When your stomach hurts, you’re tired all the time, and you’re rushing to the bathroom more than usual, it’s easy to blame stress or bad food. But if these symptoms stick around for weeks or months, it could be something deeper-like inflammatory bowel disease, or IBD. Among the most common forms of IBD are Crohn’s disease and ulcerative colitis. They sound similar, share many symptoms, and even get confused by doctors sometimes. But they’re not the same. Understanding the difference isn’t just academic-it changes your treatment, your prognosis, and your daily life.
Where the Inflammation Happens
- Ulcerative colitis only affects the colon and rectum-the large intestine. The inflammation starts at the rectum and moves upward in a continuous line. There are no healthy patches in between. If you have UC, your entire colon could be involved, or just the lower part. But it never touches your small intestine or stomach.
- Crohn’s disease can strike anywhere from your mouth to your anus. Most often, it hits the end of the small intestine (ileum) and the beginning of the colon. But it can show up in the stomach, esophagus, or even around the anus. What makes Crohn’s stand out is the patchy nature of the inflammation. Healthy sections of intestine sit right next to inflamed ones-like islands in a sea of normal tissue. These are called "skip lesions."
This difference in location isn’t just a map detail. It’s why Crohn’s patients often have problems absorbing nutrients-because the small intestine, where most digestion happens, is damaged. UC patients, on the other hand, mostly struggle with bleeding and urgency because the colon is where water is absorbed and stool is stored.
How Deep the Damage Goes
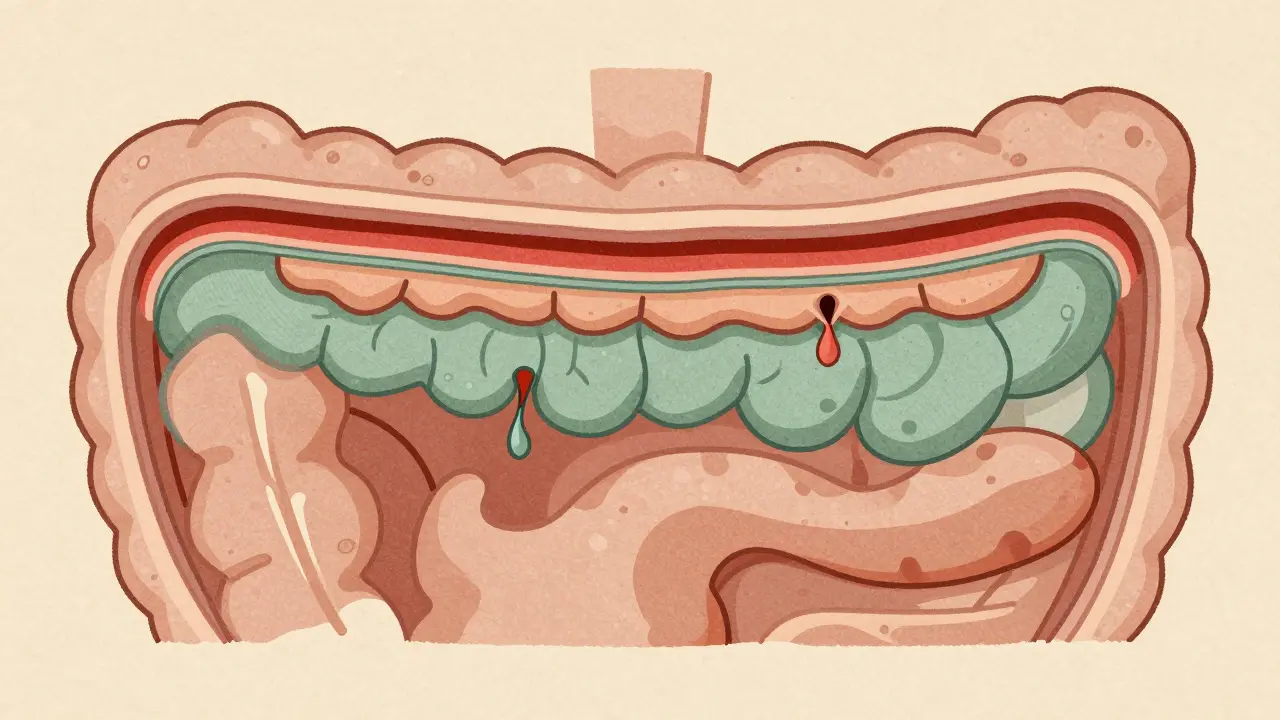
Your intestine has layers. Think of it like an onion: the inner lining (mucosa), then a thick muscle layer, then outer connective tissue. In ulcerative colitis, the damage stays mostly on the surface-in the mucosa and just below it. That’s why bleeding is so common. The lining gets so thin and raw that it bleeds easily.
