If you’ve ever had stomach pain, bloating, or changes in your bowel habits, you’ve probably wondered: is this IBS or IBD? The two sound similar, and they even share some symptoms. But they’re not the same. One is a functional problem - your gut looks normal but acts up. The other is an inflammatory disease - your gut is actually damaged. Mixing them up can lead to the wrong treatment, unnecessary worry, or even dangerous delays in care.
What Is IBS? A Functional Disorder Without Visible Damage
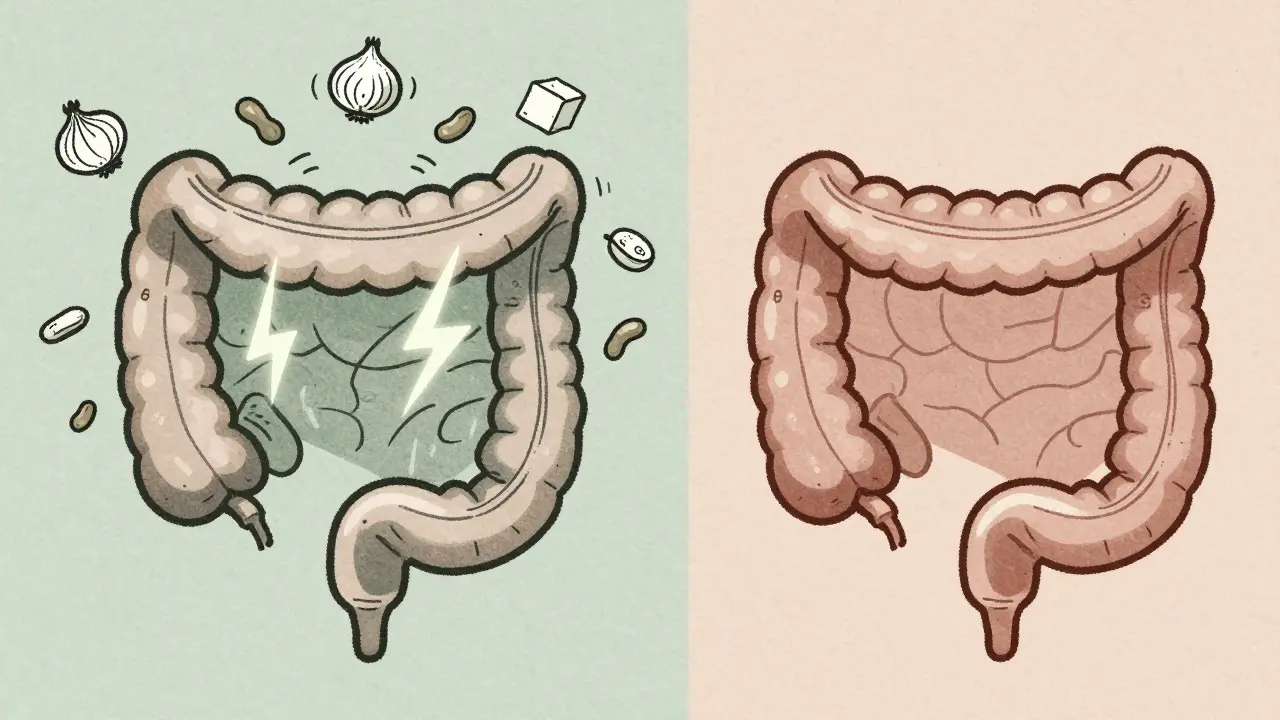
IBS - Irritable Bowel Syndrome - doesn’t show up on scans, blood tests, or colonoscopies. Your intestines look perfectly healthy. But they don’t work right. The nerves in your gut are overly sensitive. The muscles contract too strongly or too weakly. That’s why you get pain, bloating, diarrhea, or constipation - even though nothing’s physically wrong.
The Rome IV criteria, used by doctors worldwide since 2016, define IBS as recurring abdominal pain at least one day a week for three months, along with changes in bowel habits. About 76% of people with IBS report bloating. Nearly half notice mucus in their stool. Symptoms often flare after eating, especially with certain foods like onions, beans, or dairy.
There’s no cure for IBS, but many people find relief. A low-FODMAP diet works for 76% of patients, according to a 2021 review in Clinical Gastroenterology and Hepatology. That means cutting back on fermentable carbs that feed gut bacteria and cause gas. Some find help with low-dose antidepressants, which calm nerve signals in the gut. Others use medications like eluxadoline for diarrhea-predominant IBS.
