FDA shortages: Why drug supply gaps happen and what you can do
When the FDA shortages, temporary or prolonged gaps in the availability of essential medications approved by the U.S. Food and Drug Administration. Also known as drug shortages, these aren’t just inconveniences—they can delay treatments, force risky substitutions, or leave patients without life-saving drugs. This isn’t a rare glitch. Over 300 drugs have faced shortages in the last five years, from antibiotics to insulin, chemotherapy agents to simple pain relievers. The problem isn’t one thing—it’s a chain of failures: factories shut down for inspections, raw materials get stuck at borders, or a single plant makes 80% of a drug and then has a quality issue.
Behind every shortage is a generic drug, a cheaper version of a brand-name medication that must meet the same FDA standards for safety and effectiveness. Also known as off-patent medications, these make up 90% of prescriptions in the U.S. But they’re also the most vulnerable. Manufacturers often operate on razor-thin margins, so when one company faces a production hiccup, there’s no backup. And because many generics come from just one or two overseas facilities, a single factory closure in India or China can ripple across the entire country. Even pharmaceutical supply chain, the network of suppliers, manufacturers, distributors, and regulators that move drugs from labs to pharmacies. Also known as drug distribution system, it’s built for efficiency, not resilience. When a storm hits, or a regulator flags a batch, the whole system slows down.
What does this mean for you? If you take a daily pill for blood pressure, thyroid, or diabetes, you might suddenly find your pharmacy out of stock. Your doctor might switch you to another brand—or worse, a different drug entirely. Some patients have waited weeks for insulin or antibiotics. Others have had to split pills or skip doses. These aren’t theoretical risks. They’re real, documented events that happen every month. The FDA tracks these shortages, but their public list doesn’t always tell you when a replacement will arrive—or if it’s safe for your condition.
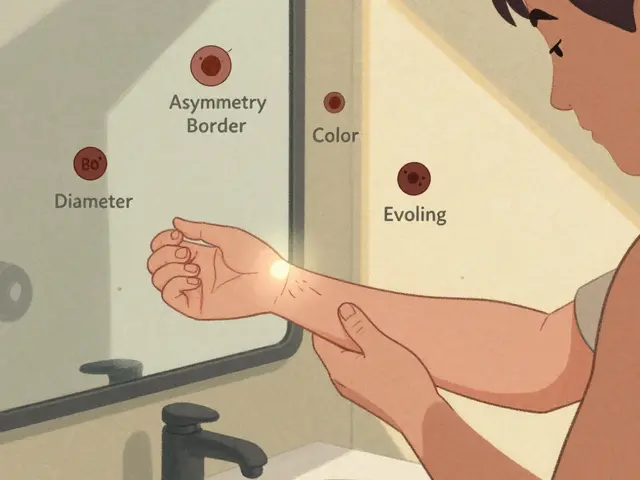
There’s no magic fix, but awareness helps. Knowing that shortages often hit generics first means you can ask your pharmacist: "Is this the only version available?" or "Has this drug been on shortage before?" Some pharmacies keep backup lists or can order from alternate suppliers. If your medication is critical, talk to your doctor about alternatives before you run out. And don’t assume a new brand is safer—many are made in the same factories, just under a different label.
The posts below dive into what’s really going on behind the scenes: why certain drugs keep running out, how manufacturing defects play a role, how global policies affect what’s on your shelf, and what you can do to protect yourself when the system falters. You’ll find real stories, practical checks, and clear comparisons—not just warnings, but ways to act before it’s too late.

- Dec 1, 2025
- Posted by Cillian Osterfield
Government Response to Drug Shortages: Federal Actions in 2025
In 2025, the U.S. government is responding to record drug shortages with stockpiling, AI monitoring, and new laws-but critical gaps remain in manufacturing, enforcement, and economic incentives that keep shortages alive.
Categories
- Health and Wellness (72)
- Medications (69)
- Health and Medicine (28)
- Pharmacy Services (12)
- Mental Health (9)
- Health and Career (2)
- Medical Research (2)
- Business and Finance (2)
- Health Information (2)
Latest Posts
©2026 heydoctor.su. All rights reserved