When your pharmacist hands you a pill that looks nothing like the one you’ve been taking, it’s normal to feel uneasy. The color’s different. The shape’s off. Even the name on the bottle changed. You’re not alone. Millions of people switch from brand-name drugs to generics every year-mostly because it saves money. But what really happens when you make the switch? Is it safe? Will it still work? And why do some people have problems while others don’t?
Generics aren’t knockoffs-they’re exact copies, legally
The U.S. Food and Drug Administration (FDA) doesn’t allow generic drugs to be "similar" to brand-name ones. They have to be identical in active ingredient, strength, dosage form, and how fast they work in your body. The only things that can differ are the color, shape, flavor, or inactive ingredients like fillers or dyes. That’s why your new pill might be white and oval instead of blue and round. It’s still the same medicine inside.
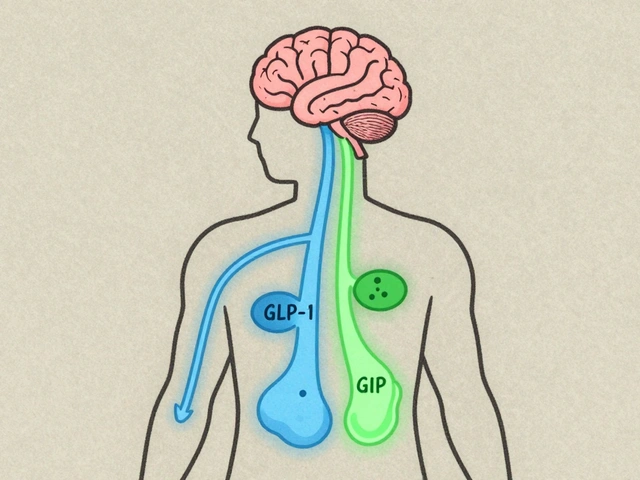
Before a generic can hit the market, the manufacturer must prove it delivers the same amount of active drug into your bloodstream at the same rate as the brand. This is called bioequivalence. The FDA requires the generic’s absorption to fall within 80% to 125% of the brand’s. That’s a tight range. It’s not a guess-it’s science. Over 90% of all prescriptions filled in the U.S. are for generics, and they’ve saved the system over $370 billion since the 1980s.
Cost savings are real-sometimes life-changing
Let’s say you take a blood pressure pill that costs $120 a month as a brand. The generic version? $12. That’s not a typo. The 2019 Association for Accessible Medicines report found that 90% of generic copays are under $20, while only 39% of brand-name copays are that low. For people on fixed incomes, that difference isn’t just convenient-it’s the reason they can afford to keep taking their medicine at all.
One study showed that patients were 266% more likely to abandon a brand-name prescription because of cost. That means they didn’t fill it, skipped doses, or stopped entirely. That’s dangerous. High blood pressure, diabetes, or thyroid conditions don’t wait for you to afford the right pill. Switching to generic often means starting-or continuing-treatment. That’s why many insurers now refuse to cover brand-name drugs unless your doctor specifically says "dispense as written."
But not all drugs are created equal-some switches can backfire
For most medications, switching is smooth. But for drugs with a narrow therapeutic index, even tiny differences in how your body absorbs the drug can cause problems. These are drugs where the difference between a therapeutic dose and a toxic one is small.
Anti-seizure medications are the most documented case. Studies show that some patients with epilepsy experience more seizures after switching to a generic version-even though the active ingredient is the same. Why? Because small changes in absorption can push blood levels just outside the safe range. One patient reported their TSH level (a thyroid marker) jumped from 2.5 to 8.7 after switching from Synthroid to generic levothyroxine. That’s a big change. Their doctor had to switch them back.
Warfarin (a blood thinner), certain thyroid meds, and some psychiatric drugs are also in this high-risk group. That’s why doctors often write "dispense as written" on prescriptions for these. It’s not about trusting generics less-it’s about controlling variables in treatments where precision matters.

Why do some people feel worse after switching?
If you feel different after switching, it’s not always in your head. Here are the real reasons:
- Inactive ingredients: Fillers, dyes, or preservatives can cause reactions in sensitive people. One person might get a rash from a dye in one generic brand but not another.
- Appearance changes: If your pill looks different every time you refill, you might think you got the wrong medicine. That confusion can lead to skipped doses or anxiety.
