Drug Supply Chain: How Medications Get to You and Why It Matters
When you pick up a prescription, you’re holding the end result of a complex drug supply chain, the network of organizations, processes, and regulations that move medications from manufacturers to patients. Also known as pharmaceutical distribution system, it includes makers, shippers, wholesalers, pharmacies, and regulators—all working together to get the right drug to the right person at the right time. It’s not just about delivery. It’s about safety, cost, and trust.
Behind every pill is a factory. Some make brand-name drugs. Others make generic drugs, medications with the same active ingredients as brand-name versions but often at a fraction of the cost. Also known as authorized generics, they can come from the same factory as the brand, just without the fancy packaging. But not all generics are equal. Some have manufacturing defects—like uneven dosing, contamination, or pills that fall apart. These aren’t rare. And they directly affect whether your medicine works—or puts you at risk.
The pharmaceutical manufacturing, the process of producing medications under strict quality controls to meet FDA and global standards. Also known as drug production, it requires calibrated machines, clean rooms, and trained staff. One small error—a mislabeled batch, a broken thermometer, a skipped validation step—can ripple through the whole system. That’s why temperature control during drug distribution, the transport and storage of medications from factory to pharmacy. Also known as pharmaceutical logistics, it ensures drugs like insulin and vaccines don’t lose potency. matters. A shipment stuck in a hot truck can ruin a life-saving drug before it even reaches the pharmacy.
And it’s not just about science. Culture, laws, and money shape the chain too. In some countries, patients distrust generics because of color or packaging. In others, strict substitution rules keep prices low. Global policies on generic drugs, medications approved as equivalent to brand-name drugs and widely used to reduce healthcare costs. Also known as generic medications, they make treatment accessible to millions. determine who gets treated and who doesn’t. Even your local pharmacy’s supplier can affect what’s on the shelf—and whether it’s safe.
What you’ll find here aren’t abstract theories. These are real stories: a faulty generic that caused a crisis, a vaccine shipped in freezing temps that stayed potent, a patient confused by a pill that looked different but was supposed to be the same. You’ll learn how manufacturing defects happen, why some drugs cost less without being worse, and how a broken link in the chain can hurt someone you know. This isn’t just about how pills are made. It’s about how they get to you—and what you can do to protect yourself.
- Feb 19, 2026
- Posted by Cillian Osterfield
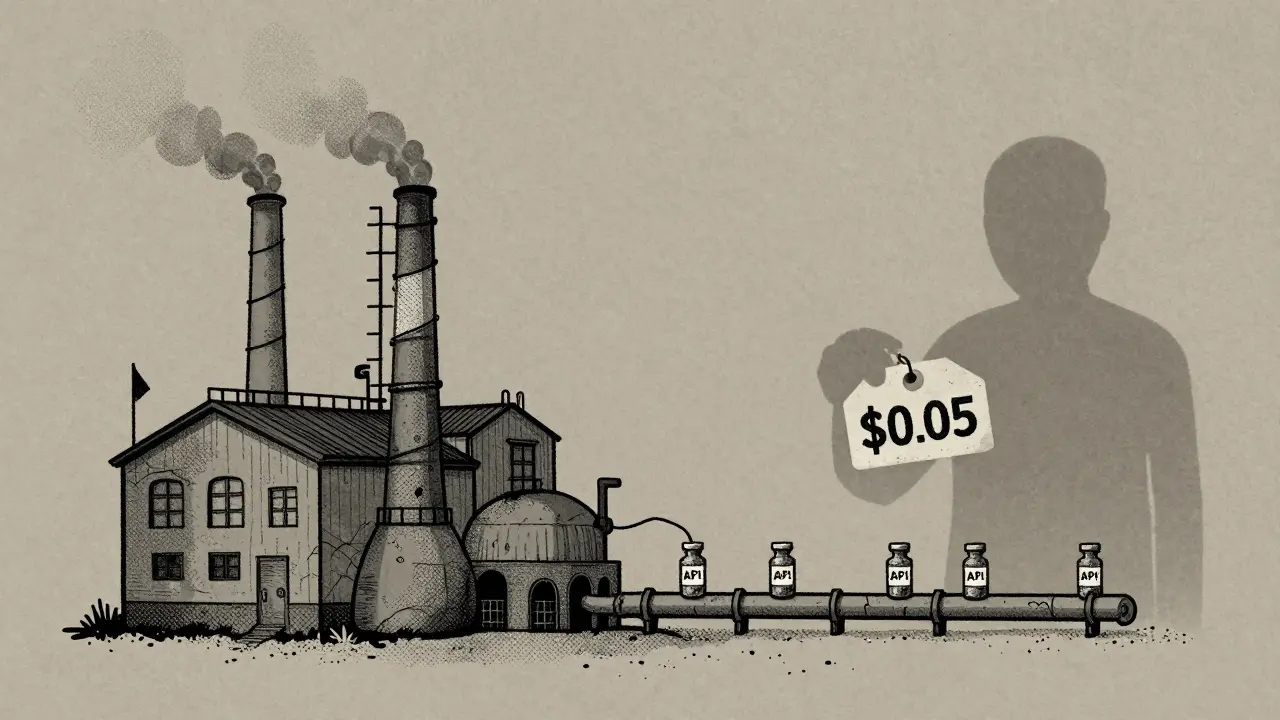
Causes of Generic Drug Shortages: Manufacturing and Supply Chain Issues
Generic drug shortages are caused by fragile manufacturing, overseas supply chains, and a pricing system that punishes reliability. Over 95% of shortages involve generics, and without structural change, they'll keep happening.

- Dec 1, 2025
- Posted by Cillian Osterfield
Government Response to Drug Shortages: Federal Actions in 2025
In 2025, the U.S. government is responding to record drug shortages with stockpiling, AI monitoring, and new laws-but critical gaps remain in manufacturing, enforcement, and economic incentives that keep shortages alive.
Categories
- Health and Wellness (72)
- Medications (69)
- Health and Medicine (28)
- Pharmacy Services (12)
- Mental Health (9)
- Health and Career (2)
- Medical Research (2)
- Business and Finance (2)
- Health Information (2)
Latest Posts
©2026 heydoctor.su. All rights reserved