Blood Thinner Travel Safety Assistant
Identify Your Blood Thinner Type
Personalized Travel Safety Guide
Travel Safety Checklist
- Talk to your doctor 4-6 weeks before departure
- Confirm medication allowed in your destination country
- Get extra pills (10+ days beyond trip length)
- Pack your yellow booklet (if on warfarin)
- Get a doctor's letter in English
- Set phone alarms for medication times
- Carry water bottle and plan hydration
- Know nearest hospital at your destination
- Avoid alcohol, herbs, and aspirin
- Don't travel within 4 weeks of a recent clot
Getting ready for a trip abroad? If you’re on blood thinners, your checklist needs more than just sunscreen and adapters. Skipping a dose, mixing meds with local food, or forgetting your paperwork could turn a vacation into a medical emergency. The good news? With the right planning, you can travel safely-even with anticoagulants. Millions do it every year. But it’s not about luck. It’s about knowing what to do before you leave, what to carry, and how to handle time zones, flights, and unfamiliar healthcare systems.
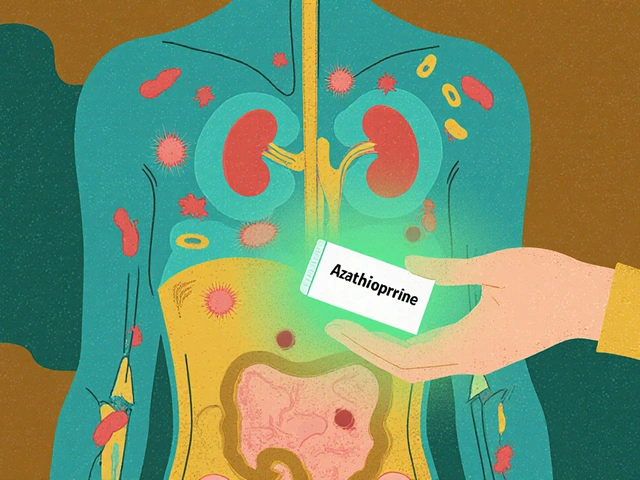
Know Which Blood Thinner You’re On
Not all blood thinners are the same. There are two main types: warfarin and DOACs. Warfarin has been around for decades. It’s cheap and effective, but it’s finicky. Your body’s response to warfarin changes based on what you eat, especially vitamin K-rich foods like kale, spinach, broccoli, and soy products. A sudden shift in diet-like eating more local greens in Japan or more olive oil in Italy-can throw your INR off. That’s why warfarin users need regular blood tests, usually every 4 to 6 weeks. If you’re on warfarin and traveling, you need to plan for those tests. Can you get one in Bangkok? In Lima? Maybe, but not always easily.DOACs-like apixaban, rivaroxaban, dabigatran, and edoxaban-are newer. They don’t need blood tests. They’re not as affected by food. And they start working faster, clear out quicker, and don’t require daily INR checks. For travelers, this makes them the preferred choice. The NIH’s 2018 review confirms DOACs are now the standard for treating blood clots, including those linked to long flights. If you’re still on warfarin, talk to your doctor before your trip. Switching to a DOAC might be an option. If you can’t switch, you’ll need a tighter plan.
Never Skip Your Dose-Even When Time Zones Change
Time zones mess with routines. You land in Tokyo, it’s 3 a.m. your body thinks it’s 7 p.m. Do you take your pill now? Or wait until your usual time? For DOACs, the rule is simple: take your pill at the same time each day, adjusted to your new local time. If you usually take it at 8 a.m. EST and you fly to Paris, switch to 8 a.m. Paris time the next day. Don’t double up. Don’t skip. Set a phone alarm. Use a pill organizer with alarms. Write it down on your calendar. This isn’t optional. Skipping even one dose increases your risk of a clot.Warfarin users have a harder time. If you’re on a 2-week trip and your next INR test was due in 10 days, but you’re now in a country without testing access, your doctor might give you extra doses of different strengths (like 1 mg, 2 mg, 5 mg tablets) to adjust if needed. Carry those. Never rely on buying warfarin abroad. Brand names and dosages vary. Your yellow booklet with INR history? That’s your lifeline. Always keep it on you-not in checked luggage. Medical staff overseas need to know your last INR, your target range, and your current dose. Without it, they’re flying blind.
