Understanding Osteodystrophy in Children
Osteodystrophy is a medical term that refers to a group of bone disorders affecting children. These conditions result from various factors, including hormonal imbalances, nutritional deficiencies, and genetic factors. In this article, we will explore the symptoms, diagnosis, and management of osteodystrophy in children, providing parents and caregivers with valuable information to help them care for their young ones.
Common Symptoms of Osteodystrophy in Children
Children with osteodystrophy may exhibit a range of symptoms, depending on the specific disorder they have. Some common signs to watch for include:
1. Slowed growth and development
Children with osteodystrophy may grow at a slower pace than their peers, leading to short stature. Additionally, they may experience delays in reaching developmental milestones, such as crawling, walking, and speaking, as their bones and muscles struggle to support their body weight.
2. Bone and joint pain
Osteodystrophy can cause pain in the bones and joints, making it difficult for children to move and participate in everyday activities. This pain may be chronic or intermittent and can worsen during periods of rapid growth, such as growth spurts.
3. Dental issues
Children with osteodystrophy may have weak teeth prone to cavities and other dental problems. In some cases, tooth development may be delayed, and teeth may be smaller than average or have an abnormal shape.
4. Skeletal deformities
Children with osteodystrophy may develop visible skeletal deformities, such as bowed legs, knock knees, or an abnormal curvature of the spine (scoliosis).
5. Muscle weakness and fatigue
Weak bones can lead to muscle weakness and fatigue, making it difficult for children to participate in physical activities and keep up with their peers.
Diagnosing Osteodystrophy in Children
If you suspect your child may have osteodystrophy, it's essential to consult with a healthcare professional for a proper diagnosis. The diagnostic process may involve the following steps:
1. Medical history and physical examination
Your child's doctor will begin by taking a thorough medical history, asking about any symptoms, family history of bone disorders, and other relevant information. They will also perform a physical examination to assess your child's growth, development, and overall health.
2. Laboratory tests
Various blood and urine tests may be ordered to check for hormonal imbalances, nutritional deficiencies, and other factors that could contribute to osteodystrophy.
3. Imaging studies
X-rays, MRI, and CT scans may be necessary to assess your child's bone structure, identify any deformities, and monitor the progression of the disorder.
4. Genetic testing
In some cases, genetic testing may be recommended to identify specific gene mutations associated with inherited forms of osteodystrophy.
Managing Osteodystrophy in Children
While there is no cure for osteodystrophy, there are several ways to manage the condition and improve your child's quality of life. Treatment options may include:
1. Nutritional supplementation
Ensuring your child receives adequate amounts of essential nutrients, such as calcium, vitamin D, and phosphorus, is crucial for promoting bone health. Your healthcare provider may recommend dietary changes or supplements to help meet these needs.
2. Hormone therapy
For children with hormonal imbalances, hormone replacement therapy (such as growth hormone or thyroid hormone) may be prescribed to help regulate bone growth and development.
3. Physical therapy
Physical therapy can help improve muscle strength, flexibility, and overall mobility in children with osteodystrophy. A trained therapist will work with your child to develop an individualized exercise program tailored to their specific needs.
4. Orthopedic interventions
In some cases, orthopedic interventions such as braces, shoe inserts, or even surgery may be necessary to correct skeletal deformities and improve your child's ability to move and function independently.
5. Pain management
Managing pain is a crucial aspect of treating osteodystrophy, as it can significantly impact your child's quality of life. Your healthcare provider may recommend over-the-counter pain relievers, prescription medications, or alternative therapies such as massage or acupuncture to help alleviate pain.
Supporting Your Child with Osteodystrophy
As a parent or caregiver, it's essential to provide support and encouragement to your child as they navigate life with osteodystrophy. Consider the following strategies:
1. Educate yourself and your family
Learn as much as you can about osteodystrophy and how it affects your child, and share this information with other family members and friends. This will help create a supportive environment for your child and ensure everyone understands their unique needs.
2. Foster a positive attitude
Encourage your child to focus on their abilities rather than their limitations, and help them develop coping strategies for dealing with pain and other challenges associated with osteodystrophy.
3. Advocate for your child
Work with your child's school, healthcare providers, and other important individuals in their life to ensure they receive the appropriate accommodations and support they need to succeed.
4. Connect with others
Join a support group or online community for parents of children with osteodystrophy. This can provide valuable information, resources, and emotional support as you navigate the journey together.
In conclusion, osteodystrophy in children can present various challenges, but with early diagnosis, proper management, and a strong support system, your child can lead a healthy and fulfilling life. By understanding the symptoms, diagnostic process, and available treatment options, you can be an informed advocate for your child and help them overcome the obstacles associated with this condition.





