When you’re diagnosed with lupus, especially systemic lupus erythematosus (SLE), the goal isn’t just to manage symptoms-it’s to stop your immune system from attacking your own body. That’s where azathioprine is an immunosuppressant drug used to reduce immune system activity in autoimmune conditions like lupus. Also known as Imuran, it’s been a backbone of lupus treatment for over 50 years, even as newer drugs have come onto the scene.
Why Azathioprine Is Still Used Today
Many people assume that if a drug is old, it’s outdated. But azathioprine isn’t just hanging around because it’s cheap-it’s still widely prescribed because it works reliably. A 2023 study in the Journal of Autoimmunity tracked over 1,200 lupus patients on azathioprine for five years. Nearly 68% achieved sustained disease control without needing high-dose steroids. That’s a big deal. Steroids like prednisone help fast, but they cause weight gain, bone loss, diabetes, and mood swings over time. Azathioprine lets doctors lower those doses, reducing long-term damage.
It’s not a quick fix. It takes 3 to 6 months to reach full effect. That’s why it’s often started alongside a short-term steroid burst. Think of azathioprine as the slow, steady hand that keeps the fire under control after the initial flame is doused.
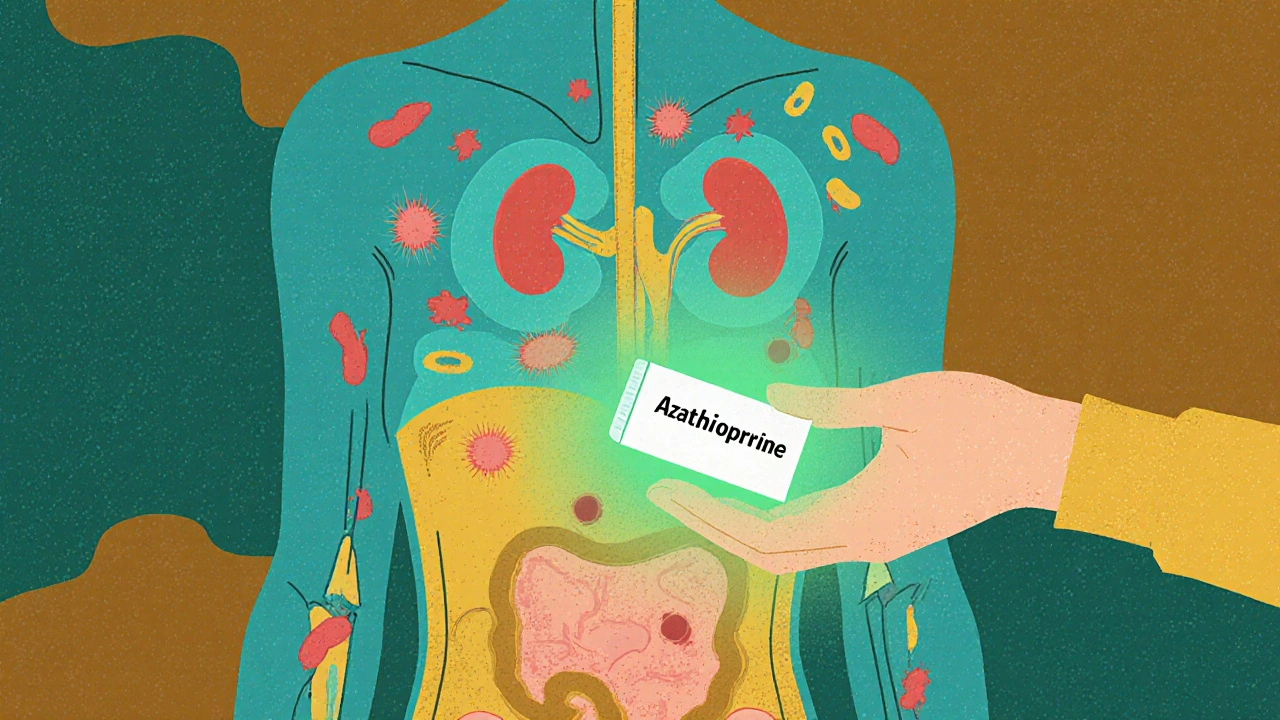
How Azathioprine Actually Works
Azathioprine doesn’t shut down your immune system completely. It targets specific white blood cells-mainly T and B lymphocytes-that go rogue in lupus. These cells normally protect you from viruses and bacteria. In lupus, they misfire and start attacking your skin, joints, kidneys, and even your brain.