Hydration Is Your Secret Weapon
Dehydration thickens your blood. That’s dangerous when you’re on a blood thinner. Airplanes are dry. Long car rides? You’re stuck. Sitting for hours? Your circulation slows. Add alcohol, coffee, or sugary drinks? That’s a triple threat. Alcohol can interact with warfarin. Sugary drinks cause inflammation. Coffee? It’s fine in moderation, but don’t use it to replace water.Drink water. Every hour on a flight. One liter per 10 hours is a good baseline. If you’re in a hot country, drink more. Carry a refillable bottle. Avoid soda, energy drinks, and excessive alcohol. UT Physicians and the National Blood Clot Alliance both stress this: hydration reduces clot risk more than most people realize. It’s not just about avoiding DVT-it’s about keeping your medication working properly.

Movement Matters-Even in a Seat
You’ve heard it before: “Get up and walk.” But it’s not just advice. It’s medical protocol. If you’re on a flight longer than six hours, you’re at higher risk for deep vein thrombosis (DVT), especially if you’ve had a clot before. The CDC and NIH both say sitting for long periods cuts blood flow in your legs. That’s when clots form.Walk the aisle every 2 to 3 hours. Do seated leg lifts. Point and flex your toes. Circle your ankles. Even small movements help. If you’re driving, stop every 2 hours. Walk for 5 minutes. Stretch your calves. Don’t wait until your legs feel stiff. By then, it’s too late. If you’ve had a recent clot-within the last 4 weeks-don’t travel at all. Healthline and other medical sources agree: the risk is too high. Wait. Let your body stabilize.
What to Pack-Beyond Your Pills
Your suitcase needs more than clothes. Here’s your must-pack list:- Original prescription bottles with your name and doctor’s info-never transfer pills to unlabeled containers.
- Extra supply-at least 10 days more than your trip length. Flights get delayed. Pharmacies abroad may not stock your exact brand.
- Yellow INR booklet (if on warfarin)-always in your carry-on.
- Doctor’s letter explaining your condition and meds. Include generic and brand names, dosage, and reason for use. Some countries require this for controlled substances.
- Emergency contact info-your doctor, pharmacy, and a family member. Save it on your phone and write it on paper.
- Reversal agent info (for DOACs)-know if your medication has an antidote. Idarucizumab for dabigatran. Andexanet alfa for apixaban and rivaroxaban. Write this down. Not everyone knows this.
What to Avoid-Even If It Seems Harmless
Some things seem safe. They’re not.- Aspirin without approval-don’t take it with your blood thinner unless your doctor says so. It increases bleeding risk.
- Herbal supplements-ginkgo, garlic, ginger, St. John’s wort, and fish oil can interfere with warfarin and DOACs. Even “natural” doesn’t mean safe.
- Scuba diving-if you’re on warfarin, a decompression injury could cause internal bleeding in your ears or spine. Divers Alert Network warns this is a real danger. DOACs are slightly safer, but still not recommended without specialist clearance.
- Traveling to areas with poor medical care-if you’re on warfarin and your destination lacks labs for INR testing, reconsider. DOACs are better here, but even they need access to emergency care if you bleed.
What to Do If Something Goes Wrong
You feel dizzy. Your gums bleed for no reason. Your leg swells. You have sudden chest pain. Don’t wait. Don’t assume it’s just jet lag. These could be signs of a clot or a bleed.Go to the nearest hospital. Show your yellow booklet or doctor’s letter. Say clearly: “I’m on a blood thinner.” If you’re in a non-English-speaking country, use a translation app or carry a card that says: “I take anticoagulant medication. I need immediate medical attention.”
Most hospitals worldwide can manage DVT or bleeding events. But speed matters. The sooner you get help, the less likely you’ll be stuck in a foreign hospital for days. UT Physicians says: “Getting help early has a low likelihood of interrupting your trip and may prevent a far worse problem.”
