Have you ever stopped a medication because you felt worse after starting it-only to wonder if the drug was really to blame? Many people assume that if symptoms appeared after taking a pill, the pill must be the cause. But that’s not always true. Sometimes, other factors are at play. That’s where dechallenge and rechallenge come in. These aren’t fancy medical jargon-they’re simple, real-world tests doctors use to figure out if a drug actually caused a side effect.
What Is Dechallenge?
Dechallenge is the first step in confirming whether a drug caused a bad reaction. It’s simple: you stop taking the suspected medication and watch what happens. If the side effect gets better-or disappears-within a reasonable time, that’s called a positive dechallenge. It suggests the drug was likely responsible.For example, imagine someone develops a painful, itchy rash two weeks after starting a new antibiotic. Their doctor tells them to stop the drug. Within five days, the rash fades. That’s a classic positive dechallenge. The timing matters. If the reaction clears in line with how long the drug stays in the body (its half-life), it strengthens the case. A drug like metronidazole, which leaves the system in about 8 hours, shouldn’t cause symptoms to linger for weeks after stopping. If they do, something else might be going on.
But not all dechallenge results are clear-cut. Sometimes, symptoms improve slowly, or only partially. Maybe the rash fades but leaves dark spots behind. That’s still useful information. Even partial improvement counts as a positive dechallenge. What doesn’t count is if symptoms stay the same or get worse after stopping the drug. That’s a negative dechallenge, and it suggests the drug probably didn’t cause the issue-or the damage is already permanent.
What Is Rechallenge?
Rechallenge is the next step-when doctors consider giving the drug back, on purpose, to see if the reaction returns. This is the gold standard for proving causality. If the same side effect comes back, exactly as before, you can be almost certain the drug caused it.One well-documented case involved a patient who developed a fixed-drug reaction: a blistering rash that always appeared in the same spot on the leg after taking metronidazole. After stopping the drug, the rash cleared. Months later, under strict medical supervision, the doctor gave the drug again. Within 48 hours, the exact same rash reappeared in the same spot. That’s rechallenge in action. It’s not just correlation-it’s confirmation.
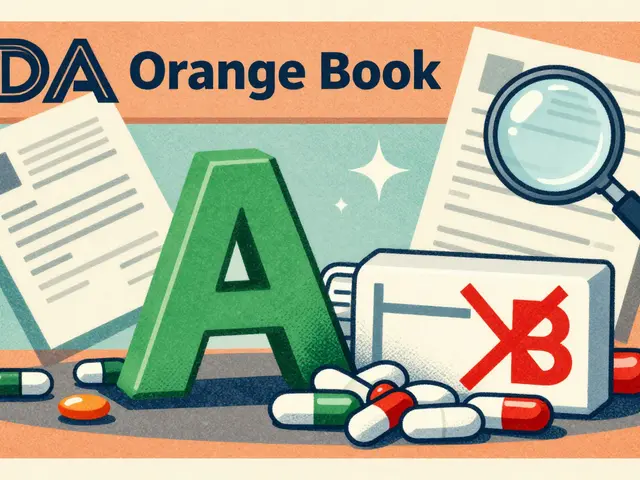
But here’s the catch: rechallenge is risky. If the reaction was severe-like liver failure, Stevens-Johnson syndrome, or anaphylaxis-re-exposing a patient is dangerous, even life-threatening. That’s why it’s rarely done. In dermatology, where skin reactions are common, rechallenge is used in fewer than 15% of cases. In psychiatry, where stopping meds can trigger relapse, it’s even rarer. Regulatory agencies like the FDA only approve rechallenge in about 0.3% of serious adverse event investigations, and only under tight controls: with ethics board approval, full informed consent, and emergency care ready.
Why These Tests Matter More Than You Think
You might think doctors just guess which drug caused a side effect. But they don’t. They use a four-part framework to assess causality:- Temporal relationship: Did the reaction happen after taking the drug? (Timing matters.)
- Dechallenge: Did symptoms improve after stopping it?
- Rechallenge: Did symptoms return when the drug was restarted?
- Biological plausibility: Does this reaction match what’s known about the drug’s effects?
Dechallenge and rechallenge are the only parts of this framework that give clinical proof. The rest are clues. Temporal relationship? A heart attack could happen right after taking a new pill-but that doesn’t mean the pill caused it. Maybe the patient was already having a heart attack. Biological plausibility? We know some antibiotics can cause diarrhea, but that doesn’t mean every case of diarrhea on antibiotics is from the drug.