Crucially, IBS doesn’t cause bleeding, weight loss, or fever. It doesn’t lead to cancer or damage your intestines. The Mayo Clinic confirms it won’t turn into IBD. But it can still wreck your life. People with IBS say they’d give up coffee, sex, or even their phone to be free of symptoms.
What Is IBD? Chronic Inflammation That Changes Your Gut
IBD - Inflammatory Bowel Disease - is not a function problem. It’s a structural one. Your immune system attacks your own digestive tract, causing real, visible damage. There are two main types: Crohn’s disease and ulcerative colitis.
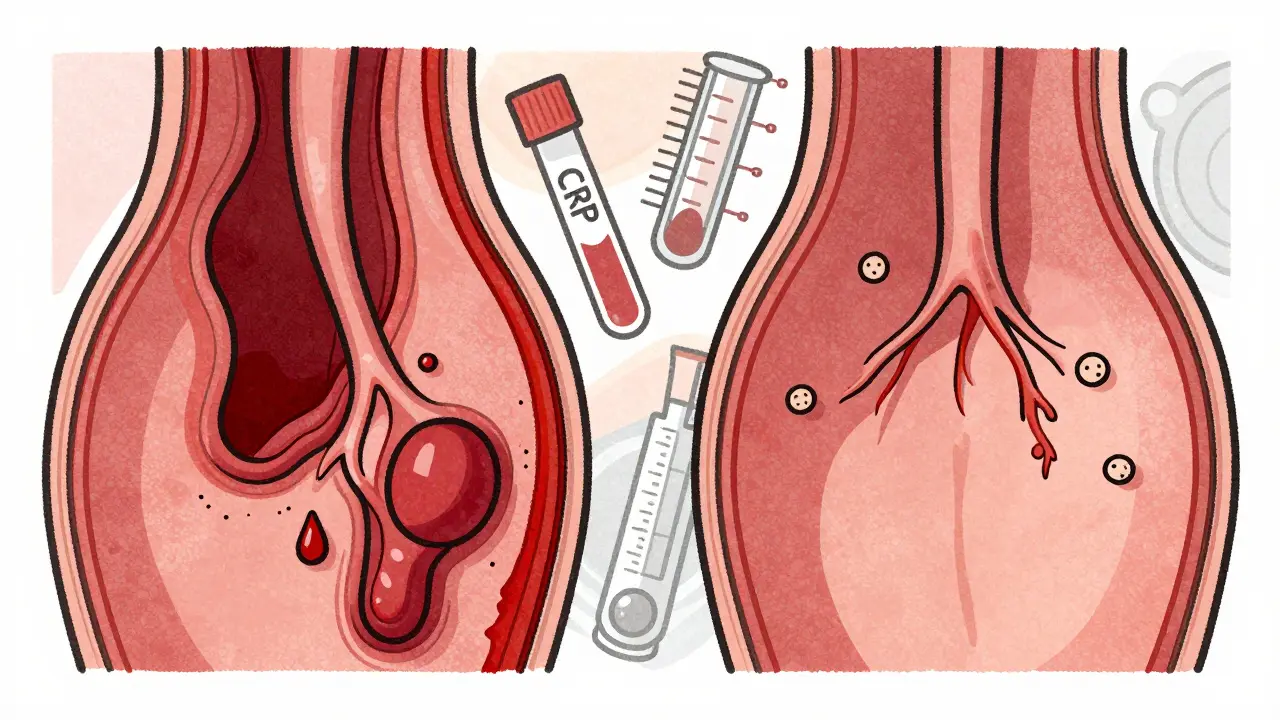
Crohn’s can affect any part of the GI tract, from mouth to anus. It creates deep, patchy ulcers and thickens the bowel wall. Over time, it can cause strictures - narrow sections that block food - or fistulas - abnormal tunnels between organs. About 33% of Crohn’s patients develop strictures within 10 years.
Ulcerative colitis only hits the colon and rectum. It causes continuous, shallow ulcers in the inner lining. Blood in the stool is common - 92% of ulcerative colitis patients have it at diagnosis. Unlike IBS, where blood is a red flag, it’s a hallmark of IBD.
