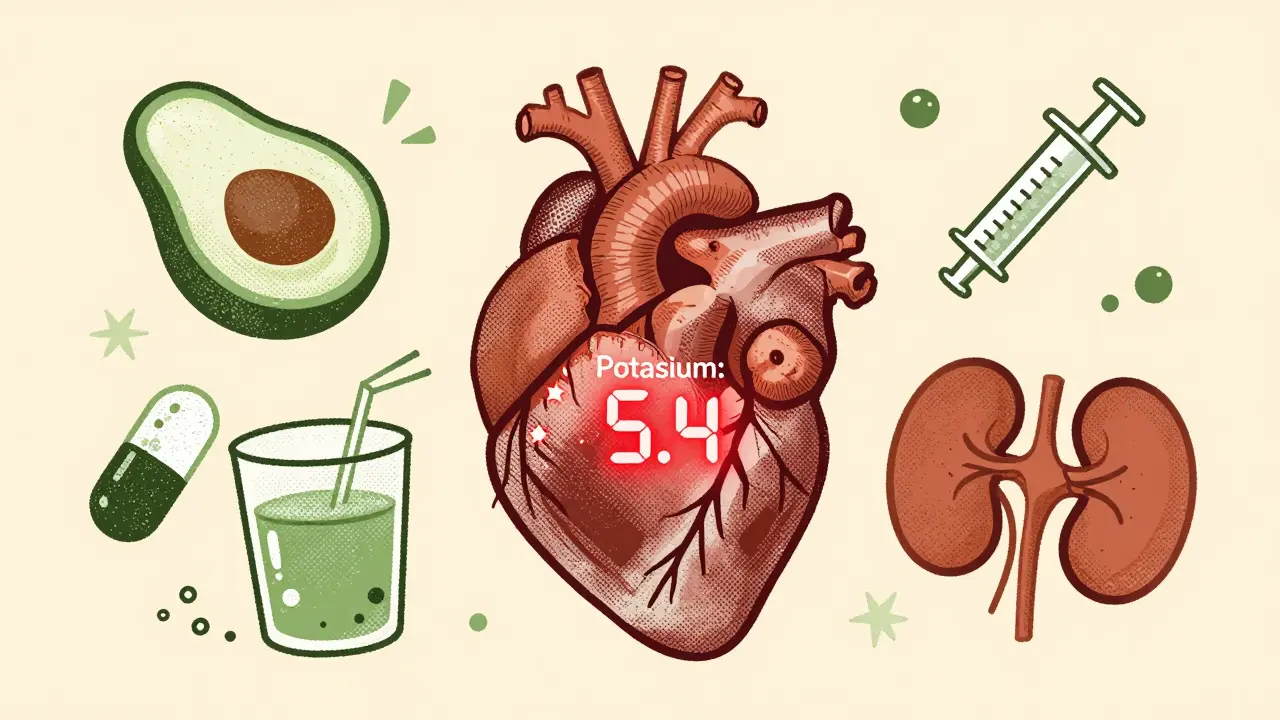
What Counts as Too Much Potassium?
Your blood potassium level should stay between 3.5 and 5.0 mmol/L. Anything above 5.0 is considered high. Above 6.0? That’s a medical emergency. At that level, your heart rhythm can go haywire, leading to cardiac arrest.Most people don’t get there from food alone. But when you combine high-potassium meals with ACE inhibitors or spironolactone, the risk climbs. One study found that 11.3% of elderly patients on ACE inhibitors developed dangerously high potassium levels after eating more fruits and vegetables. That’s not rare. It’s predictable.
And here’s something most don’t know: supplements are far riskier than food. A study of kidney disease patients given potassium chloride pills saw an 11% rate of hyperkalemia in just two weeks. But those eating the same amount of potassium through sweet potatoes and beans? Almost no spikes.
High-Potassium Foods You Should Track
You don’t have to give up these foods-but you do need to know how much you’re eating. Here’s a quick reference:- 1 medium banana: 422 mg
- 1 medium sweet potato: 542 mg
- 1 cup cooked spinach: 839 mg
- 1 avocado: 975 mg
- 1 cup coconut water: 600 mg
- 3 oz salmon: 534 mg
- 1 cup white beans: 829 mg
Some people think, “I’ll just eat one banana a day,” but if you’re on spironolactone and also snack on an avocado for lunch and drink coconut water after your workout? You’re hitting over 2,000 mg from food alone-on top of what your body holds onto because of your meds.
