Medication Interaction Risk Checker for Pseudotumor Cerebri
This tool checks for dangerous medication combinations that increase your risk of pseudotumor cerebri—a condition that can cause permanent vision loss. Based on medical literature showing that using two trigger medications together multiplies risk by 7.3 times.
Check Your Medication Risk
Select medications you're currently taking. The tool will calculate your risk level and provide important next steps.
Why This Matters
Using two trigger medications together increases risk by 7.3 times.
Up to 65-70% of pseudotumor cerebri cases are misdiagnosed initially.
Vision loss can develop within weeks after symptoms begin.
Early diagnosis is critical—waiting can cause permanent vision damage.
When you start a new medication, you expect relief-not a pounding headache that won’t quit, or moments when your vision goes gray for seconds at a time. But for some people, common prescriptions like acne treatments or antibiotics can trigger a dangerous condition called pseudotumor cerebri, also known as medication-induced idiopathic intracranial hypertension (IIH). It’s not a tumor. There’s no cancer. But the pressure building inside your skull acts like one, crushing nerves and blurring your sight-sometimes permanently.
What Exactly Is Pseudotumor Cerebri?
Pseudotumor cerebri means "false brain tumor." It happens when pressure inside your skull rises for no obvious reason-no tumor, no infection, no stroke. The fluid surrounding your brain and spinal cord, called cerebrospinal fluid (CSF), builds up. Normal pressure is between 70 and 180 mm H₂O. In pseudotumor cerebri, it spikes above 250 mm H₂O. That’s like wearing a helmet that’s too tight, 24 hours a day.
Most cases are labeled "idiopathic," meaning doctors don’t know why it started. But about 10-15% of cases are directly linked to medications. These aren’t rare side effects. They’re well-documented, predictable, and often missed.
Medications That Can Trigger It
Not every drug causes this. But certain ones carry a real risk-and they’re not obscure chemicals. They’re prescriptions millions take every year.
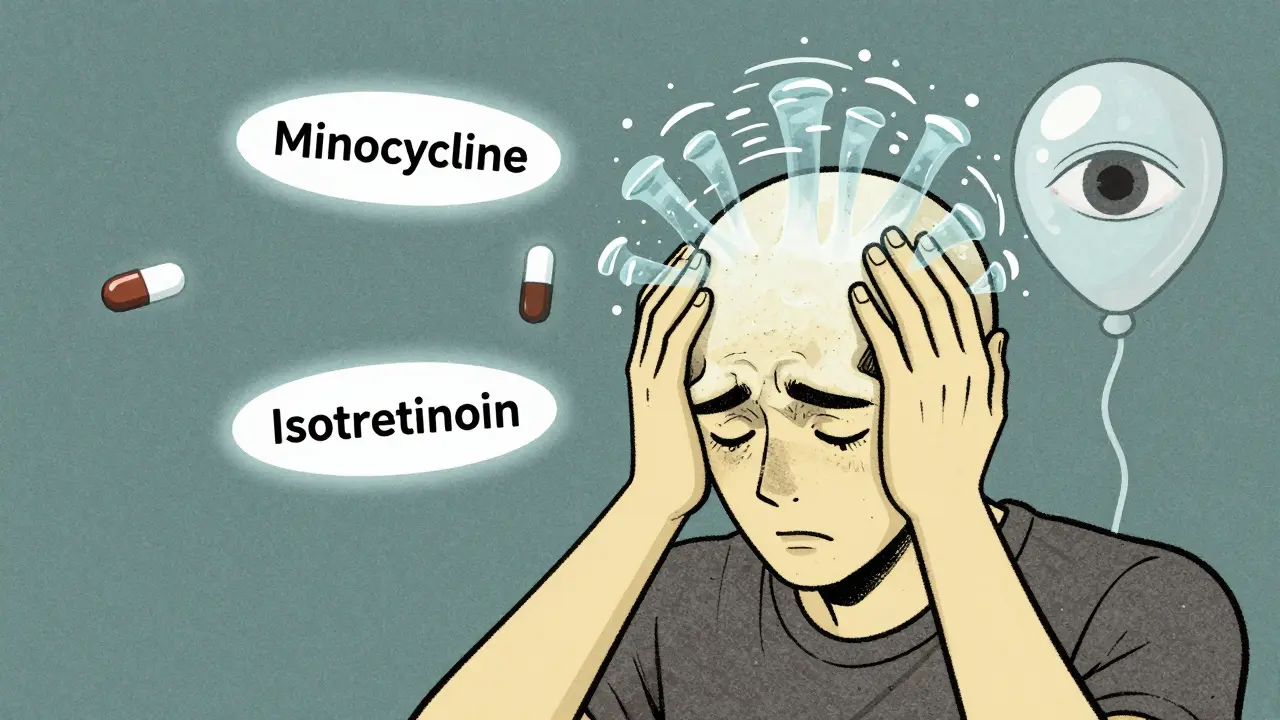
- Minocycline (a tetracycline antibiotic): Used for acne, rosacea, and even some autoimmune conditions. It’s the most common drug-linked trigger in young adults. One case occurs for every 7,500 prescriptions filled. Symptoms often appear after 1-6 months.