Once you take azathioprine, your body converts it into 6-mercaptopurine (6-MP). This compound interferes with DNA building blocks, which stops those overactive immune cells from multiplying. Less active immune cells = less inflammation = fewer flares.
It’s a targeted approach. Unlike broad immunosuppressants that wipe out entire immune populations, azathioprine slows down the troublemakers without leaving you defenseless against common infections. That’s why many patients stay on it for years-even decades-without major complications.
Who Gets Prescribed Azathioprine
Not every lupus patient needs it. Doctors usually recommend azathioprine when:
- Your symptoms are moderate to severe-like kidney inflammation (lupus nephritis), serious rashes, or ongoing joint pain.
- You’ve had flare-ups despite using hydroxychloroquine (Plaquenil), which is often the first-line drug.
- You can’t tolerate steroids or need to cut back on them.
- You’re planning a pregnancy. Azathioprine is one of the safest immunosuppressants during pregnancy, unlike mycophenolate, which can cause birth defects.
It’s especially common in patients with kidney involvement. The 2021 European League Against Rheumatism (EULAR) guidelines list azathioprine as a preferred maintenance drug after initial treatment for lupus nephritis. That’s because it reduces the risk of kidney failure by about 40% over 10 years compared to no maintenance therapy.
Side Effects and Risks
No drug is without trade-offs. Azathioprine’s most common side effects show up early:
- Nausea and vomiting (affects about 30% of users, usually in the first month)
- Loss of appetite
- Mild fatigue
- Increased risk of infections, especially upper respiratory ones
More serious risks are rare but serious:
- Low white blood cell count (leukopenia)-this is why monthly blood tests are mandatory for the first 6 months.
- Liver enzyme changes-usually temporary, but monitored closely.
- Very rare: increased risk of lymphoma or skin cancer over long-term use (less than 1 in 1,000 patients over 10 years).
One key thing: your body’s ability to process azathioprine depends on an enzyme called TPMT. About 1 in 300 people have a genetic variant that makes them extremely sensitive to the drug. If you’re one of them, even a standard dose can cause life-threatening bone marrow suppression. That’s why many clinics now test for TPMT levels before starting treatment. If your levels are low, your doctor will cut the dose by 70-90% or switch you to another drug.
Azathioprine vs. Other Lupus Drugs
It’s not the only option. Here’s how it stacks up:
| Drug | Time to Effect | Common Side Effects | Pregnancy Safety | Monitoring Required |
|---|---|---|---|---|
| Azathioprine | 3-6 months | Nausea, low WBC, liver changes | Safe | Monthly blood tests (first 6 months) |
| Mycophenolate mofetil | 2-4 months | Diarrhea, infections, GI upset | Not safe-causes birth defects | Monthly blood tests |
| Methotrexate | 6-8 weeks | Liver toxicity, mouth sores, lung issues | Not safe | Monthly liver and blood tests |
| Belimumab (Benlysta) | 3-6 months | Headache, injection site reactions, depression | Probably safe-limited data | Every 4 weeks (infusion) |
Belimumab is newer and targets a specific protein (BLyS) involved in lupus, but it costs over $30,000 a year. Azathioprine? Around $20-$50 a month in most countries. That’s why it’s still the go-to for many, especially where healthcare access is limited.