5 comments
Keith Bloom
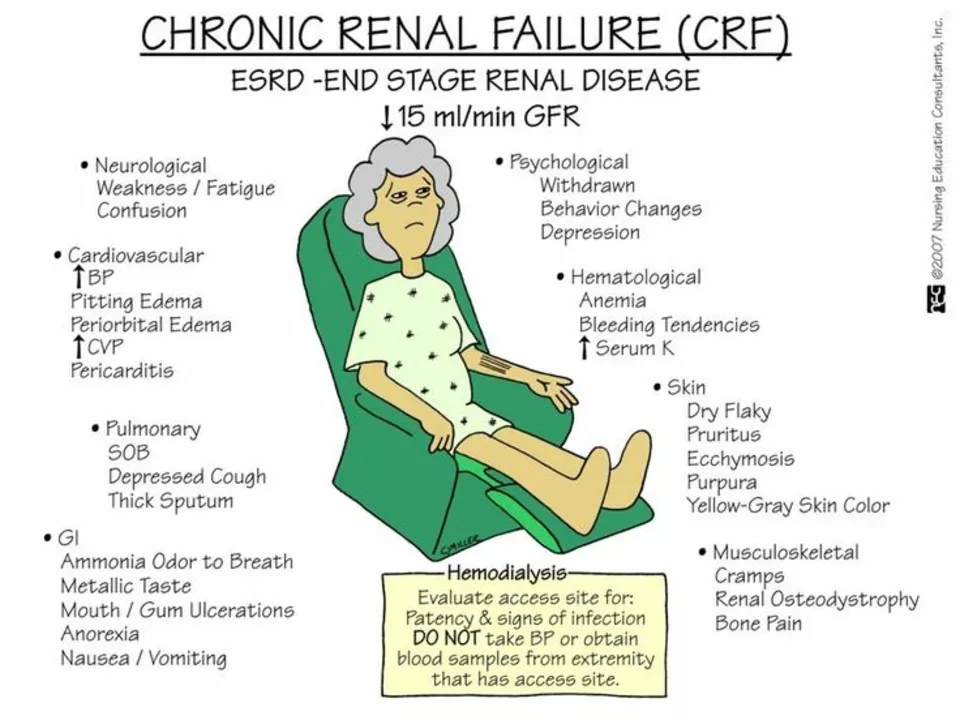
This article is textbook fluff. You say 'osteodystrophy' like it's one thing, but it's a whole damn spectrum-rickets, fibrous dysplasia, renal osteodystrophy... none of these are the same. Stop lumping them together and misleading parents. And no, vitamin D isn't a magic fix for genetic bone disorders.
Also, why are you linking to psychiatry journals? Did you copy-paste this from a grad student's thesis draft?
Ben Jackson
Big props to the author for breaking this down without drowning us in jargon. As a physio who works with pediatric bone cases daily, I can tell you: early intervention is EVERYTHING.
Parents, if your kid's walking late, has bowed legs, or complains of joint pain that doesn't go away after a week-don't wait for the next well-child visit. Push for a serum calcium, phosphate, ALP, and 25-OH-D panel.
And yes, PT helps. Not just for mobility, but for confidence. Kids with these conditions don't need pity-they need permission to move, to try, to fail safely. We've seen kids go from wheelchair to walking with braces. It's not miracle work. It's consistent, smart rehab.
Bhanu pratap
I am from India, and I have seen so many children suffering silently because families think 'bones are weak because of bad karma' or 'it will fix itself with time'.
This article is a light in the dark.
My nephew had severe rickets at age 3-bent legs, no teeth, could not stand. We found out too late. But once we started vitamin D3 and calcium, and took him for weekly physio, within 8 months he was running.
Do not wait. Do not ignore. Do not believe in home remedies over science.
God bless the doctors who fight for these children. And thank you for writing this. You gave hope to someone who thought there was none.
Meredith Poley
Let me guess-this was written by someone who’s never met a child with osteodystrophy but read three abstracts and a WebMD page.
‘Nutritional supplementation’ as a primary treatment? Sure. Just give a kid with XLH vitamin D and watch the pseudofractures multiply.
And ‘genetic testing may be recommended’? It’s not ‘may’-it’s mandatory if there’s family history or bilateral deformities. You’re doing a disservice by soft-pedaling the urgency.
Also, no one says ‘osteodystrophy’ anymore. It’s ‘renal osteodystrophy’, ‘rickets’, or ‘hypophosphatemic rickets’. Stop using the term like it’s a diagnosis and not a symptom complex.
Mathias Matengu Mabuta
While the general structure of this article is commendable from a pedagogical standpoint, the omission of the 2020 International Society for Clinical Densitometry (ISCD) guidelines regarding pediatric bone density interpretation is a critical scholarly oversight. Furthermore, the conflation of secondary osteodystrophy with primary genetic disorders such as osteogenesis imperfecta type IIA constitutes a fundamental diagnostic error that may lead to inappropriate clinical management. The references to psychiatric literature, while perhaps intended to contextualize psychosocial outcomes, are methodologically irrelevant to the pathophysiological framework being presented.
Moreover, the suggestion of acupuncture as a viable modality for pain management in pediatric bone disorders lacks empirical support in peer-reviewed, double-blind, randomized controlled trials as per the Cochrane Collaboration’s 2022 meta-analysis.
As a clinician-scientist with over 17 years in pediatric endocrinology, I must formally request that this article be retracted and revised in accordance with current evidence-based standards.