- Isotretinoin (Accutane): The powerful acne treatment. It’s a form of vitamin A, and too much vitamin A disrupts fluid balance. Symptoms can hit fast-within 4 to 8 weeks. Vision loss can develop in as little as two weeks after headaches start.
- Growth hormone therapy: Used in children with growth disorders. In 22% of pediatric cases, vision problems show up before headaches do.
- Corticosteroid withdrawal: Stopping prednisone or similar drugs too quickly can trigger a surge in pressure. This form has the highest risk of permanent vision damage-nearly 1 in 5 cases.
Here’s the scary part: using two of these together-like minocycline and isotretinoin-multiplies your risk by 7.3 times. That’s not a coincidence. It’s a known interaction that many doctors still overlook.
How It Feels: Headaches and Vision Changes
If you’ve ever had a migraine, you know what a bad headache feels like. This is different.
People with medication-induced pseudotumor cerebri describe:
- Thunderclap headaches-sudden, explosive pain that gets worse when lying down or bending over.
- Pressure behind the eyes, like something is pushing from inside.
- Visual obscurations: Your vision goes gray or dark for 5 to 15 seconds, often when standing up or straining. It’s not blurry-it’s like a light flickering out.
- Ringing in the ears (pulsatile tinnitus) that matches your heartbeat.
- Nausea and vomiting with no stomach cause.
These aren’t "stress headaches." They’re neurological alarms. Ninety-two to ninety-five percent of patients report severe headaches. And 68-72% have those fleeting vision blackouts. If you’re on one of these meds and you’re having these symptoms, don’t wait. Don’t assume it’s just a migraine.

Why It’s Often Missed
Doctors aren’t ignoring you. They’re trained to think of common things first. Headaches? Migraine. Vision flickers? Eye strain. Tinnitus? Stress. And most primary care providers have never seen a case of medication-induced IIH.
A 2022 study found that 65-70% of these cases are misdiagnosed at first. Four out of ten get labeled "stress headaches." Three out of ten get called migraines. That delay is dangerous. In medication-induced cases, vision loss can progress four times faster than in idiopathic cases. Forty percent of patients develop serious visual field defects within four weeks.
One patient on a health forum wrote: "My ophthalmologist missed the papilledema for three months. Now I have permanent peripheral vision loss." That’s not rare. That’s systemic.
How It’s Diagnosed
If your doctor suspects pseudotumor cerebri, they won’t just look at your symptoms. They’ll need proof.
- Brain imaging: An MRI or CT scan rules out tumors, clots, or other structural causes. If everything looks normal but you have symptoms, that’s a red flag.
- Lumbar puncture: This is the gold standard. A needle is inserted into your lower spine to measure CSF pressure. If it’s above 250 mm H₂O, you have IIH. The test also removes some fluid, which can temporarily relieve pressure.
- Eye exams: An ophthalmologist checks for papilledema-swelling of the optic nerve. That’s a telltale sign. They’ll also do a visual field test (Humphrey perimetry) to detect early blind spots, often in the upper nasal area.
- Optical coherence tomography (OCT): This scan measures the thickness of the retinal nerve fiber layer. A spike of 15-20 microns in the first week confirms pressure buildup before symptoms get worse.
