When you walk into the pharmacy to pick up your prescription, you expect to pay your copay and leave. But what if your copay suddenly jumps from $20 to $80? Or worse-your doctor’s prescribed medication isn’t covered at all? That’s often because of something called a drug formulary. It’s not a secret code or a hospital policy you can’t understand. It’s a list. A simple, official list of medications your insurance plan agrees to pay for. But what’s on that list-and where it’s placed-can make a huge difference in your wallet and your health.
What Exactly Is a Drug Formulary?
A drug formulary is a list of prescription medications that your health insurance plan (or Medicare Part D) covers. It’s not random. It’s built by a team of doctors, pharmacists, and health experts called a Pharmacy and Therapeutics (P&T) committee. They look at clinical studies, safety data, and real-world outcomes to decide which drugs work best-and which ones offer the best value. The goal? To help you get the right medicine while keeping costs down for everyone. Think of it like a grocery store’s sale section. Not every brand is on sale. The store picks the ones that are both good quality and affordable. Insurance plans do the same thing. They put certain drugs on their “preferred” list because they’ve proven to be effective and cost-efficient. Nearly every private insurance plan, Medicare Part D, and Medicaid program in the U.S. uses a formulary. In fact, over 95% of Americans with prescription coverage are affected by one. And while it sounds technical, you don’t need a medical degree to understand it.How Are Drugs Organized in a Formulary?
Most formularies use a tier system-usually 3 to 5 levels-to show how much you’ll pay for each drug. The lower the tier, the less you pay. Here’s how it typically breaks down:- Tier 1: Generic Drugs - These are the cheapest. They contain the same active ingredients as brand-name drugs but cost a fraction of the price. Most plans charge $0-$10 for a 30-day supply. The FDA requires generics to meet the same strict standards for safety, strength, and effectiveness as brand-name versions.
- Tier 2: Preferred Brand-Name Drugs - These are brand-name medications that the plan has negotiated lower prices for. You might pay $25-$50 per prescription, or 15-25% coinsurance.
- Tier 3: Non-Preferred Brand-Name Drugs - These are brand-name drugs that aren’t on the preferred list. They’re more expensive for the plan, so you pay more too-usually $50-$100 per fill or 25-35% coinsurance.
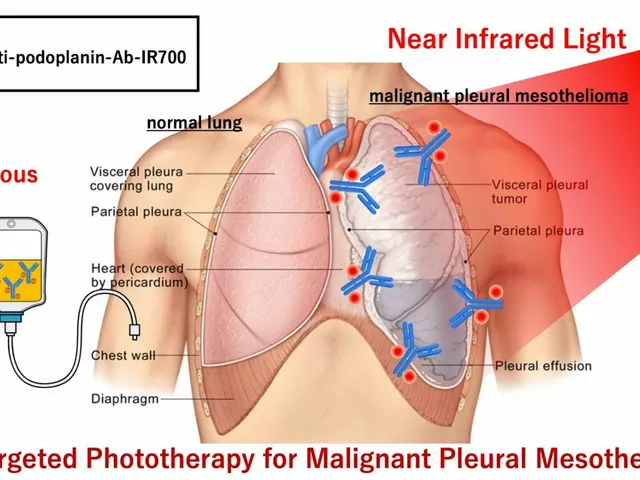
- Tier 4: Specialty Drugs - Used for complex conditions like cancer, multiple sclerosis, or rheumatoid arthritis. These are often injectables or infusions. Copays can be $100-$300, or 30-50% coinsurance. Some plans even have a Tier 5 for the most expensive drugs, like gene therapies.
Here’s the key: the same drug can be on different tiers across different plans. For example, your diabetes pill might be Tier 2 with one insurer and Tier 3 with another. That’s why a $35 monthly cost with one plan can become $150 with another.
Why Do Formularies Have Restrictions?
It’s not enough to just list drugs. Formularies often come with rules to control how they’re used. These are called utilization management tools, and they’re meant to prevent waste and ensure safety:- Prior Authorization - Your doctor must get approval from the insurance company before the drug is covered. This often happens with high-cost or high-risk medications.
- Step Therapy - You have to try a cheaper, approved drug first. Only if it doesn’t work can you move to the one your doctor originally prescribed.
- Quantity Limits - You can only get a certain amount at a time. For example, maybe you’re limited to 30 pills per month, even if your doctor prescribed 60.