And don’t forget salt substitutes. Many “low-sodium” salts are actually potassium chloride. A quarter-teaspoon can pack 250-700 mg of potassium. If you’re on an ACE inhibitor, that’s like adding a daily potassium pill without realizing it.
When It’s Safe (and Even Helpful)
The good news? For most people with normal kidney function, eating more potassium while on ACE inhibitors or ARBs is safe. A 2016 study tracked patients over four weeks as they increased their potassium intake. Their blood levels stayed steady-between 4.1 and 4.3 mmol/L. No spikes. No problems.The key? Your kidneys have to be working well. If your eGFR (a measure of kidney function) is above 60 mL/min, your body can handle the extra potassium. But if your kidneys are already struggling, even small increases can be dangerous.
And here’s the real win: potassium works best when paired with lower sodium. If you’re eating more bananas and less processed food, your blood pressure drops more than if you just cut salt alone. The DASH diet, which emphasizes fruits, veggies, and whole grains, lowers systolic pressure by 8-14 mm Hg-better than most drugs.
What Real Patients Are Saying
Online forums are full of stories. One Reddit user, on spironolactone, said switching from three bananas a day to blueberries dropped their potassium from 5.4 to 4.8. Another patient on lisinopril started using the Cronometer app to track intake and found they were eating 4,000 mg a day without realizing it. After cutting back on spinach and beans, their levels stabilized.But not all stories are positive. A survey of 872 hypertension patients found 19% had symptoms like muscle weakness or heart fluttering after increasing potassium. Seven percent ended up in the ER. These aren’t outliers. They’re preventable.
What You Should Do
If you’re on a blood pressure med that affects potassium, here’s your action plan:- Get a baseline blood test. Ask your doctor for a serum potassium level before making any dietary changes.
- Wait 2-4 weeks. After changing your diet, get tested again. That’s how long it takes for levels to stabilize.
- Know your limits. If your potassium is already near 5.0, don’t add more high-potassium foods without talking to your doctor.
- Avoid potassium supplements. Unless prescribed, they’re unnecessary and risky.
- Use a food tracker. Apps like Cronometer or the National Kidney Foundation’s Potassium Counts app help you see what you’re really eating.
And if you’re unsure? Don’t guess. Talk to your pharmacist or a dietitian who specializes in kidney or heart health. A 45-minute consultation can save you a hospital trip.
The Bigger Picture
This isn’t just about avoiding danger. It’s about using food as medicine-wisely. The average American eats only 2,400 mg of potassium a day. The recommended amount is 4,700. That gap contributes to millions of preventable cases of high blood pressure.But if you’re on the right meds, you can close that gap safely. The FDA now requires potassium warnings on ACE inhibitor and ARB packaging. That’s progress. But it’s not enough. You need to know your numbers, your meds, and your meals.
There’s a new tool on the horizon: Omron’s HeartGuide smartwatch, launching in 2024, will monitor potassium trends in real time. But for now, the best tech you have is your awareness. Track your food. Know your labs. Talk to your doctor.
Potassium isn’t the enemy. But when it teams up with the wrong meds, it can become one. You don’t have to choose between healthy food and safe medicine. You just need to make the connection.
Can I still eat bananas if I’m on lisinopril?
Yes, but in moderation. One banana a day is usually fine if your kidney function is normal and your potassium levels are under 5.0 mmol/L. But if you’re eating multiple bananas daily, along with other high-potassium foods like spinach or sweet potatoes, you could be pushing your levels too high. Check your blood potassium every few weeks after changing your diet.
Are salt substitutes safe with blood pressure meds?
Not if you’re on ACE inhibitors, ARBs, or potassium-sparing diuretics. Most salt substitutes are made of potassium chloride. A quarter-teaspoon can add 250-700 mg of potassium to your daily intake. For someone on these meds, that’s enough to raise blood potassium into the dangerous range. Stick to regular salt in small amounts or use herbs and spices instead.