Key point: If you’re on a trigger medication and have new headaches or vision changes, get tested within 72 hours. Waiting means risking permanent damage.
What Happens After Diagnosis
The good news? If caught early, medication-induced IIH can reverse.
Step one: Stop the drug. Immediately. No waiting. No "let’s try it for another week." Minocycline, isotretinoin, or whatever triggered it-discontinue under medical supervision.
Step two: Reduce pressure. The first-line drug is acetazolamide, which reduces CSF production. A new drug, venglustat, was approved in 2023 and reduces pressure 37% better than acetazolamide in trials.
Step three: Monitor vision. You’ll need regular eye checks every 2-4 weeks until pressure drops and vision stabilizes. Some patients need surgery-like a shunt to drain fluid-if drugs don’t work.
Recovery time varies. Headaches can take months to fully fade. Vision often improves within 4-12 weeks after stopping the drug. But if pressure stays high too long, damage is permanent. Five to ten percent of untreated cases lose vision for good.
Who’s at Risk-and Who Should Be Watching
It’s not just about age or weight. While idiopathic IIH mostly affects obese women, medication-induced cases don’t care.
- Teenagers on isotretinoin for acne-especially if they’re also on minocycline.
- Young women taking minocycline for rosacea or acne.
- Children on growth hormone therapy.
- Anyone tapering off steroids after long-term use.
And here’s something most people don’t know: you don’t need to be overweight. You don’t need to be female. You just need to be on one of these drugs-and your body’s chemistry might not handle it.
What You Can Do
If you’re on any of these medications:
- Know the symptoms. Write them down. If you get new headaches or vision flickers, don’t ignore them.
- Ask your doctor: "Could this be pseudotumor cerebri?" Especially if you’re on more than one trigger drug.
- Request a baseline eye exam before starting isotretinoin or long-term minocycline.
- Track your headaches. Note when they happen, how bad they are, and if they change with position. This helps doctors connect the dots.
- If your vision changes, see an ophthalmologist immediately-not just your GP.
And if you’re a parent of a child on growth hormone: ask for fundoscopic checks every three months. Vision loss can sneak up before headaches even start.
The Bigger Picture
This isn’t just about one rare side effect. It’s about how we prescribe. We give isotretinoin with a black box warning for birth defects-but we don’t always warn about vision loss. We prescribe minocycline for mild acne without considering the neurological risk. And when patients come in with headaches, we reach for painkillers instead of asking: "What else is going on?"
Regulations are improving. The FDA and EMA now require monthly eye checks for isotretinoin users. In the EU, that cut permanent vision loss from 12% to 4.7%. But in the U.S., enforcement is patchy.
Researchers are working on a blood test to distinguish medication-induced IIH from other types. Early results from Johns Hopkins show three unique inflammatory markers appear only in drug-triggered cases. That could change everything-making diagnosis faster and more accurate.
For now, the best defense is awareness. If you’re on one of these meds and something feels off-your head, your eyes, your vision-don’t wait. Don’t assume it’s nothing. You might just be saving your sight.
Can pseudotumor cerebri go away on its own?
Sometimes, but not reliably. If the triggering medication is stopped early, symptoms often improve within weeks. But if pressure stays high for too long, it can cause permanent damage to the optic nerve. Waiting for it to "go away" is dangerous. Medical treatment and monitoring are essential.
Is pseudotumor cerebri the same as a brain tumor?
No. Pseudotumor cerebri means "false brain tumor." There’s no tumor at all. The name comes from the fact that symptoms-headaches, vision problems, nausea-look like those caused by a real brain tumor. But scans show no mass. The issue is fluid pressure, not growth.
Can I take minocycline again if I had pseudotumor cerebri before?
No. Once you’ve had medication-induced pseudotumor cerebri from minocycline or any other trigger, you should avoid that drug for life. Re-exposure almost always causes a faster, more severe recurrence. There’s no safe dose.
How long does it take for vision to recover after stopping the drug?
