Shift Work Disorder Risk Checker
Shift Work Disorder is a sleep-wake condition that arises when work schedules clash with the body’s natural circadian rhythm, causing chronic fatigue, insomnia, and mood disturbances.
Anyone who’s ever pulled an all‑night shift or rotated between mornings and evenings knows the groggy feeling that follows a night of work. That tiredness isn’t just “being a little sleepy”; it can be a full‑blown disorder that impacts health, safety, and quality of life. Below you’ll find the facts you need to recognize the problem, understand why it happens, and start fixing it.
Why the Body Resists Unusual Hours
Circadian Rhythm is a 24‑hour internal clock that regulates hormones, body temperature, and sleep propensity. When work hours force you to stay awake when the rhythm signals darkness, the mismatch throws hormones like melatonin and cortisol out of sync. Melatonin, the hormone that tells you it’s time to sleep, peaks at night. Light exposure during a night shift suppresses that peak, leaving you alert when you should be winding down.
Two schedule patterns are most disruptive:
- Rotating shifts that change every few days, preventing the body from ever settling into a steady rhythm.
- Permanent night shifts that require you to stay up for long stretches of darkness.
Both patterns increase the risk of Insomnia a difficulty initiating or maintaining sleep despite adequate opportunity, leading to a cascade of secondary problems.
Core Symptoms to Spot Early
The hallmark signs of shift work disorder cluster around three domains:
- Excessive Sleepiness: Persistent fatigue during work hours, microsleeps, or an inability to stay alert.
- Insomnia: Trouble falling asleep after a night shift, frequent awakenings, or waking too early.
- Mood & Cognitive Effects: Irritability, anxiety, reduced concentration, and in severe cases, depressive symptoms.
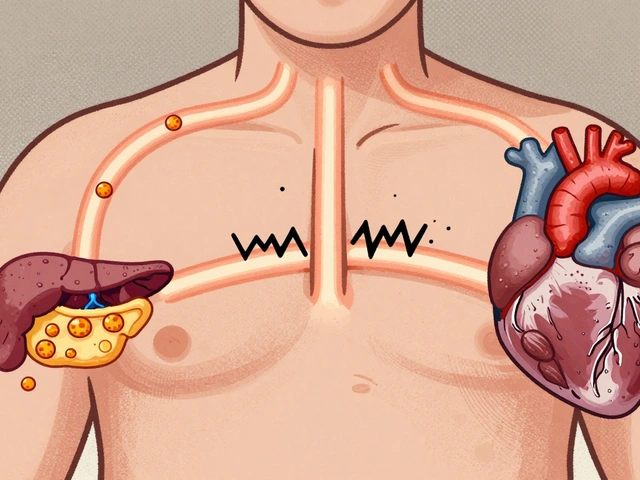
Additional clues include gastrointestinal upset, headaches, and a higher propensity for cardiovascular events-especially in workers who have been on irregular schedules for years.
How Professionals Diagnose the Condition
Diagnosis hinges on clinical interview, sleep logs, and sometimes actigraphy (a wrist‑worn device that records movement to infer sleep patterns). The Diagnostic Criteria outlined in the DSM‑5 and ICD‑10 for shift work disorder require:
- Persistent insomnia or excessive sleepiness that occurs exclusively on workdays.
- Symptoms lasting at least three months.
- Evidence that the schedule conflicts with the individual’s circadian rhythm.
- Exclusion of other sleep disorders such as sleep apnea.
Occupational health specialists often collaborate with sleep physicians to rule out other causes and to craft a workplace‑friendly management plan.
Evidence‑Based Treatment Options
There’s no one‑size‑fits‑all cure, but a combination of behavioral, environmental, and (when needed) pharmacologic strategies can dramatically reduce symptoms.
1. Light Therapy
Light Therapy is a treatment that uses bright artificial light to shift circadian timing. Exposure to 10,000 lux for 20-30 minutes at the beginning of a night shift can delay melatonin secretion, making you feel more alert. Conversely, wearing blue‑light‑blocking glasses on the way home eases the transition to sleep.
2. Cognitive Behavioral Therapy for Insomnia (CBT‑I)
Cognitive Behavioral Therapy for Insomnia a structured program that changes sleep‑negative thoughts and habits is the gold standard for chronic insomnia. For shift workers, CBT‑I is adapted to include schedule‑specific sleep‑restriction, stimulus control (using the bed only for sleep), and relaxation techniques.
3. Pharmacologic Aids
Short‑acting stimulants (e.g., modafinil) can boost alertness during a night shift, while low‑dose melatonin taken post‑shift helps initiate sleep. Prescription should be overseen by a physician, especially for individuals with cardiovascular risk.
