When your panic attack hits like a freight train-heart racing, chest tight, mind spinning out-benzodiazepines can feel like a lifeline. They work fast. Really fast. Within minutes, the terror starts to fade. That’s why doctors still prescribe them. But here’s the catch: what helps today can trap you tomorrow.
How Benzodiazepines Actually Work
Benzodiazepines don’t just make you feel calm. They change how your brain works at a chemical level. They boost the effect of GABA, a natural calming neurotransmitter. Think of GABA as your brain’s brake pedal. Benzodiazepines press it down harder and faster than your brain normally would. That’s why they stop panic attacks, quiet seizures, and help you sleep when nothing else will.
Not all benzodiazepines are the same. Some wear off in hours, others stick around for days. Alprazolam (Xanax) is short-acting, good for sudden panic. Diazepam (Valium) lasts longer, used for muscle spasms or alcohol withdrawal. Lorazepam (Ativan) sits in the middle-often used in hospitals. Triazolam (Halcion) is only for sleep, because it clears your system so quickly you won’t feel groggy the next day.
This matters because the half-life determines how you use them. Short-acting ones are better for panic or insomnia. Long-acting ones help with chronic anxiety or detoxing from alcohol. But no matter the type, they all carry the same hidden risk: dependence.
The Real Benefits: When They Save Lives
Benzodiazepines aren’t just for anxiety. They’re essential tools in emergencies. In the ER, when someone is having a seizure that won’t stop, midazolam or diazepam can stop it within seconds. In the ICU, they help patients on ventilators stay calm. For people going through alcohol withdrawal, they prevent deadly seizures and delirium.
For acute anxiety, they’re unmatched. While SSRIs like sertraline or escitalopram take 4 to 6 weeks to kick in, a single dose of alprazolam can calm someone down in under an hour. That’s why they’re still used-when someone is suicidal from panic, or can’t leave their house because of terror, these drugs can be the bridge to getting help.
Studies show 60% to 80% of people with acute anxiety see big improvements within days. That’s better than any other class of medication for immediate relief. In those moments, the benefit outweighs the risk.
The Hidden Trap: How Dependence Builds
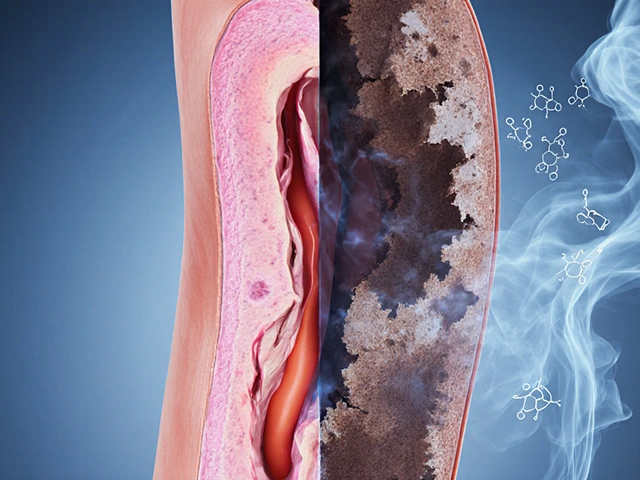
Here’s the problem no one tells you until it’s too late: your brain adapts. After just 2 to 4 weeks of daily use, your GABA receptors start to downregulate. They need more of the drug to get the same effect. That’s tolerance. Then, when you try to stop, your brain is left without enough natural calming power. That’s withdrawal.
Between 30% and 50% of people who take benzodiazepines daily for more than a month become physically dependent-even if they’re taking the dose their doctor prescribed. That’s not addiction. That’s biology. Addiction means you’re using it to get high or to escape. Dependence means your body literally can’t function without it.
Withdrawal isn’t just feeling jittery. It can include:
- Severe rebound anxiety-worse than before you started
- Insomnia that makes sleep impossible
- Tremors, muscle cramps, and sweating
- Heart palpitations and high blood pressure
- Seizures, hallucinations, and feelings of unreality
One study found that 23% of people on prescribed doses had memory gaps during daily life-forgetting conversations, driving routes, or even meals. That’s anterograde amnesia. It’s not rare. It’s a documented side effect.

Who’s at Highest Risk?
Not everyone who takes benzodiazepines ends up stuck. But some groups are far more vulnerable.
Women are prescribed these drugs nearly twice as often as men. In the U.S., 8.3 prescriptions per 100 women versus 4.3 per 100 men. Why? Partly because women are more likely to be diagnosed with anxiety. Partly because doctors assume they’ll be more compliant. But that doesn’t make them safer.