DOACs vs. Warfarin: The Traveler’s Choice
| Feature | Warfarin | DOACs (Apixaban, Rivaroxaban, Dabigatran, Edoxaban) |
|---|---|---|
| Requires blood tests? | Yes, every 4-6 weeks | No |
| Food interactions? | Yes, especially vitamin K | Minimal |
| Dosing flexibility across time zones? | Harder-needs INR adjustment | Easy-take at same local time |
| Emergency reversal available? | Vitamin K, fresh frozen plasma | Yes-idarucizumab (dabigatran), andexanet alfa (Xa inhibitors) |
| Best for long trips? | Only with planning and testing access | Yes-ideal for travelers |
If you’re choosing between the two, DOACs win for travel. They’re simpler, safer, and more predictable. But if you’re on warfarin and can’t switch, you’re not out of options-you just need to be more careful.
Final Checklist Before You Go
- ✅ Talk to your doctor 4-6 weeks before departure
- ✅ Confirm your medication is allowed in your destination country
- ✅ Get extra pills (10+ days beyond trip length)
- ✅ Pack your yellow booklet (if on warfarin)
- ✅ Get a doctor’s letter in English
- ✅ Set phone alarms for medication times
- ✅ Carry water bottle and plan hydration
- ✅ Know the nearest hospital at your destination
- ✅ Avoid alcohol, herbs, and aspirin
- ✅ If you’ve had a clot in the last 4 weeks-don’t travel
Traveling with blood thinners isn’t about fear. It’s about control. You’ve managed your condition every day. Now you’re just taking it on the road. Do the prep. Pack smart. Move often. Stay hydrated. And you’ll be fine. The world is still out there-and you’re still allowed to see it.
Can I fly with blood thinners?
Yes, you can fly with blood thinners. The key is to take your medication as prescribed, stay hydrated, move during the flight, and carry all your documents. Long flights increase clot risk, but proper precautions make flying safe. DOACs are especially well-suited for air travel because they don’t require blood tests and have fewer interactions.
What should I do if I miss a dose of my blood thinner?
If you miss a DOAC dose, take it as soon as you remember-if it’s within 6 hours of your usual time. If it’s more than 6 hours late, skip it and take your next dose at the regular time. Never double up. For warfarin, call your doctor immediately. Missing a dose can raise your INR unpredictably. Keep extra doses on hand so you can adjust if needed.
Can I drink alcohol while on blood thinners?
Moderate alcohol is usually okay, but avoid heavy drinking. Alcohol can increase bleeding risk and interfere with warfarin’s effectiveness. One drink a day is generally safe, but never use alcohol to replace water. Avoid binge drinking, especially in hot climates or during long flights.
Do I need to tell airport security I’m on blood thinners?
No, you don’t need to tell security. But keep your medications in original bottles and carry your doctor’s letter. If you’re questioned, show your prescription. Never pack pills in checked luggage. Carry them in your personal bag with your documents.
Is it safe to travel after having a blood clot?
Not for at least 4 weeks after diagnosis or treatment. Your body is still healing, and your risk of another clot is highest during this time. Wait until your doctor clears you. Even then, follow all travel precautions-hydration, movement, and medication discipline. Don’t rush.







12 comments
Edith Brederode
This is so helpful!! I’m on rivaroxaban and just booked my trip to Japan 🙌 I was stressing about the time zones but now I know to just switch to local time. Also, hydration tip? Lifesaver. I’ll be carrying my bottle everywhere. Thanks for this!! 💧✈️
clifford hoang
Let me guess - the government doesn’t want you to know that DOACs are just a pharmaceutical scam to replace warfarin with pricier pills. 🤡 They’ve been pushing this since 2010. The real reason? Insurance companies pay less for warfarin tests than they do for DOACs. And don’t get me started on ‘reversal agents’ - those are just profit engines. You’re being manipulated. Stick with warfarin. It’s been tested for 70 years. The rest? Lab experiments with fancy labels.
Also, ‘hydration reduces clot risk’? That’s what they told us about COVID. Drink water, avoid the vaccine. Same script. Wake up.