IBD patients often have symptoms beyond the gut. Joint pain, skin rashes like erythema nodosum, eye inflammation (uveitis), and liver issues are all linked to IBD. These are called extraintestinal manifestations. They’re a sign your immune system is overactive, not just in your gut.
Weight loss, fever, and fatigue aren’t just annoying - they’re warning signs. The CDC says these are not typical of IBS. If you’re losing weight without trying or running a fever with stomach pain, you need urgent evaluation. IBD can lead to serious complications: toxic megacolon, perforated bowel, and increased cancer risk. After 10 years of pancolitis, the risk of colorectal cancer jumps by 2% each year.
How Doctors Tell Them Apart
Here’s the key: IBS is diagnosed by ruling everything else out. IBD is diagnosed by finding something wrong.
For IBS, your doctor will check for alarm signs: blood in stool, unexplained weight loss, family history of colon cancer, or symptoms starting after age 50. If none are present, and your blood tests and colonoscopy come back normal, you’re likely diagnosed with IBS. That’s the Rome IV process - a diagnosis of exclusion.
For IBD, doctors look for inflammation. Blood tests show elevated CRP (C-reactive protein) - levels above 5 mg/L when normal is under 3. Stool tests reveal high calprotectin - over 250 µg/g, when normal is under 50. These markers mean immune cells are active in your gut lining.
Colonoscopy is the gold standard. In IBD, biopsies show inflamed tissue, crypt abscesses, or granulomas. In IBS, everything looks normal. Imaging like MRI enterography can show thickened bowel walls, abscesses, or fistulas - all signs of Crohn’s. You won’t see any of that in IBS.
Dr. Baidoo of Regional One Health puts it simply: “IBD is a structural disease. IBS is a functional disease.” That’s the entire difference.
Treatment: Calming Nerves vs. Stopping Inflammation
IBS treatment is about managing signals. You’re not fixing damage - you’re calming a hypersensitive system. Dietary changes, stress reduction, and gut-targeted meds like peppermint oil capsules or rifaximin help. Low-dose tricyclic antidepressants reduce pain by 50% in 60% of IBS patients. It’s not about suppressing your immune system - it’s about quieting your nerves.
IBD treatment is about stopping the attack. You need drugs that suppress your immune system. Anti-TNF drugs like infliximab bring remission in 50-60% of Crohn’s patients within 14 weeks. Steroids work fast for flares but can’t be used long-term - they cause bone loss, diabetes, and cataracts. Newer biologics like vedolizumab target only gut inflammation, reducing side effects.
Some IBD patients need surgery - removing part of the colon or rectum. That’s not an option for IBS. You can’t surgically fix a nervous system that’s too reactive.
And yes - you can have both. About 22-35% of IBD patients in remission still meet IBS criteria. Their gut is healed, but their nerves stay jumpy. That’s why some people on IBD meds still have bloating and cramps. It’s not the disease coming back - it’s IBS hanging around.

What You Should Do If You’re Unsure
Don’t guess. Don’t rely on Google. If you have:
- Bloody stool
- Unexplained weight loss
- Constant fever
- Severe fatigue
- Joint pain or skin rashes with gut issues
- get tested for IBD. These are not IBS symptoms. They’re red flags.
If you’ve been told you have IBS but still have alarming symptoms, ask for a second opinion. Some doctors skip tests because IBS is common. But missing IBD can cost you your colon - or worse.
Even if you have IBS, track your symptoms. What foods trigger them? When do they get worse? Stress? Sleep? That’s your roadmap to control. IBS isn’t a life sentence - it’s a puzzle you can solve with patience and the right tools.
IBD is more serious. But with modern treatments, many people live full lives. The goal isn’t just symptom control - it’s healing the gut and preventing long-term damage.
Final Takeaway: It’s Not About the Pain - It’s About the Cause
Both IBS and IBD hurt. Both make you feel isolated. Both make you cancel plans and avoid restaurants. But one is a misfiring system. The other is a burning house.
IBS: Your gut is fine, but the alarm system is broken. Turn down the volume.
IBD: Your gut is on fire. Put it out before it spreads.
Know the difference. Ask the right questions. Get the right tests. Your future self will thank you.