Crohn’s disease doesn’t stop at the surface. It eats through all the layers. This is called transmural inflammation. When it punches through the outer wall, it can create tunnels called fistulas-abnormal connections between your intestine and bladder, skin, or other organs. About 25% of people with Crohn’s develop fistulas over their lifetime. You won’t see that in ulcerative colitis.
Another big risk with Crohn’s is strictures-narrowed sections of intestine caused by scar tissue. About one-third of people with Crohn’s will need surgery to remove a blocked part of their bowel. That’s rare in UC.
What the Tests Show
There’s no single blood test that says "yes, it’s Crohn’s" or "no, it’s UC." Diagnosis comes from putting together clues: your symptoms, imaging, endoscopy, and biopsy results.
During a colonoscopy, a doctor looks at your colon. In ulcerative colitis, the lining looks uniformly red, swollen, and ulcerated. You’ll often see pseudopolyps-small bumps of healed tissue that form after ulcers heal. In Crohn’s, the lining looks patchy, with deep, craggy ulcers and a cobblestone appearance. That’s caused by the inflammation jumping between areas.
Biopsies help too. UC shows inflammation limited to the top layers. Crohn’s shows granulomas-tiny clumps of immune cells-in about 20% of cases. Not everyone has them, but if they’re there, it’s almost always Crohn’s.
Imaging makes the difference clearer. An MRI or CT enterography can show if inflammation is in the small bowel-something UC never does. Capsule endoscopy (swallowing a tiny camera) finds Crohn’s in the small intestine in 70% of cases where colonoscopy looked normal.
Blood and stool tests add more clues. A stool test for calprotectin (a marker of gut inflammation) is high in both, but slightly higher in UC. A blood test for pANCA antibodies is positive in 60-70% of UC patients, but only 10-15% of Crohn’s patients. It’s not perfect, but it helps when the picture is blurry.
Complications That Set Them Apart
Both diseases can cause fatigue, weight loss, and joint pain. But the big risks are different.
- Ulcerative colitis carries a rare but scary risk: toxic megacolon. This is when the colon swells dangerously and can rupture. It happens in about 5% of severe UC flares. It’s life-threatening and needs emergency surgery.
- Crohn’s disease is more likely to cause fistulas and strictures. It can also lead to abscesses-pockets of infection that need drainage. People with Crohn’s are also more likely to have malnutrition because their small intestine can’t absorb vitamins like B12, iron, or fat-soluble ones (A, D, E, K).
There’s also a liver condition called primary sclerosing cholangitis (PSC). It’s linked to ulcerative colitis, affecting 3-7% of UC patients. It’s rare in Crohn’s-under 1%. PSC can lead to liver damage and even liver cancer over time.
Both can cause skin rashes, eye inflammation, and arthritis. These are called extraintestinal manifestations. About one in three IBD patients gets them. But they don’t tell you which type you have-they just mean your immune system is overactive.
Treatment Differences
Some treatments work for both. Biologics like infliximab or adalimumab help reduce inflammation in both Crohn’s and UC. But how they’re used, and how well they work, can differ.
For mild to moderate ulcerative colitis, doctors often start with medications delivered directly to the colon-enemas or suppositories with 5-ASAs. These work well because they target the problem right where it is. About 60-80% of UC patients respond. For Crohn’s, those local treatments don’t help much because the inflammation is deeper and spread out. Crohn’s needs systemic drugs that go through your whole body.
Surgery is where the biggest difference shows up.