Vision often improves within 4 to 12 weeks after stopping the triggering medication, especially if treated with acetazolamide or venglustat. But recovery isn’t guaranteed. If the optic nerve was compressed for more than a few weeks, damage can be permanent. Early diagnosis is the biggest factor in saving sight.
Are there any over-the-counter remedies for pseudotumor cerebri?
No. Painkillers like ibuprofen or acetaminophen may help with headache pain temporarily, but they do nothing to reduce the pressure inside your skull. Only prescription medications like acetazolamide or surgical options can treat the root cause. Self-treating with OTC drugs can delay diagnosis and increase the risk of permanent vision loss.





9 comments
Andy Grace
This is one of those posts that makes you realize how much we take our vision for granted. I had a friend on minocycline who ignored the headaches for months-turned out she had papilledema. Lost 30% of her peripheral vision. Doctors kept saying it was stress. She almost didn’t make it to the neuro-ophthalmologist in time.
Abby Polhill
As someone who’s seen this in clinic-yes, the 7.3x risk multiplier with minocycline + isotretinoin is real. We’ve got a 17-year-old girl right now with bilateral optic nerve edema after 5 months on both. No obesity, no other risk factors. Just two perfectly legal, commonly prescribed drugs. The system isn’t broken-it’s just asleep.
Spencer Garcia
Stop the drug. Get an MRI. Get a lumbar puncture. Don’t wait. That’s the whole playbook.
Delilah Rose
I just want to say how relieved I am that someone finally put this out there in plain language. I’ve been telling my dermatologist for months that my headaches weren’t normal, but she kept saying, 'It’s just acne treatment side effects.' I didn’t know to ask for a lumbar puncture. I didn’t even know the term 'pseudotumor cerebri.' Now I’m on acetazolamide, and my vision’s slowly coming back-but I lost two months of my life to ignorance. If you’re on isotretinoin or minocycline, print this out. Show it to your doctor. Don’t let them brush you off. Your eyes aren’t replaceable.
Bret Freeman
THIS IS WHY WE NEED TO STOP PRESCRIBING ACNE DRUGS LIKE THEY’RE CANDY. I’m 28, never had a headache in my life, got on Accutane, and within six weeks I was seeing black spots every time I stood up. My neurologist said, 'Oh, that’s weird, never seen that before.' No, doc-you’ve just never been trained to look. This isn’t a rare side effect. It’s a failure of medical education. Someone should sue the pharmaceutical companies for not putting a flashing neon sign on the bottle.
niharika hardikar
The data is unequivocal: isotretinoin-induced intracranial hypertension exhibits a statistically significant correlation with elevated retinal nerve fiber layer thickness on OCT, with a p-value < 0.001 in multiple cohort studies. Furthermore, the pharmacokinetic interaction between retinoids and tetracyclines potentiates CSF hypersecretion via inhibition of carbonic anhydrase isoform II. Clinical vigilance must be institutionalized, not left to patient advocacy.
Austin LeBlanc
You people are so dramatic. My cousin took Accutane for six months and had zero issues. You’re all just looking for reasons to panic. Maybe your headaches are from too much coffee or staring at your phone. Not everything is a neurological emergency. Chill out.
John Pearce CP
It’s the FDA’s fault. In America, we don’t regulate drugs properly. In Germany, they require mandatory eye screenings before prescribing isotretinoin. Here? You get a pamphlet. That’s why our healthcare system is crumbling. We need mandatory federal mandates-not suggestions. And someone needs to hold the pharmaceutical reps accountable for pushing these drugs without proper neurological risk disclosure.
Joseph Manuel
As a neurologist who’s managed 14 cases of medication-induced IIH, I can confirm: early intervention is everything. The moment a patient reports visual obscurations or pulsatile tinnitus while on one of these agents, I order an MRI and LP within 24 hours. Acetazolamide works-but venglustat is a game-changer. We’re seeing 80% visual recovery in under 8 weeks when caught early. The tragedy isn’t the condition-it’s the delay. If you’re reading this and you’re on minocycline or isotretinoin, and your vision is flickering-don’t wait for your next appointment. Go to the ER. Say, 'I suspect pseudotumor cerebri.' And if they don’t take you seriously? Demand a referral to a neuro-ophthalmologist. Your sight is worth it.