- Multiple switches: In some countries, like Saudi Arabia, the government changes which generic manufacturer supplies the drug every year based on bidding. That means you might switch from Generic A to Generic B to Generic C-all with different looks and fillers. One study found over 25% of medications switched between brand and generic versions in just five years. That’s a lot of confusion.
- Psychological effect: If you believe generics are inferior, your body might react to that belief. But that doesn’t mean the drug isn’t working-it means your mind is part of the treatment.
Massachusetts, where law requires pharmacies to substitute generics unless the doctor says otherwise, did a patient survey. Sixty-three percent were worried at first. But after three months, 82% said they were satisfied. The key? Education. When patients understood why the pill looked different, they relaxed.
What you can do before and after switching
You don’t have to just accept a switch. Here’s how to take control:
- Ask your doctor: If you’re on a high-risk medication (epilepsy, thyroid, blood thinners, etc.), ask if switching is safe. Say: "Can we keep me on the brand, or should I monitor closely?"
- Check the label: Every time you get a refill, look at the name of the manufacturer. If it changes, that’s normal-but note it. Some pharmacies put stickers on bottles to warn you about appearance changes.
- Track symptoms: Keep a simple log: date, dose, how you feel, any side effects. If you notice a pattern-more headaches, mood swings, dizziness-bring it to your doctor.
- Don’t panic if it feels off: Give it two to four weeks. Your body needs time to adjust. But if symptoms are severe or you’re having new health issues, call your provider. Don’t wait.
- Use the same pharmacy: If you stick with one pharmacy, they’re more likely to notice if your generic switches manufacturers unexpectedly. They can flag it for you.

When to ask for the brand name
You have the right to ask for the brand-name drug-even if it costs more. You just might have to pay the difference. Here are situations where it makes sense:
- You’ve had a bad reaction to a generic version before.
- You’re on a narrow therapeutic index drug and your levels have been stable on the brand.
- Your doctor recommends it based on your history.
- You’re switching and feel worse after two weeks.
Some patients who switched back to brand-name levothyroxine or epilepsy meds after problems with generics saw their symptoms improve quickly. That’s not rare. It’s evidence that individual biology matters.
What’s changing on the horizon
Experts are pushing for better systems. One idea? Lengthen procurement contracts so pharmacies don’t switch generic manufacturers every year. Another? Standardize pill appearance across manufacturers for high-risk drugs. Imagine if every generic levothyroxine looked the same, no matter who made it. That would cut down on confusion.
Also, more insurers are starting to cover brand-name drugs if you’ve had a documented issue with generics. It’s not common yet-but it’s growing.
The bottom line? Generics are safe and effective for most people. But medicine isn’t one-size-fits-all. Your body, your history, and your symptoms matter more than the label on the bottle.
If you’re switching, don’t assume it’s automatic. Ask questions. Track changes. Speak up if something feels off. You’re not being difficult-you’re being smart.
Are generic drugs as effective as brand-name drugs?
Yes, for most people and most medications. The FDA requires generics to have the same active ingredient, strength, and absorption rate as the brand. Over 90% of prescriptions in the U.S. are generics, and they’ve saved billions without a drop in overall public health. But for drugs with a narrow therapeutic index-like anti-seizure meds, thyroid pills, or blood thinners-even small differences in absorption can matter. In those cases, some patients do better on the brand.
Why do generic pills look different?
Trademark laws prevent generic manufacturers from making their pills look exactly like the brand. So they change the color, shape, or size. That’s why your pill might be white instead of blue, or oval instead of round. The inside is the same-but the outside isn’t. Some pharmacies put stickers on the bottle to warn you about appearance changes.
Can switching to a generic cause side effects?
Rarely, but yes. Side effects can come from inactive ingredients like dyes or fillers, which vary between manufacturers. Some people are sensitive to these. Also, if you’re on a drug where precise blood levels matter-like warfarin or levothyroxine-switching between different generics can cause your levels to shift slightly, leading to new symptoms. That’s why tracking how you feel after a switch is important.
Should I always choose the cheapest generic?
Not always. If you’re on a high-risk medication, ask your doctor if there’s a specific generic brand that works best for you. Some pharmacies carry multiple generics for the same drug, and one might work better than another. If you’ve had a problem with one generic, stick with the one that worked before-even if it’s slightly more expensive.