- Ulcerative colitis can be cured. If you remove the entire colon and rectum, the disease is gone. Many people get an ileal pouch-an internal reservoir made from the end of the small intestine-that lets them pass stool normally. About 10-15% of UC patients end up with this surgery within 10 years.
- Crohn’s disease can’t be cured with surgery. Even if you cut out the diseased part, the inflammation comes back-often right next to the surgical site. About half of Crohn’s patients need another operation within 10 years. Surgery is used to fix blockages, drain abscesses, or treat fistulas, but it’s not a cure.
What Patients Actually Experience
Real-life symptoms vary, too. People with ulcerative colitis often say their biggest issue is urgency-needing to go right now-and rectal bleeding. One survey found 75% of UC patients bleed during flares, compared to just 35% of Crohn’s patients.
Crohn’s patients are more likely to talk about weight loss, bloating, and food intolerances. That’s because the small intestine, which absorbs nutrients, is often damaged. One in two Crohn’s patients says they’ve lost weight because they can’t absorb enough calories or vitamins.
Triggers are different, too. On online forums, UC patients point to stress as the main flare trigger. Crohn’s patients are more likely to blame specific foods-dairy, high-fiber veggies, or fried foods. That doesn’t mean those foods cause the disease. But they can irritate an already sensitive gut.

The Gray Zone: Indeterminate Colitis
Not every case fits neatly into one box. About 10-15% of people are initially diagnosed with "indeterminate colitis." Their symptoms and test results don’t clearly point to Crohn’s or UC. Sometimes, over time, more signs appear. A person thought to have UC might develop fistulas or skip lesions-and get reclassified as Crohn’s. Studies show about 12% of UC diagnoses are later changed after years of monitoring.
Doctors now focus less on just labeling it and more on what the disease is doing. Is it causing inflammation? Strictures? Fistulas? The behavior of the disease matters more than the name.
What’s New in Treatment
Treatment is evolving fast. New drugs like mirikizumab (for Crohn’s) and etrolizumab (for UC) are in late-stage trials and could be approved soon. Fecal microbiota transplants (FMT)-where healthy gut bacteria are transferred from a donor-are showing promise, especially for UC. One trial found 32% of UC patients went into remission after FMT. For Crohn’s, the rate was lower-22%.
Researchers are also looking at how the gut microbiome differs between the two diseases. That could lead to personalized diets or probiotics tailored to each type.
Costs are rising, too. In the U.S., severe Crohn’s disease costs about $38,500 a year in medical care. Severe UC costs around $38,000. That’s not just drugs-it’s hospital visits, scans, surgeries, and lost work time.
Bottom Line: Know the Difference
Crohn’s disease and ulcerative colitis aren’t just two names for the same thing. They’re different diseases with different patterns, risks, and treatments. Getting the right diagnosis isn’t just about checking a box-it shapes your entire future with IBD. Whether you’re dealing with bleeding, pain, or fatigue, understanding which one you have helps you and your doctor pick the best path forward.
And if you’re not sure? Don’t panic. Many people start with an unclear diagnosis-and that’s okay. Doctors will watch, test, and wait. Sometimes, the disease tells its own story over time.
Can you have both Crohn’s disease and ulcerative colitis?
No, you can’t have both at the same time. They are two distinct conditions. But sometimes, it’s hard to tell them apart at first. About 10-15% of people are initially labeled with "indeterminate colitis" because their symptoms and test results don’t clearly point to one or the other. Over time, as the disease progresses or more tests are done, most cases become clearly Crohn’s or UC. Rarely, a person might be reclassified after years of monitoring.
Is one condition more serious than the other?
Neither is "worse"-they’re just different. Crohn’s disease has a higher risk of complications like fistulas, strictures, and malnutrition because it affects the whole bowel wall and can involve the small intestine. Ulcerative colitis carries a rare but dangerous risk of toxic megacolon and has a higher chance of colon cancer over time if the entire colon is inflamed for many years. Both can severely impact quality of life. The key is early diagnosis and the right treatment plan.
Can diet cure Crohn’s or ulcerative colitis?