What Happens If You Stop Taking It
Some patients feel better after a year or two and wonder if they can quit. Stopping azathioprine too soon is one of the biggest mistakes in lupus care. Studies show that patients who discontinue it before 2-3 years of stable disease have a 60-70% chance of relapse within 12 months. Even if you’ve been in remission for 5 years, doctors usually recommend staying on it unless you’re planning pregnancy or have serious side effects.
If you do stop, it’s done slowly-over 3 to 6 months-and only under close supervision. Your doctor will monitor your blood work and symptoms closely during the taper.

Real-Life Experience: What Patients Say
Emma, 34, from Auckland, was diagnosed with lupus nephritis in 2022. She started on high-dose steroids and azathioprine. "The nausea was awful at first. I thought I’d never make it through the first month. But after three months, my energy came back. My kidney numbers improved. Now I’m on a low dose. I’ve been off steroids for over a year. I can run with my kids again. That’s worth the side effects."
Not everyone has the same story. Some can’t tolerate it. Others find it doesn’t fully control their symptoms. But for many, it’s the difference between living with constant pain and living with control.
What to Do If Azathioprine Doesn’t Work
If after 6 months you’re still having flares, your doctor will likely adjust your treatment. Options include:
- Increasing the azathioprine dose (if your TPMT levels allow)
- Switching to mycophenolate mofetil
- Adding belimumab or rituximab
- Trial of low-dose cyclophosphamide (for severe kidney or nervous system involvement)
There’s no one-size-fits-all. Lupus is too unpredictable. That’s why treatment is personalized-based on your organs affected, your response, your lifestyle, and your goals.
Final Thoughts
Azathioprine isn’t glamorous. It doesn’t have flashy ads or viral TikTok videos. But for tens of thousands of lupus patients, it’s the quiet hero that keeps them out of the hospital, off steroids, and living full lives. It’s not perfect. It requires patience, regular blood tests, and honesty with your doctor. But when used right, it’s one of the most reliable tools we have.
If you’re on azathioprine, don’t skip your blood work. Don’t stop without talking to your doctor. And if you’re just starting, give it time. It doesn’t work overnight-but it works long-term.
How long does it take for azathioprine to start working for lupus?
Azathioprine typically takes 3 to 6 months to reach its full effect in lupus patients. During this time, symptoms like joint pain, fatigue, and skin rashes may improve gradually. Doctors often prescribe a short-term steroid like prednisone alongside azathioprine to control symptoms while the drug builds up in your system.
Is azathioprine safe during pregnancy?
Yes, azathioprine is considered one of the safest immunosuppressants to use during pregnancy. Unlike mycophenolate or cyclophosphamide, which are known to cause birth defects, azathioprine has been used for decades in pregnant lupus patients with no significant increase in fetal abnormalities. Many women continue taking it throughout pregnancy to prevent disease flares that could harm both mother and baby.
Do I need blood tests while taking azathioprine?
Yes, regular blood tests are essential. You’ll need them monthly for the first 6 months to check your white blood cell count, liver enzymes, and platelets. After that, tests may drop to every 2-3 months if your levels stay stable. This monitoring helps catch low blood cell counts early, which can be dangerous if left unchecked.
Can azathioprine cause cancer?
Long-term use of azathioprine slightly increases the risk of certain cancers, especially lymphoma and skin cancer. However, the risk is very low-less than 1 in 1,000 patients over 10 years. The benefit of controlling lupus, which itself increases cancer risk, usually outweighs this small risk. Using sunscreen and avoiding excessive sun exposure is strongly recommended.
What happens if I miss a dose of azathioprine?
If you miss a single dose, take it as soon as you remember that day. If it’s already the next day, skip the missed dose and return to your regular schedule. Never double up to make up for a missed dose. Missing doses occasionally won’t cause immediate harm, but consistent missed doses can lead to disease flares over time.
Is there a generic version of azathioprine?