4. Sleep Hygiene & Chronotype Alignment
Sleep Hygiene practices that promote consistent, restorative sleep includes a dark, cool bedroom, limiting caffeine after the first half of the shift, and establishing a pre‑sleep routine. Knowing your Chronotype the natural propensity toward morningness or eveningness can guide shift placement; evening‑type workers often tolerate night work better than morning‑type peers.
5. Workplace Adjustments
Employers can help by designing forward‑rotating schedules (morning → evening → night), providing well‑lit break rooms, and allowing nap periods when feasible. A policy that limits consecutive night shifts to no more than three can reduce cumulative fatigue.

Comparing Related Sleep Disorders
| Attribute | Shift Work Disorder | Primary Insomnia | Circadian Rhythm Sleep Disorder |
|---|---|---|---|
| Primary Cause | Work schedule vs. circadian timing | Psychological/physiological stress | Internal clock misalignment (e.g., jet lag) |
| Typical Symptoms | Daytime sleepiness + night‑time insomnia limited to workdays | Persistent insomnia every night | Sleep onset/offset at abnormal times, may be chronic |
| Diagnosis Method | Sleep logs + schedule analysis | Clinical interview + polysomnography (if needed) | Actigraphy + melatonin profiling |
| Treatment Focus | Light therapy, schedule adjustment, CBT‑I | CBT‑I, sleep hygiene | Chronotherapy, melatonin timing |
Prevention: Building a Resilient Shift Schedule
Pre‑empting the disorder starts with smart scheduling. Forward‑rotating shifts allow the circadian system to gradually adapt, whereas backward rotations force a sudden phase advance. Limiting night‑shift length to 8-10hours, providing a 30‑minute bright‑light break every 3hours, and encouraging a post‑shift wind‑down routine lower the odds of chronic fatigue.
Employers can also invest in on‑site nap pods, educate staff about the importance of consistent sleep windows on off‑days, and monitor fatigue levels using brief self‑assessment tools (e.g., the Karolinska Sleepiness Scale).
When to Seek Professional Help
If excessive sleepiness leads to microsleeps at the wheel, if insomnia persists despite hygiene changes, or if mood symptoms (anxiety, depression) intensify, it’s time to involve a sleep specialist. Early intervention prevents long‑term health risks such as hypertension, type‑2 diabetes, and cardiovascular disease, which research from the American Academy of Sleep Medicine links to chronic shift work.
Quick Checklist for Night‑Shift Workers
- Track sleep‑wake times for at least two weeks.
- Expose yourself to bright light at shift start; wear blue‑light blockers on the way home.
- Reserve a dark, cool bedroom for daytime sleep.
- Consider a short‑acting stimulant or melatonin after consulting a clinician.
- Practice CBT‑I strategies: limit time in bed, keep the bedroom cue‑free.
- Talk to your manager about forward‑rotating schedules and nap breaks.
Adopting these habits can turn a draining night shift into a manageable part of your routine.
Frequently Asked Questions
What’s the difference between shift work disorder and regular insomnia?
Shift work disorder is tied to a work schedule that conflicts with the body’s internal clock, so symptoms appear mainly on workdays. Regular insomnia occurs every night, irrespective of work timing.
Can I cure shift work disorder without medication?
Yes. Light therapy, CBT‑I, strict sleep hygiene, and schedule adjustments can resolve most cases. Medication is reserved for severe or persistent symptoms after behavioral interventions.
How does light therapy actually shift my clock?
Bright light suppresses melatonin production, signaling the brain that it’s daytime. By timing exposure appropriately-usually at the start of a night shift-you push the circadian rhythm later, making you feel more awake during the shift.
Is it safe to use melatonin after a night shift?
Low‑dose melatonin (0.5‑3mg) taken immediately after the shift can help cue sleep. It’s generally safe, but anyone with hormonal disorders or on blood‑thinning medication should check with a doctor first.
My workplace won’t change my schedule-what can I do?
Focus on personal strategies: use a light box at the start of each shift, create a dark sleep environment, limit caffeine after the first half of the shift, and practice CBT‑I techniques. Consider discussing fatigue‑monitoring policies with HR.







14 comments
Joe Puleo
I've been a night-shift nurse for 12 years, and this is the first time I've seen a post that actually gets it right. Light therapy + blue-light blockers on the way home? Game changer. I started doing it last year and my sleep finally stuck. No more 3 a.m. panic wakes. Just pure, dumb, blessed sleep.