9 comments
Nina Stacey
Wow this post literally changed how I think about my stomach issues I’ve been dealing with for years I always thought it was just stress but now I realize I might’ve been ignoring real red flags
My mom had Crohn’s so I’ve always been paranoid about any gut pain but never knew the difference between IBS and IBD until now
Thanks for breaking it down like this I’m going to finally push for bloodwork and a colonoscopy instead of just taking peppermint oil and hoping for the best
Kevin Motta Top
IBS is a misfiring alarm. IBD is a burning house. Perfect analogy.
Alisa Silvia Bila
I appreciate how this explains both sides without minimizing either. IBS isn’t ‘all in your head’ and IBD isn’t just ‘bad digestion.’ Both are real, both are hard, and both deserve care.
My cousin was misdiagnosed with IBS for 4 years before they found Crohn’s. By then, she needed surgery. Please don’t wait if something feels off.
Marsha Jentzsch
Ugh I’ve been told I have IBS but I’ve had fevers and weight loss for months and my doctor just said ‘stress’ and gave me ZzzQuil??
Are you serious?? I’m not lazy I’m not anxious I’m not ‘overthinking’-I’m losing hair and my joints ache and I can’t eat anything without screaming pain and now you’re telling me I might have IBD??
Why do doctors just shrug and say ‘it’s probably IBS’ when the red flags are flashing like a damn neon sign??
I’m going to the ER tomorrow and I’m bringing this article with me and I’m not leaving until they do a calprotectin test and an MRI and if they don’t I’m suing for malpractice because I’m not dying because someone didn’t want to look at a colonoscopy report.
Also I’ve been on low-FODMAP for 8 months and it did NOTHING so I’m done with diets and I’m done with being gaslit by the medical system.
Danielle Stewart
This is one of the clearest breakdowns I’ve ever read. Thank you for writing it.
If you’re reading this and you’ve been told you have IBS but still have unexplained weight loss, fevers, or blood in stool-please don’t accept that answer. Push for testing. You’re not being dramatic. You’re being smart.
And if you have IBS-you’re not broken. Your gut isn’t defective. It’s just hypersensitive. There’s hope, and there are tools. You’re not alone.
Also, if you’re a doctor reading this-please don’t skip the basics. Don’t assume. Don’t dismiss. Your patient might be one test away from a life-changing diagnosis.
Sajith Shams
You people are so naive. IBS doesn’t exist. It’s just undiagnosed IBD. Every single person who says they have IBS has low-grade inflammation they’re ignoring. Your ‘low-FODMAP diet’ is just placebo. The real problem is your lazy lifestyle and processed food addiction.
My cousin had ‘IBS’ for 12 years. Turned out he had Crohn’s and his colon was half-dead. You think peppermint oil fixes that? Wake up.
India has way better gut health than the US because we don’t eat gluten-free junk and we don’t treat every stomach ache like a medical emergency. You’re all hypochondriacs.
Glen Arreglo
Sajith, you’re oversimplifying. IBS and IBD are both real, and both need respect. The fact that you’ve seen one case doesn’t invalidate millions of others.
Also, your ‘India has better gut health’ claim? That’s not backed by global GI epidemiology. India has high rates of parasitic infections and malnutrition-related gut issues-not ‘better’ gut health.
Let’s not replace one myth with another. The science here is clear: IBS is functional. IBD is inflammatory. Both need different care. Both deserve compassion.
shivam seo
Ugh I’m so tired of these ‘IBS vs IBD’ articles. They’re just clickbait. Everyone knows it’s all about diet. No one needs a colonoscopy. Just cut out sugar and gluten and you’ll be fine.
Also, why are all these people so dramatic? My grandpa had ‘IBD’ and he just ate rice and died at 82. You’re all overreacting because you’re too soft.
Also, I’m Australian and we don’t do this overthinking nonsense here. We just drink beer and ignore it.
benchidelle rivera
To the person who said they’re going to the ER tomorrow: I’m proud of you. You’re advocating for yourself, and that’s the most powerful thing you can do.
To the doctor who dismissed you: shame on you.
To everyone else reading this: if you’ve been told ‘it’s just IBS’ and you still feel like something’s wrong-trust yourself. Your body is not lying.
Get the tests. Demand the answers. You deserve to know what’s happening inside you. This isn’t about being dramatic. It’s about being alive.
And if you have IBS-your pain is valid. Your struggle is real. You’re not broken. You’re adapting. And you’re not alone.