These rules can feel frustrating. One patient on Reddit shared: “I was prescribed a medication for my arthritis, but my plan made me try three cheaper ones first. I waited six weeks-and the pain got worse.”
But here’s the flip side: these tools help keep premiums lower for everyone. Without them, plans would have to charge more to cover every drug, no matter the cost.
What Happens If Your Drug Isn’t on the Formulary?
If your medication isn’t listed at all, it’s called “non-formulary.” That means your plan won’t cover it-or will charge you full price, which could be thousands of dollars.But you’re not stuck. You can ask for a formulary exception. This is a formal request, usually filed by your doctor, asking the insurance company to cover the drug anyway. Your doctor needs to explain why the formulary alternatives won’t work for you-maybe you had bad side effects, or the drug is the only one that controls your condition.
According to Medicare data, about 67% of these exceptions are approved. Expedited requests (for urgent cases) are often decided within 24 hours. Standard requests take about 72 hours.
One patient with cancer said: “My immunotherapy wasn’t on the formulary at first. My oncologist filed an exception. It was approved in two days. I paid $95 instead of $5,000.”
How to Check Your Formulary (And When to Do It)
You can’t just assume your meds are covered. Plans change their formularies every year-and sometimes mid-year.- For Medicare Part D: Use the Medicare Plan Finder tool. It’s updated every October for the next year’s coverage.
- For private insurance: Log in to your plan’s website. Look for “Drug Formulary,” “Preferred Drug List,” or “Formulary Search.” Most plans make this available online.
- When to check: Always check before your doctor writes a new prescription. Also check during open enrollment (October 15-December 7 for Medicare) when you can switch plans.
According to a 2023 Kaiser Family Foundation survey, 68% of insured adults check their formulary before filling prescriptions. And 42% have switched medications because of formulary changes.
Here’s a real example: A woman with type 2 diabetes had her medication move from Tier 2 to Tier 3. Her monthly cost jumped from $35 to $85. She couldn’t afford it, so she switched to a generic alternative. Her blood sugar stayed under control.

Changes in 2024-2025 That Affect You
The rules are changing. Here’s what’s new:- Insulin cap: Since 2023, Medicare Part D plans cap insulin at $35 per month. That’s a huge relief for millions.
- Out-of-pocket cap: Starting in 2025, there will be a $2,000 annual cap on what you pay for all covered drugs under Medicare Part D.
- Biosimilars: More affordable versions of biologic drugs (like Humira or Enbrel) are being approved. Formularies are adding them to cut costs.
- Transparency: Plans must now use standardized forms for exceptions. This makes the process easier to understand.
These changes are designed to make coverage fairer. But they also mean you need to stay updated. A drug that was covered last year might not be this year.
What You Can Do Right Now
You don’t have to guess or wait for surprises. Here’s your action plan:- Find your plan’s formulary-go to your insurer’s website and search for “formulary” or “drug list.”
- Look up your meds-enter the exact name (brand or generic) to see the tier and any restrictions.
- Ask your pharmacist-they can check coverage while you wait.
- Ask your doctor-if your drug is expensive or restricted, ask: “Is there a similar drug on my formulary?”
- Check every year-don’t wait for a bill to tell you something changed.
And if you’re hit with an unexpected charge? Don’t accept it. Call your insurer. Ask for the reason. Ask about an exception. You have rights.
Bottom Line: Formularies Are Tools-Not Barriers
Drug formularies aren’t perfect. They can be confusing. Sometimes they delay care. But they’re also why millions of people can afford life-saving drugs at all.When used well, formularies help you get the best treatment at the lowest cost. When they’re too rigid, they can hurt. Your job is to understand them, use them, and speak up when they don’t work for you.
Know your list. Know your tier. Know your options. That’s how you take control of your care-and your costs.
What is the difference between a formulary and a drug list?
There’s no difference. "Formulary" and "drug list" are used interchangeably. Some insurers call it a Preferred Drug List (PDL), but they all mean the same thing: a list of medications your plan covers.
Can my insurance change my formulary during the year?
Yes. While most updates happen each January, insurers can remove or re-tier drugs mid-year if new safety data emerges or if they renegotiate pricing. They must give you at least 60 days’ notice before a change takes effect.
Why is my generic drug not on Tier 1?
Even generics can be placed on higher tiers if the plan has a deal with a brand-name manufacturer that makes the generic less cost-effective. This is rare, but it happens. Always check the tier-don’t assume all generics are cheap.
Do all insurance plans have the same formulary?