That’s why dechallenge alone is rated as “probable” causality on most scales. Rechallenge? It bumps it to “definite.” Studies show that when rechallenge is successfully performed, 97% of cases meet the WHO-UMC’s highest causality rating. No algorithm, no statistical tool, no AI model can match that level of certainty.

Why Rechallenge Is So Rare
Even though rechallenge gives the clearest answer, it’s not used often-and for good reason.First, ethics. Giving a drug back to someone who had a dangerous reaction is like playing Russian roulette with their health. If the reaction was mild-like a rash or mild nausea-it might be worth it. But if it was life-threatening? Almost never done.
Second, practicality. Many patients stop their meds on their own without telling their doctor. That’s not a real dechallenge-it’s just self-discontinuation. Without a controlled stop, you can’t be sure the reaction was tied to the drug. Also, if someone is taking five different medications, stopping them all at once makes it impossible to know which one caused the problem.
Third, timing. If the reaction happened six months ago, you can’t easily rechallenge. The patient may have moved, changed doctors, or forgotten details. The window to confirm causality is narrow.
How Technology Is Changing the Game
New tools are emerging to make dechallenge and rechallenge safer and more accurate.Wearable sensors now track heart rate, skin temperature, and inflammation markers in real time as patients stop a drug. This gives doctors objective data instead of relying on how the patient feels. In one study, sensors caught resolution of symptoms in 78% of cases, compared to just 52% with patient reports alone.
There’s also progress in lab-based alternatives. Scientists can now test a patient’s blood cells in a dish to see if they react violently to a specific drug. These lymphocyte toxicity assays predict adverse reactions with 89% accuracy. That means doctors might soon avoid rechallenge entirely for high-risk patients.
Machine learning is being trained to predict whether a reaction will resolve after dechallenge, based on past cases. Early models can forecast recovery timelines with 76% accuracy. But experts agree: no algorithm replaces the real thing. As Dr. Elena Rodriguez from the WHO put it, “No algorithm can substitute for the clinical reality of symptom resolution after drug discontinuation.”
What This Means for You
If you’ve had a bad reaction to a medication, don’t assume you know the cause. Talk to your doctor about dechallenge. Did your symptoms improve after stopping the drug? When? How much? Keep a simple log: date you started, date you stopped, when symptoms began, when they eased. That’s invaluable information.If your doctor suggests rechallenge, ask why. Is it safe? What are the risks? What happens if the reaction comes back? Make sure you understand the trade-offs. Most of the time, you won’t need it. But when you do, it’s the most powerful tool doctors have to prove what caused your reaction.
For the pharmaceutical industry, this isn’t just academic. Regulatory agencies require dechallenge data in every safety report. Companies use it to update drug labels, warn other doctors, and avoid lawsuits. That’s why electronic health records now have specific fields to document dechallenge outcomes. It’s not just about your health-it’s about protecting future patients too.
When Dechallenge and Rechallenge Don’t Work
These tests aren’t perfect. Some reactions are irreversible. Think of drug-induced liver scarring or permanent nerve damage. Stopping the drug won’t undo that. In those cases, dechallenge is negative-not because the drug didn’t cause it, but because the damage is done.Some reactions are delayed. A drug might trigger a reaction months later, making dechallenge hard to link. Others are masked by other conditions. A patient on multiple drugs might stop one, but the side effect persists because another drug is still in play.
And sometimes, the reaction is psychological. If someone believes a drug causes side effects, they might feel worse just from stopping it-what’s called a nocebo effect. That’s why objective measures, like lab tests or wearable sensors, are becoming more important.
When all else fails, doctors use tools like the Naranjo Scale, which scores likelihood based on timing, dechallenge results, and other factors. But even this tool gives probabilities-not proof. Only dechallenge and rechallenge deliver certainty.
Can I try rechallenge on my own if I think a drug caused my side effect?
No. Never restart a medication that caused a bad reaction without medical supervision. Rechallenge is only done in controlled settings with emergency care available. Doing it on your own could be life-threatening, especially if the reaction was serious like swelling, breathing trouble, or liver damage.
If my symptoms improved after stopping a drug, does that mean it definitely caused them?
Not always. A positive dechallenge suggests the drug was likely the cause, but it’s not 100% proof. Other factors could have improved at the same time-like stress, diet, or another medication you also stopped. Doctors look at the full picture: timing, biological plausibility, and whether the reaction matches known side effects of the drug.
Why do some doctors never use rechallenge?
Because it’s risky. For reactions that could be fatal-like anaphylaxis, toxic epidermal necrolysis, or drug-induced liver failure-rechallenge is considered unethical. Even for milder reactions, many doctors avoid it because the risk outweighs the benefit, especially when alternatives like lab tests or AI models are available.