No diet can cure either condition. But diet can help manage symptoms. People with Crohn’s often find that avoiding high-fiber foods, dairy, or fried foods reduces bloating and diarrhea. Those with ulcerative colitis may benefit from low-residue diets during flares. Some find relief with the low-FODMAP diet, which reduces certain fermentable carbs. But these aren’t cures-they’re tools to feel better. Always work with a dietitian who knows IBD.
Do I need surgery if I have ulcerative colitis?
Not everyone does. Many people control UC with medication for years. But if medications stop working, or if you have severe bleeding, pre-cancerous changes in the colon, or toxic megacolon, surgery becomes necessary. About 10-15% of UC patients end up having their colon removed within 10 years. After surgery, many people live without symptoms and don’t need ongoing medication.
Can stress cause Crohn’s or ulcerative colitis?
Stress doesn’t cause either disease. IBD is an autoimmune condition, meaning your immune system mistakenly attacks your gut. But stress can make symptoms worse and trigger flares. Many people report that anxiety, major life events, or lack of sleep lead to more frequent bathroom trips or increased pain. Managing stress through therapy, exercise, or mindfulness can help reduce flare frequency, even if it doesn’t stop the disease itself.








11 comments
Isaac Bonillo Alcaina
Let’s be real-most people don’t even know what ‘transmural’ means, and yet they’re self-diagnosing IBD from TikTok videos. If you’re reading this and thinking ‘I have Crohn’s because I hate broccoli,’ you don’t. Stop. Just stop. This isn’t a diet trend. It’s a chronic autoimmune disorder that wrecks your life. If you’re lucky, you get meds. If you’re not, you get fistulas, surgeries, and a 3 a.m. bathroom emergency that becomes your new normal. Stop romanticizing it.
And yes, I’ve had both flares. I know what I’m talking about.
Also, ‘indeterminate colitis’? That’s just the medical system admitting it’s confused. Welcome to the club.
And no, your ‘gut cleanse’ isn’t fixing it. You’re not special. You’re just sick.
Stop posting ‘healing with turmeric’ memes. It’s not helping anyone.
Go see a gastroenterologist. Not a wellness influencer.
Bhargav Patel
The distinction between Crohn’s disease and ulcerative colitis, though clinically significant, reveals a deeper truth about the nature of medical classification itself. Human biology rarely conforms to the neat dichotomies we impose upon it. The very existence of indeterminate colitis-nearly one in seven cases-suggests that our taxonomic frameworks, however useful, are provisional tools, not eternal truths.
One might argue that the disease is not merely defined by its anatomical location or histological features, but by the lived experience of the individual: the sleepless nights, the dietary recalibrations, the quiet grief over lost autonomy. In this light, the label becomes secondary to the narrative. Perhaps medicine ought to evolve from diagnostic certainty toward therapeutic empathy.
After all, the colon does not care whether we call it Crohn’s or UC. It only knows pain, inflammation, and the desperate yearning for relief.
Let us treat the person, not just the pathology.
Lu Jelonek
As someone who’s lived with UC for 12 years, I appreciate how clearly this breaks down the differences. I used to get so frustrated when people said, ‘Oh, you have IBS, right?’ or ‘Just eat less spicy food.’
One thing no one talks about enough: the emotional toll of being misdiagnosed for years. I was told I was ‘anxious’ for five years before a colonoscopy confirmed it. The shame of thinking you’re ‘overreacting’ is real.
Also, the pouch surgery? Life-changing. I didn’t think I’d ever be able to travel again. Now I’ve been to six countries. It’s not perfect-but it’s freedom.
And yes, I still carry a bag of wipes everywhere. Always.
siddharth tiwari
cmon man this is all a lie the govts made up crohns and uc to sell drugs and get people to pay for colonoscopies. the real cause is 5g wifi and fluoridated water. i had a friend who went on a raw food diet and his symptoms vanished. they dont want you to know this. theyre all just profit driven. i saw a video on youtube where a doc said the same thing. its all connected. the pharmaceutical industry owns the aas. also why do they always say ‘biologics’? sounds like sci fi. theyre probably nanobots. i think the cia is behind this.
suhani mathur
Oh wow, a 2000-word essay on IBD and not a single mention of the fact that UC patients are basically walking time bombs for colon cancer?