Older adults are another high-risk group. The American Geriatrics Society warns that benzodiazepines increase fall risk by 50% in people over 65. They also raise dementia risk by 32% with long-term use. Yet they’re still prescribed to seniors for sleep and anxiety-despite safer alternatives like CBT-I for insomnia.
People with a history of substance use disorder are at extreme risk. Even if they’ve been clean for years, benzodiazepines can trigger relapse. The brain’s reward system gets hijacked. What starts as a prescription can turn into a craving.
Alternatives That Work Better Long-Term
If you’ve been on benzodiazepines for more than a month, it’s time to talk about what comes next. The truth? There are better options for lasting relief.
CBT-I (Cognitive Behavioral Therapy for Insomnia) is the gold standard for sleep problems. It doesn’t just help you sleep-it rewires how you think about sleep. Studies show it’s more effective long-term than any sleeping pill.
SSRIs and SNRIs like fluoxetine, sertraline, or venlafaxine take longer to work, but they don’t cause dependence. They’re the first-line treatment for generalized anxiety, panic disorder, and PTSD. They’re not perfect-they can cause nausea or sexual side effects-but they’re safe for years.
And then there’s the combo approach. A 2023 study in JAMA Internal Medicine found that people who used low-dose benzodiazepines along with CBT cut their risk of long-term dependence by 58%. The drug gave them breathing room. The therapy gave them back control.

How to Get Off Safely
If you’ve been on benzodiazepines for more than a few weeks, quitting cold turkey is dangerous. Seizures and psychosis can happen. That’s why tapering is non-negotiable.
The Ashton Manual is the most trusted guide for this. It recommends reducing your dose by 5% to 10% every 1 to 2 weeks. For someone on a high dose for years, that can take 6 months to a year. It’s slow. It’s hard. But it works.
Switching from a short-acting benzo like alprazolam to a long-acting one like diazepam can make the process smoother. Diazepam’s slow clearance helps avoid withdrawal spikes. Your doctor needs to know this. If they don’t, find one who does.
Don’t try to do this alone. Support groups, therapists trained in withdrawal, and pharmacists who specialize in mental health meds can make the difference between a rough patch and a medical crisis.
The Future of Benzodiazepines
Prescriptions are already falling. Kaiser Permanente cut long-term use by 37% by adding electronic alerts when prescriptions go past 90 days. The UK’s NICE guidelines now say don’t start benzodiazepines for anxiety at all. The FDA added a boxed warning in 2020 about abuse and dependence.
But they’re not disappearing. In emergency rooms, in ICUs, in alcohol detox centers-they’re still lifesavers. The goal isn’t to ban them. It’s to use them like a fire extinguisher, not a daily drink.
Doctors are learning. Patients are learning. The data is clear: short-term use, with clear exit plans, can be safe. Long-term use? It’s a gamble most people don’t win.
If you’re on these meds and feel stuck, you’re not weak. You’re not broken. You’re just caught in a system that gave you fast relief without a roadmap out. The good news? There is a way out. And it starts with one conversation-with your doctor, with a therapist, with someone who understands.
Can benzodiazepines be used safely?
Yes-but only for short-term, targeted use. They’re safe and effective for acute panic attacks, procedural sedation, or alcohol withdrawal when used under medical supervision for less than 4 weeks. Long-term daily use significantly increases the risk of dependence, tolerance, and dangerous withdrawal. The key is having a clear end date before you start.
What’s the difference between dependence and addiction to benzodiazepines?
Dependence means your body has adapted to the drug and needs it to function normally. Withdrawal symptoms occur if you stop. Addiction means you’re using it compulsively, despite harm, often chasing euphoria or using it to escape emotions. You can be dependent without being addicted. But addiction almost always includes dependence.
Why are benzodiazepines still prescribed if they’re so risky?
Because they work fast-and sometimes, fast is life-saving. For someone in a full-blown panic attack, waiting 6 weeks for an SSRI isn’t an option. For a patient having a seizure in the ER, there’s no better option than diazepam. The issue isn’t the drug-it’s how it’s used. When prescribed without limits, without follow-up, and without a plan to taper, the risks skyrocket.
How long does benzo withdrawal last?
It varies. Acute withdrawal usually peaks within 1 to 4 days after stopping short-acting benzos (like Xanax) and can last 1 to 2 weeks. For long-acting ones (like Valium), it may take longer to start but can last 2 to 8 weeks. Protracted withdrawal-where symptoms like anxiety, insomnia, or brain zaps linger-can last months or even over a year in some cases, especially after years of use. Slow tapering reduces severity and duration.
Are there natural alternatives to benzodiazepines for anxiety?
There are no natural substances that replicate the speed or strength of benzodiazepines. But evidence-backed non-drug approaches work better over time: CBT for anxiety, mindfulness meditation, regular aerobic exercise, and sleep hygiene. Magnesium and L-theanine may help mild symptoms, but they’re not replacements for medical treatment. The most effective strategy combines therapy with lifestyle changes-not supplements.