Arlene Mathison
YESSSS. I’ve been on apixaban for 3 years and traveled to 12 countries. This is 100% spot on. The biggest game-changer? The pill organizer with alarms. I used to forget and now I’m like a human robot. 🤖 Also, never skip movement - even if you’re on a 10-hour drive. I do ankle circles while waiting in line at museums. No one notices. I’m just the weird lady wiggling her toes in the Louvre. Worth it. 💪
Emily Leigh
Ugh. Another ‘travel with blood thinners’ guide. Like, who even reads this? You’re already paranoid enough to be on anticoagulants - now you need a 2000-word essay to go to Bali? 🙄 I took my pills, drank soda, didn’t move, and lived. The world doesn’t care. You’re not special. Stop overcomplicating everything.
Carolyn Rose Meszaros
Thank you for writing this. I’m on warfarin and was terrified to go to Mexico. But now I know to bring my yellow booklet and extra doses. I even printed out a doctor’s letter in Spanish! 😊 Also, the hydration tip? I’m going to start calling my water bottle ‘my clot-fighting BFF’. 💧❤️
Greg Robertson
I’ve been on warfarin for 8 years and traveled to Europe twice. The key? Talk to your doctor early. Mine helped me get a 6-week supply of extra tablets and even called the clinic in Prague ahead of time. They confirmed they could do INR tests. Also, don’t forget the sunscreen - warfarin makes your skin more sensitive. I got a nasty burn in Barcelona because I skipped that step. Lesson learned. 😅
Renee Stringer
It’s irresponsible to suggest people switch from warfarin to DOACs just for convenience. These are powerful drugs. You don’t just ‘trade’ them like you’d swap a phone plan. People with atrial fibrillation need stability, not marketing-driven trends. This article reads like a Pfizer ad. And ‘drink water’? That’s your medical advice? Really?
Courtney Carra
There’s a philosophical layer here. We treat blood thinners as problems to be managed, but they’re actually reminders of our fragility. Traveling while on them isn’t about logistics - it’s about accepting that we’re biological systems navigating chaotic worlds. The pill is a ritual. The water, a sacrament. The movement, a prayer. We’re not just avoiding clots - we’re negotiating with mortality, one step at a time.
Also, don’t forget to breathe.
Thomas Varner
My dad’s on warfarin and went to Thailand last year. He got his INR tested at a private hospital in Chiang Mai for $15. Seriously. I thought it’d be a nightmare - turned out it was easier than getting a coffee in NYC. Point is: don’t assume you can’t get care abroad. Do a quick Google search. Call the hotel concierge. Most places are way more prepared than we think.
Manoj Kumar Billigunta
This is very good advice. I am from India and I use apixaban. I travel often for work. I always carry my medicine in original bottle. I drink water every hour. I walk after every 2 hours. I tell my colleagues I am on blood thinner so they remind me if I forget. Simple things make big difference. You are not alone. Many people travel safely. Be calm. Be smart. You will be fine.
Nadia Watson
While I appreciate the effort behind this comprehensive guide, I must note that the orthographic inconsistencies - particularly the inconsistent use of serial commas and the occasional omission of articles - detract from the otherwise authoritative tone. Furthermore, the assertion that DOACs are ‘ideal for travelers’ requires qualification: while they reduce monitoring burden, their cost remains prohibitive for many, and access to reversal agents is not universal, even in developed nations. One must not conflate convenience with safety. Still, the hydration and movement recommendations are empirically sound and deserve emphasis.
thomas wall
How is it that we’ve reduced a life-saving medical protocol to a checklist of ‘pack this, drink that, move here’? This isn’t travel advice - it’s corporate wellness propaganda. You’re not a product. You’re not a ‘patient profile’. You’re a human being with a complex physiology, and you’re being sold a sanitized, algorithm-friendly version of survival. The real danger isn’t skipping a dose - it’s believing that compliance alone will keep you safe. The system doesn’t care if you live. It just wants you to buy the right pill.
And yes - I’ve been on warfarin for 14 years. I’ve flown through 47 countries. I’ve bled. I’ve clot. I’ve survived. Not because I followed a Reddit guide. Because I learned to listen to my body. And you should too.