What if my insurance won’t cover the brand-name drug?
Your doctor can file an exception request with your insurer, especially if you’ve had a bad reaction to generics or your condition is unstable. Many insurers approve these requests for drugs like levothyroxine, epilepsy meds, or blood thinners. Don’t assume it’s impossible-ask your doctor to help you navigate it.
Is it safe to switch back and forth between brand and generic?
Frequent switching-especially between different generic manufacturers-isn’t recommended, especially for drugs with a narrow therapeutic index. Each switch could change how your body absorbs the drug. If you’re stable on one version, stay with it. If you must switch, do it once and monitor closely. Avoid cycling between versions unless your doctor advises it.
Final thought: Trust your body, not just the label
Generics are a win for the system-and for your wallet. But your health isn’t a spreadsheet. If you feel different after a switch, it’s not weakness. It’s information. Pay attention. Talk to your doctor. Keep a record. You know your body better than any algorithm or insurance policy. The goal isn’t to avoid generics-it’s to use them wisely. And sometimes, that means choosing the brand.






9 comments
Terri Gladden
so i switched to generic levothyroxine and suddenly i was crying in the shower for no reason and my hair was falling out like a bad 90s telenovela??? my doctor said "it's probably just stress" but i know better. i think the filler is made of pure despair and i'm pretty sure the pill company is secretly run by Big Pharma ghosts.
en Max
It is imperative to underscore, with the utmost scientific rigor, that bioequivalence, as defined by the FDA’s 80–125% confidence interval for Cmax and AUC0–t, constitutes a statistically validated threshold for therapeutic interchangeability. The variance in inactive excipients, while pharmacologically inert in the majority of cases, may precipitate idiosyncratic reactions in susceptible populations, particularly those with IgE-mediated hypersensitivities or compromised metabolic pathways.
Jacob Milano
Man, I used to freak out every time my pill changed color-purple one day, white the next. Then I started keeping a little notebook: ‘Day 3: no dizziness. Day 7: sleep’s better.’ Turns out, my body just needed a chill pill (literally). Generics aren’t magic, but neither are brand names. It’s all about tuning in to your own rhythm.
Allen Ye
What we’re really discussing here is the commodification of human biology under late-stage capitalism. The pill you swallow is not merely a molecule-it is a symbol of systemic cost-cutting, of corporate arbitrage, of the erasure of patient autonomy in favor of algorithmic efficiency. The FDA’s 80–125% window isn’t science-it’s a compromise forged in the fires of profit. And yet, we are told to trust. To adapt. To normalize the instability. But when your thyroid levels swing like a pendulum in a haunted house, who is really being served? The system? Or the person who just wants to feel human again?
mark etang
Adopting generic medications is a responsible, fiscally prudent decision that aligns with the principles of sustainable healthcare delivery. The savings generated enable broader access, reduce patient abandonment rates, and promote adherence. It is incumbent upon patients to collaborate with their providers and exercise diligence in monitoring outcomes.
Brendan F. Cochran
generic drugs are just the government’s way of making us sick so they can sell us more meds. they change the pills so you can't tell if you're getting the real stuff. i heard the FDA gets kickbacks from the big pharma companies that make the generics. also, why do all the pills look like they were designed by a 5-year-old? i'm not taking that crap.
jigisha Patel
While anecdotal reports of adverse reactions are documented, the aggregate data from over 12,000 controlled studies indicate no clinically significant difference in therapeutic efficacy between brand and generic formulations. The perceived variability is largely attributable to confirmation bias and the nocebo effect. Patients exhibiting non-adherence following generic substitution should undergo psychological evaluation rather than pharmacological reversion.
Jason Stafford
They're watching us. Every time you take a generic, they track your blood levels through the pill’s nano-chip. That’s why your thyroid spikes after a switch-it’s not the filler, it’s the surveillance. They want us dependent on the system. The color changes? That’s the algorithm recalibrating your mood. And don’t get me started on the pharmacy stickers-they’re coded messages. Wake up.
Justin Lowans
There’s something beautiful about how medicine can be both a science and a deeply personal journey. The pill might look different, but if you’re feeling stable, grounded, alive-that’s the real active ingredient. I’ve seen people terrified of switching, then years later say, ‘I wish I’d done it sooner.’ Trust your body, yes-but also trust that you’re not alone in this. You’ve got this.