Low Blood Sugar: Symptoms, Causes, and What to Do When It Happens
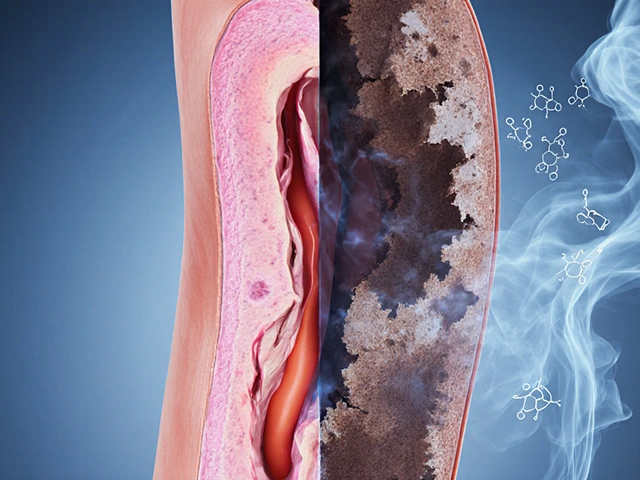
When your low blood sugar, a condition where glucose levels in the blood drop below normal, often triggering physical and mental symptoms. Also known as hypoglycemia, it can happen to anyone—but it’s most common in people with diabetes who take insulin or other glucose-lowering drugs. It’s not just about feeling shaky. Severe low blood sugar can lead to confusion, seizures, or even loss of consciousness if not treated quickly.
What causes it? Skipping meals, taking too much insulin, drinking alcohol on an empty stomach, or overdoing exercise without adjusting food or meds are common triggers. People on insulin, a hormone used to manage blood sugar in diabetes are especially at risk because their bodies don’t naturally balance the dose. Even those without diabetes can get low blood sugar from rare conditions like insulinomas or after gastric surgery. And it’s not always obvious—some people stop feeling the warning signs over time, which makes it even more dangerous.
Recognizing the early signs matters. Sweating, trembling, hunger, fast heartbeat, and dizziness are your body’s alarm system. If you ignore them, you might slip into confusion, blurred vision, or slurred speech. That’s when you need fast-acting sugar—glucose tablets, juice, or candy—not a meal. Wait too long, and you could need emergency help. People with diabetes should always carry a source of quick sugar and wear medical ID. Caregivers and family members should know how to use a glucagon kit if someone becomes unconscious.
It’s not just about treating the episode—it’s about preventing the next one. Tracking patterns helps. Did it happen after a workout? After skipping lunch? After changing your insulin dose? Writing it down gives you and your doctor real data to adjust your plan. Some newer closed-loop systems, automated insulin delivery devices that adjust doses based on real-time glucose readings are designed to reduce these episodes by predicting drops before they happen. But even without fancy tech, simple habits—eating regularly, checking blood sugar before driving or exercising, and never skipping snacks when on insulin—make a huge difference.
You’ll find real stories here from people who’ve dealt with this—how they learned to spot their own warning signs, what worked when they felt faint at work or school, and how they avoided emergencies. Some posts dig into how certain medications, like metformin or sulfonylureas, can contribute to drops. Others show how diet, timing, and even stress play roles. You’ll also see how people manage low blood sugar while traveling, sleeping, or dealing with other health issues like kidney disease or thyroid problems. This isn’t just theory. These are practical lessons from real lives.

- Dec 4, 2025
- Posted by Cillian Osterfield
Managing Hypoglycemia from Diabetes Medications: A Practical Step-by-Step Plan
Learn how to prevent and treat low blood sugar caused by diabetes medications like insulin and sulfonylureas. This practical guide covers risk factors, emergency treatment, tracking patterns, and new technologies to stay safe.
Categories
- Health and Wellness (72)
- Medications (70)
- Health and Medicine (28)
- Pharmacy Services (12)
- Mental Health (9)
- Health and Career (2)
- Medical Research (2)
- Business and Finance (2)
- Health Information (2)
Latest Posts
©2026 heydoctor.su. All rights reserved