No. Every plan builds its own formulary based on negotiations with drug makers. Two plans from the same insurer might have different lists. That’s why comparing plans during open enrollment matters.
How do I know if my drug is a specialty medication?
Specialty drugs are usually high-cost, require special handling (like refrigeration), or are given by injection or infusion. They’re often used for cancer, autoimmune diseases, or rare conditions. If your drug costs more than $670 per month (as of 2024), it’s likely classified as specialty.
Can I switch plans just because my drug was removed from the formulary?
Outside of open enrollment, you usually can’t switch plans unless you qualify for a Special Enrollment Period. But if your drug was removed, you can request a formulary exception. If denied, you may qualify for a special enrollment to switch to a plan that covers your drug.







14 comments
sagar patel
Formularies are just cost-control tools disguised as patient care. Insurance companies don't care if you suffer-they care about margins. That $35 insulin cap? Only because Congress forced their hand. Don't be fooled.
Michael Dillon
Yeah but let’s be real-without formularies, premiums would be $1000/month. I’d rather pay $50 for a Tier 3 drug than see my neighbor lose their house because the plan went bankrupt. It’s not perfect, but it’s the system we’ve got.
Katherine Blumhardt
I just had to fight my insurer for 3 months to get my antidepressant covered 😔 they moved it to Tier 4 and said 'try Zoloft first'-but Zoloft made me feel like a zombie. My therapist cried when I told her. I’m not even mad anymore. Just tired.
Bailey Adkison
Anyone who thinks formularies are fair hasn’t read the fine print. These are negotiated backroom deals between pharma and insurers. The drugs that make the list aren’t the best-they’re the ones with the biggest kickbacks. Wake up.
Sophie Stallkind
It is imperative that patients understand the structure of formularies, as they directly impact therapeutic adherence and financial stability. A comprehensive review of one's formulary prior to prescription initiation is not merely advisable-it is a critical component of responsible healthcare navigation.
Winni Victor
They call it a 'formulary' like it's some kind of medical bible. Nah. It's a corporate spreadsheet written by accountants who’ve never held a pill in their hand. My dad died because his chemo drug got kicked off the list mid-treatment. They called it 'cost optimization.' I call it murder by bureaucracy.
Terry Free
Step therapy? More like step to the back of the line. My doctor prescribed a drug that works. Insurance says 'try three cheaper ones first.' So I tried three that made me sicker. Now I'm on the original drug-after 6 months of pain. Congrats, insurance. You saved $200. I lost 6 months of my life.
Lindsay Hensel
Thank you for this clear, compassionate breakdown. Many patients feel powerless when faced with formulary changes. Your guidance empowers them to advocate for themselves-and that is no small thing.
Linda B.
Did you know the P&T committees are secretly funded by Big Pharma? The 'experts' deciding which drugs make the list? They all have consulting contracts with the same companies that make the most expensive meds. This isn’t science-it’s a rigged casino.
Christopher King
They tell you to 'know your tier' like it’s a game. But what if your tier changes every month? What if your drug gets yanked because some CEO decided to cut costs? You’re not a patient-you’re a line item. And the system doesn’t care if you live or die, as long as the quarterly report looks good.
Justin James
Look, I get it. Formularies are meant to save money. But here’s the thing: when you cap insulin at $35, you’re not saving money-you’re exposing how broken the entire system is. If a life-saving drug should cost $35, why does it cost $500? The real problem isn’t the formulary-it’s the price tag. And no tier system fixes that. It just hides it behind a curtain of bureaucracy. They’re not protecting you. They’re protecting profits. And you’re paying for it-with your health, your time, your dignity.
Zabihullah Saleh
Back home in Afghanistan, we didn’t have formularies. We had hope. And sometimes, just one pill. I miss that. Here, I spend more time fighting insurance than I do with my doctor. I’m not anti-formulary. I’m anti-obsession with paperwork over people.
Rick Kimberly
It is important to note that formulary changes are often communicated via email or portal updates, which many elderly or low-income patients may not monitor regularly. Proactive consultation with pharmacists and primary care providers is strongly recommended to mitigate adverse outcomes.
Oluwatosin Ayodele
Why are you even surprised? In the US, healthcare is a business. Not a right. If your drug isn’t profitable, it’s not getting covered. Simple math. Stop acting like this is a flaw-it’s the feature. You’re not a patient. You’re a customer. And customers don’t get to pick the menu. The CEO does.