Also, ‘indeterminate colitis’? That’s just the medical system’s way of saying, ‘We have no idea, but here’s a $12,000 bill anyway.’
And can we talk about how every single ‘helpful’ article forgets to mention that your insurance will deny your biologic because it’s ‘not first-line’? Yeah. That’s real life.
Meanwhile, my Crohn’s friend’s doctor just said, ‘Try a keto diet.’
Bro. I’ve eaten kale for 10 years. It didn’t help. Stop acting like nutrition is a cure.
Also-why do people always say ‘you look fine’? I feel like I’m dying. You’re just not seeing the inside of me.
Diana Alime
i swear to god i read this whole thing and still dont know if i have crohns or uc or if im just a mess. also why does everything say ‘you can be cured’ for uc but then say ‘youll need surgery’ and then say ‘but you’ll be fine’?? like who’s fine?? i’m crying in the bathroom again. and why is everyone on the internet saying ‘low fodmap’ like its a religion? i tried it. i ate plain rice for 3 weeks. i lost 15 lbs. i cried into my broth. not helpful. also i hate my colon.
Adarsh Dubey
It’s interesting how the medical community clings to binary labels when biology is so fluid. I’ve seen patients with UC develop fistulas. I’ve seen Crohn’s patients with continuous inflammation that looks just like UC. The real takeaway? The labels are useful for treatment, but they’re not the whole story.
What matters is whether the inflammation is responding. Whether the person is eating. Whether they’re sleeping. Whether they’re able to hold a job, hug their kid, or take a walk without fear.
Maybe we should measure success not by which box the diagnosis fits in, but by how much of their life they get back.
And for the love of all that’s holy-stop Googling ‘IBD symptoms’ at 2 a.m.
Bartholomew Henry Allen
This article is weak. America has the best medical system in the world. If you have Crohn's or UC you are just lazy. Get off your phone. Eat real food. Stop whining. The rest of the world doesn't have this luxury. We don't need fancy biologics. We need discipline. I have seen people in India and Africa with worse symptoms and they walk ten miles to get water. You have access to doctors. Use it. Stop complaining. This is not a privilege. This is a test of character.
Andrea Di Candia
I just want to say thank you to whoever wrote this. I’ve been diagnosed with IBD for 8 years and I’ve never seen it explained so clearly. I cried reading the part about ‘indeterminate colitis’-I thought I was broken for not fitting into a box.
Also, the part about stress not causing it but making it worse? That’s the truth. I thought I was losing my mind because I’d flare after a work presentation. Turns out, my body wasn’t weak-it was just reacting.
And yes, I carry wipes. And emergency underwear. And a list of my meds in my wallet. And I’m proud of that. I’m not ‘just stressed.’ I’m fighting. Every day.
To anyone reading this who’s scared? You’re not alone. We’re all in this weird, messy, painful, weirdly beautiful club. And we’re still here.
claire davies
Oh my goodness, this is the most beautifully written, compassionate, and clinically accurate breakdown of IBD I’ve ever read. I’ve been a nurse for 22 years, mostly in GI, and I still learned a few things-especially about the capsule endoscopy stats and the new trial drugs.
What struck me most was how you framed the emotional weight of misdiagnosis. So many patients spend years being told they’re ‘anxious’ or ‘neurotic.’ I’ve had mothers cry in my office because their 16-year-old was told they were ‘just being dramatic’ for three years before getting a colonoscopy.
And the bit about diet? Spot on. I always tell patients: ‘Your gut isn’t broken because you ate pizza. Your immune system is broken, and pizza is just the trigger.’
Also, can we all agree that ‘toxic megacolon’ is the most terrifying phrase in medicine? It sounds like a dystopian sci-fi novel. And yet-it’s real.
Thank you for writing this. I’m sharing it with every new patient I see. And maybe, just maybe, it’ll help someone feel less alone.
Raja P
i had uc for 7 years. took 4 meds. finally got the pouch. best decision ever. now i can eat tacos again. no more bleeding. no more panic attacks before leaving the house. yeah, i poop out of a hole in my stomach now. but i’m alive. and i can hug my daughter without worrying i’ll have to run to the bathroom. this article got it right. surgery isn’t failure. it’s freedom.