How often should I get my potassium checked?
If you’re starting a new potassium-rich diet or beginning an ACE inhibitor or ARB, get tested at baseline, then again at 2 and 4 weeks. After that, every 3-6 months is standard for most patients. If you have kidney disease or your levels have been high before, your doctor may want checks every 1-3 months.
What are the early signs of high potassium?
Early symptoms are subtle: muscle weakness, tingling in hands or feet, nausea, or an irregular heartbeat. Many people ignore them, thinking it’s just fatigue. But if you’re on a high-risk medication and notice these, get your potassium checked right away. Severe hyperkalemia can cause cardiac arrest without warning.
Should I take potassium supplements to lower my blood pressure?
No-unless your doctor specifically prescribes them. Most people get enough potassium from food. Supplements can cause dangerous spikes, especially if you have kidney issues or are on blood pressure meds. The risk isn’t worth it. Focus on whole foods like vegetables, beans, and fish instead.
Can I eat potatoes if I’m on spironolactone?
You can, but be careful. A medium baked potato has about 900 mg of potassium. If you’re eating potatoes daily, plus spinach, beans, and avocado, you’re likely exceeding safe limits. Try swapping some potatoes for lower-potassium options like cabbage, cauliflower, or apples. Your doctor can help you build a balanced plate that keeps your potassium in range.
Does cooking affect potassium levels in food?
Yes. Boiling vegetables like spinach or potatoes can reduce potassium by up to 50% because it leaches into the water. If you’re trying to lower your intake, boil instead of steam or bake. But don’t throw out the water-it’s full of nutrients. Just don’t drink it. If you want to keep potassium high, steam or roast instead.






11 comments
Anu radha
I never knew bananas could be dangerous with my blood pressure pills. I eat one every morning with my oatmeal. Guess I’m gonna switch to apples now. Thanks for the heads-up.
Jigar shah
The data on potassium and ACE inhibitors is solid, but the real issue is lack of patient education. Most people aren’t told to monitor their intake-they’re just handed a script and told to ‘eat healthy.’ That’s irresponsible.
Joe Bartlett
Brits have been eating potatoes and beans for centuries and we’re still standing. Maybe your meds are the problem, not the food.
Jody Patrick
Just stop eating all that fancy kale and avocado toast. Eat chicken and rice like normal people. Problem solved.
Anna Giakoumakatou
Oh wow, a blog post that doesn’t assume everyone’s a 23-year-old bio major with a $200 smartwatch. How quaint. I suppose the FDA warning label is the only thing keeping us from a potassium apocalypse.
BETH VON KAUFFMANN
Hyperkalemia risk stratification is heavily confounded by renal function, yet this piece conflates dietary potassium with supplement-induced spikes. The DASH diet’s efficacy is well-documented, but the 4,700 mg RDA assumes eGFR >60. Without context, this is dangerously reductive.
Raven C
I’ve been on spironolactone for three years… and I’ve never once thought to check my potassium. I’m a 52-year-old woman who eats spinach salads daily, drinks coconut water post-yoga, and uses ‘lite salt’ because I’m ‘trying to be healthy.’ I’m terrified. Thank you for this.
Donna Packard
It’s so nice to see a post that doesn’t scare people away from healthy foods. Just be mindful, get tested, and talk to your doctor. You’ve got this.
Patrick A. Ck. Trip
i just wanted to say thank you for this post. i wasnt aware that cooking veggies could lower potassium. i always boil mine. maybe i should try steaming? also, i think we need more public health info like this. thank you again.
Sam Clark
This is an excellent, balanced, and clinically sound overview. For patients on ACE inhibitors or ARBs with preserved renal function, dietary potassium is not only safe-it is therapeutic. The key is individualized monitoring and patient empowerment, not restriction. Well done.
Peter Ronai
Let me guess-you’re one of those people who thinks ‘natural’ means ‘safe.’ Potassium from food is just as dangerous as pills if your kidneys are sluggish. And you’re telling people to eat more spinach? That’s not wisdom. That’s negligence. People die from this. Don’t be that guy.