What to Do Next
If you’re taking benzodiazepines and feel like you can’t quit, don’t panic. You’re not alone. Start by writing down:
- How long you’ve been taking them
- Why you were prescribed them
- What symptoms you’re trying to manage
- What happens if you miss a dose
Then, schedule a talk with your doctor. Bring this information. Ask: "Is this still the right treatment for me?" "What’s my exit plan?" "Are there alternatives?"
If your doctor dismisses your concerns, find one who listens. Mental health isn’t about quick fixes. It’s about sustainable healing. And sometimes, the bravest thing you can do is ask for help leaving something that once saved you.


12 comments
Kathy Scaman
Been on Xanax for 3 years. Stopped cold turkey once. Thought I was gonna die. Seizure scare in the shower. Never again. Tapered with Valium over 8 months. Still have bad days but at least I can drive now. Thanks for the Ashton Manual link.
Anna Lou Chen
Let’s deconstruct the pharmacological hegemony embedded in the medical-industrial complex’s reliance on GABAergic modulation as a panacea for existential dissonance in late-stage capitalism. The real pathology isn’t anxiety-it’s the neoliberal imperative to remain perpetually productive. Benzodiazepines are merely the chemical Band-Aid on a systemic wound we refuse to address. The Ashton Manual? A beautiful relic of pre-Algorithmic Psychiatry. We need ontological rewilding, not taper schedules.
Mindee Coulter
I love how this post doesn’t just dump info but actually gives you a path forward. My therapist gave me CBT-I and it changed everything. No more sleeping pills. I still get anxious but now I know how to breathe through it. Seriously recommend.
Colin Pierce
As a pharmacist who’s worked in psych for 15 years, I’ve seen this play out too many times. Doctors prescribe Xanax like it’s Advil. Then the patient comes back 6 months later saying they can’t sleep without it. The worst part? Most don’t even know they’re dependent until they try to quit. The Ashton Manual is gold. Print it. Share it. Your doctor might not know it exists.
Mark Alan
STOP GIVING OUT DRUGS LIKE CANDY!!! 🚫💊
My uncle OD’d on Klonopin after 10 years. He was a veteran. They gave him benzos for PTSD and never told him the risks. Now he’s in a nursing home. This isn’t medicine. It’s corporate negligence. #BanBenzos
Ambrose Curtis
so i was on ativan for like 2 years after a bad breakup. felt like a zombie. tried to quit. threw up for 3 days. cried for a week. then i found a doc who switched me to diazepam and cut me down 5% every 2 weeks. took 10 months. but i can think again. no more brain fog. no more panic when i forget my keys. the key? slow. slow. slow. and dont do it alone.
Chris Urdilas
Wow. Someone actually wrote a post that doesn’t sound like a pharmaceutical ad. Who knew? 🤨
Also, the part about women being prescribed twice as much? Yeah. My mom got Xanax for ‘stress’ after my dad left. She’s been on it since 2007. ‘Stress.’ Right. Meanwhile, my dad got a referral to a therapist. Guess who’s still functional?
Mel MJPS
My sister used to take Halcion for sleep. One night she woke up at 3am and drove to the gas station 20 miles away. Didn’t remember any of it. That scared us all straight. We got her into CBT-I. Now she sleeps better than ever. No pills. Just routine and quiet.
Amber Daugs
People who take these for more than a week are weak. Real men don’t need chemical crutches. If you can’t handle your emotions, go to the gym. Or meditate. Or get a hobby. Stop looking for a pill to fix your life. You’re not broken-you’re lazy.
Robert Cardoso
Let’s be real. The FDA warning came in 2020. That’s after decades of prescribing. Why did it take so long? Because the drug companies funded the studies. Because doctors got free lunches. Because the system is rigged. The real tragedy? The people who need these drugs for emergencies are now being punished because of the abusers. And the ones who got hooked? They’re told to just ‘try harder.’
matthew martin
My grandma took Valium for 20 years. She didn’t know she was dependent until she fell and broke her hip. The hospital pulled her off it cold turkey. She had hallucinations for a week. Screamed at the ceiling like it was talking to her. That’s when we found the Ashton Manual. Took her 14 months to taper. She’s 87 now. Clear-headed. Still knits sweaters. No benzos. Just tea and patience. It’s possible. It’s just slow.
Jeffrey Carroll
Thank you for this comprehensive and deeply human overview. The distinction between dependence and addiction is critical and often misunderstood. I appreciate the emphasis on structured tapering and non-pharmacological alternatives. This is the kind of nuanced discussion our mental health discourse desperately needs.