Yes, azathioprine is available as a generic drug. It’s sold under the name azathioprine or sometimes as Imuran (the brand name). Generic versions are widely available and cost significantly less-often under $50 a month in many countries. They are bioequivalent to the brand-name version and are just as effective.
If you’re living with lupus, managing your treatment isn’t just about taking pills-it’s about understanding how each piece fits into your long-term health. Azathioprine may not be flashy, but for many, it’s the quiet, steady force that keeps the disease at bay.






11 comments
Erin Corcoran
Just started azathioprine last month and honestly? The nausea was brutal 😩 But I stuck with it, and at month 3, my joints stopped screaming. Still get tired, but I’m walking my dog again 🐶✨ Thanks for this guide-so much clearer than my rheum doc’s 3-minute spiel!
shivam mishra
As a pharmacist in Delhi, I’ve seen azathioprine save lives in resource-limited settings. Belimumab? Beautiful drug-but $30k/year is a fantasy for most Indian patients. Azathioprine’s $20/month generic? That’s equity in medicine. TPMT testing isn’t always available here, but we still use it-carefully, with weekly CBCs. It’s not glamorous, but it’s functional.
Scott Dill
Guys. I was skeptical. I thought this was just some old-school drug they gave you because they didn’t care. But after 8 months? My ANA levels dropped, my fatigue vanished, and I didn’t gain 20 pounds like I did on prednisone. I’m not a doctor, but I swear-this stuff is the quiet MVP of lupus care. Don’t quit before the 6-month mark. Trust the grind.
Arrieta Larsen
I’ve been on azathioprine for 11 years. No flares. No hospitalizations. Just monthly blood draws and a lot of coffee. It’s not perfect, but it’s mine. I don’t post about it much-lupus isn’t a TikTok trend-but this post made me feel seen. Thank you.
Mike Gordon
Azathioprine works. It’s cheap. It’s been around since the 60s. People forget that longevity isn’t a bug-it’s a feature. New drugs get hype. Old drugs get ignored. But if it’s still in the guidelines after 50 years? It’s doing something right. Also-TPMT testing should be mandatory everywhere. Not optional. Mandatory.
Kathy Pilkinton
So let me get this straight-you’re telling me we’re still using a 1960s drug because it’s cheap? And we’re calling that progress? Meanwhile, people in Europe are getting biologics on day one. This isn’t medicine. It’s triage. And it’s embarrassing.
Holly Dorger
My sister has lupus and has been on azathioprine for 7 years. She’s had two pregnancies while on it-both healthy babies. No birth defects. No flares. She’s now a nurse and tells every new patient: give it time. It’s slow. But it’s real. And honestly? It’s the only thing that lets her be a mom without being sick all the time. This post nailed it.
Amanda Nicolson
I remember the first time I felt like myself again after starting azathioprine. It was a Tuesday. I made pancakes. I didn’t nap after. I didn’t cry because my knees hurt. I just… stood there. Holding a spatula. And I thought: wow. I’m alive. Not surviving. Not just getting by. ALIVE. And it took six months. Six months of nausea, of fear, of wondering if I’d ever feel normal. But I did. And now? I’m running marathons. Not because I’m strong. Because this dumb little pill gave me back my life.
Jackson Olsen
My doc told me to wait 6 months. I thought he was lying. Turns out he wasn’t. Now I’m on low dose. No steroids. No hospital. Just me and my blood tests. Still take it. Still alive. Still here.
Penny Clark
Just wanted to say thank you for mentioning TPMT testing!! My cousin almost died because they didn’t test her and she got full bone marrow suppression. Now every clinic I go to checks it first. Please, if you’re starting this-ask for the test. It’s simple. It’s cheap. It could save your life 💙
Niki Tiki
Why are we still giving out 60s drugs like it’s 1972? We have better options. This is why America’s healthcare is broken. You get a $20 pill while rich people get $30k biologics. It’s not science-it’s classism. And it’s disgusting.