How long should I wait after stopping a drug to see if dechallenge worked?
It depends on the drug and the reaction. For skin rashes, improvement usually shows in 3-10 days. For liver or kidney issues, it might take weeks. For drugs with a short half-life (like ibuprofen), symptoms should improve within a day or two. For drugs that stay in the body longer (like fluoxetine), it could take 2-3 weeks. Your doctor will guide you based on the drug’s pharmacokinetics.
Is dechallenge and rechallenge used for all types of drug side effects?
No. They’re most commonly used in dermatology, hepatology, and immunology-areas where reactions are clear and measurable. In psychiatry, neurology, or chronic pain management, stopping a drug might cause relapse or withdrawal, so these tests are avoided. Instead, doctors rely on other tools like Naranjo scoring or pharmacogenomic testing.
Final Thought: It’s Not Guesswork-It’s Science
Dechallenge and rechallenge aren’t just medical tricks. They’re the backbone of drug safety. Every time a drug label gets updated with a new warning, or a medication is pulled from the market, it’s often because someone went through this process. Someone stopped the drug. Someone got better. And sometimes, someone let the drug back in-carefully, safely-and saw the reaction return. That’s how we know what’s truly dangerous.For you, it means your experience matters. If you’ve had a side effect, document it. Talk to your doctor. Ask about dechallenge. You’re not just a patient-you’re part of the system that keeps drugs safe for everyone else.







8 comments
John Chapman
OMG YES THIS!! I stopped my antibiotic for a rash and it vanished in 3 days 😍 I told my doctor it was probably the drug but they were like 'maybe it's stress'... nope. Classic positive dechallenge. Now I log everything. No more guessing. 🙌
Urvi Patel
Dechallenge and rechallenge are just fancy ways of saying 'did it get better when you stopped' and 'did it come back when you tried again' why do we need medical jargon for common sense? Also rechallenge is basically medical Russian roulette and no one should ever do it unless they're desperate or dumb
anggit marga
USA doctors think they invented this lol in Nigeria we've been doing this since the 80s with traditional meds and herbal mixtures no fancy sensors needed just observation and common sense if your headache goes away after stopping the bitter root you know it was the root
Joy Nickles
Okay but like… what if you stop the drug and your anxiety spikes because you’re terrified you’re dying from the side effect?? Like I stopped sertraline and felt like I was having a heart attack but it was just withdrawal?? And then I restarted it and it was fine?? So is that rechallenge or just panic?? Also I think doctors are lazy and don’t want to admit they misdiagnosed you so they say ‘dechallenge was negative’ when really you just needed a different dose??
Emma Hooper
Let me tell you something wild-dechallenge is the only real-world placebo control we’ve got in pharmacology. You don’t need double-blind trials when your body gives you a live demo. I had a friend who got hives from naproxen. Stopped it? Gone in 48 hours. Tried it again? Hives returned like clockwork. No lab. No AI. Just her skin and a pill. That’s science in its purest form. And yeah, rechallenge is risky-but so is letting people suffer under mislabeled side effects because doctors are scared to ask the right questions. If you’ve had a reaction, document it. Not for the FDA-for yourself. Your body remembers. Trust it.
Marilyn Ferrera
Rechallenge is the gold standard. But only when it’s ethical. And only when the patient is fully informed. And only when emergency care is on standby. And only when the reaction isn’t life-threatening. And only when the drug has no alternatives. And only when the timeline is clear. And only when the patient hasn’t moved three states away. And only when the doctor isn’t overworked. So… rarely.
Aaron Bales
Wearables are game-changers. I had a patient with a drug-induced arrhythmia. We stopped the med, and her heart rate normalized within 12 hours-confirmed by her Fitbit. No guesswork. That’s the future. Also, if you’re on five meds, don’t stop them all at once. That’s not dechallenge, that’s chaos. One at a time. Patience.
Lawver Stanton
Look, I get it. Dechallenge sounds smart. Rechallenge sounds like something out of a horror movie. But here’s the truth: 90% of the time, doctors don’t even do dechallenge properly. They just say, 'Oh, you stopped the drug and felt better? Cool, probably that.' No timeline. No log. No follow-up. Meanwhile, patients are left wondering if they’re crazy. And then they go on Reddit and post 2000-word essays about how their hair fell out after taking vitamin D (spoiler: it didn’t). Meanwhile, the real cases-the ones where someone gets SJS from a single pill and lives to tell the tale-get buried under a mountain of self-diagnosed nonsense. Technology helps. But the real problem? We treat drug reactions like a game of Whac-A-Mole instead of a science. And until we stop treating patients like walking symptom lists, we’re just spinning our wheels.