Keith Bloom
lol this is so basic. everyone knows you just need to drink more coffee and suck it up. my uncle worked 30 years on nights and never had a problem. you guys are just soft. also melatonin is just a supplement, not a drug, so stop acting like it’s magic. #truth
Ben Jackson
As a sleep tech, I’ve seen this play out a thousand times. The real win? CBT-I adapted for shift work. It’s not about sleeping more-it’s about sleeping *better* when your schedule is garbage. People underestimate stimulus control. Your bed = sleep only. No scrolling. No Netflix. No ‘just one more episode.’ That’s the secret sauce. Also, nap pods? Employer, please invest. Your ROI on reduced errors and absenteeism is insane.
Bhanu pratap
Bro, I’m a truck driver working 12-hour night shifts and I’ve been using this exact routine. Light box at 10 p.m., blackout curtains, melatonin 0.5mg after shift. I used to crash on the highway. Now I’m alive. I’m not saying it’s easy-but it’s possible. You’re not broken. You’re just fighting biology. And biology can be outsmarted. Stay strong. You got this.
Meredith Poley
Oh wow. A comprehensive, well-researched article that doesn’t say ‘just sleep more.’ Imagine that. The fact that this even needs to be explained in 2024 says everything about how little employers care. But hey, at least someone finally wrote it without emojis or ‘vibes.’ Progress.
Mathias Matengu Mabuta
While the article presents a phenomenological framework for circadian disruption, it fails to interrogate the structural determinants of labor exploitation inherent in 24/7 capitalism. The medicalization of shift work disorder obscures the political economy of sleep deprivation. Furthermore, the recommendation of modafinil as a pharmacological intervention constitutes a neoliberal co-optation of biological vulnerability. One must ask: who benefits from this narrative? The pharmaceutical-industrial complex, certainly. The worker? Perhaps not.
Ikenga Uzoamaka
WHY DO PEOPLE THINK THIS IS NORMAL?!?!?!!?!!? I WORK NIGHTS AND I’M TIRED ALL THE TIME AND NO ONE CARES!!! MY KID DOESN’T EVEN KNOW ME BECAUSE I’M SLEEPING WHEN SHE’S AWAKE AND WORKING WHEN SHE’S ASLEEP!!! THIS ISN’T A ‘DISORDER’-IT’S A CRIME!!!
Lee Lee
They told us light therapy works... but what if it’s all a lie? What if the ‘melatonin suppression’ is just a distraction from the real agenda? The government and Big Pharma want us to believe we can ‘hack’ our biology with gadgets and pills. But the truth? The circadian rhythm is a divine clock. Tampering with it leads to… well, you see the rise in depression, cancer, diabetes. They’re not treating the disorder-they’re masking the signal. The body is screaming. Are you listening?
John Greenfield
This article is dangerously misleading. CBT-I is not ‘gold standard’ for shift workers-it’s a placebo wrapped in jargon. I’ve studied sleep science for 20 years. The only thing that works is quitting your job. No amount of light boxes or melatonin fixes a system designed to break people. If you’re still working nights after reading this, you’re part of the problem.
Dr. Alistair D.B. Cook
Uhh... i think u missed something? like... the fact that most people dont have access to a light box? or a dark room? or even 8 hours to sleep? and cbt-i? lol. where am i supposed to find a therapist who understands shift work? my insurance covers 3 sessions a year. also... who the heck has time to do all this? i got two jobs and a kid. this article is for people who dont live in the real world.
Ashley Tucker
Wow. So now we’re giving medical advice to people who chose this lifestyle? I work a 9-to-5. I sleep at night. I don’t need a 10,000 lux lamp to function. Maybe if people stopped partying on their days off and actually respected their bodies, they wouldn’t need a whole damn handbook. This is just another excuse for laziness wrapped in science.
Allen Jones
Wait... so you’re telling me that if I use a blue-light blocker, I won’t be watched by the satellites that track my sleep patterns? 😳 I’ve been using them since 2020 and I’m pretty sure they’re still monitoring me. Also, is melatonin made from goat glands? I read a blog once... I think it’s a mind-control thing. 😵💫
jackie cote
Thank you for this clear, evidence-based overview. For those struggling, the most actionable step is to start a sleep log. Track your hours, light exposure, and caffeine intake for two weeks. Then bring it to your doctor. You don’t need to suffer silently. Your health is not negotiable.
Joe Puleo
^^^ This. I did exactly what jackie said. Wrote down every nap, every cup of coffee, every time I turned on a light. Saw a pattern: I was drinking coffee at 4 a.m. and then wondering why I couldn’t sleep at 8 a.m. Cut it off after 2 a.m. and boom-fell asleep 20 minutes faster. Small change. Huge difference.