Pediatric Fluid Intake Calculator
This tool helps estimate the recommended daily fluid intake for children to support healthy bowel function and prevent constipation.
Recommended Daily Fluid Intake:
Enter your child's weight and click calculate.
Why This Matters:
Proper hydration helps keep stools soft and easy to pass. According to the article, children should drink approximately 1 liter of fluid per 10 kg of body weight daily.
When it comes to kids, a stubborn bowel habit can feel like an endless mystery. Chronic idiopathic constipation in children is a condition where a child experiences hard, infrequent stools for at least three months without an identifiable medical cause. In plain English, "idiopathic" means doctors haven’t found a disease or anatomical issue that explains the problem. This article walks you through the red flags, typical symptoms, and evidence‑based ways to get things moving again.
- Watch for fewer than three bowel movements per week or hard pellets that resist passing.
- Look for abdominal pain, bloating, or a feeling of incomplete evacuation.
- Know the first‑line treatments: dietary tweaks, adequate fluids, and safe laxatives.
- Understand when a specialist’s evaluation is needed - especially if pain is severe or growth stalls.
- Learn long‑term strategies to keep constipation from returning.
Red‑Flag Signs Parents Should Not Ignore
Kids often can’t articulate what’s wrong, so you become the detective. The most reliable sign is a change in stool frequency. If your child goes longer than three days without a bowel movement, start logging the pattern. Other warning signs include:
- Hard, stone‑like stools that need a lot of effort to pass.
- Visible blood on toilet paper - a sign of anal fissures from straining.
- Frequent abdominal cramps, especially after meals.
- Loss of appetite or nausea caused by a backed‑up gut.
- Behavioral changes - irritability, clutching the abdomen, or avoidance of school bathroom breaks.
These clues often point to chronic idiopathic constipation, but they can also signal other issues. When you see any of them, a quick chat with your child’s pediatrician is the safest first step.
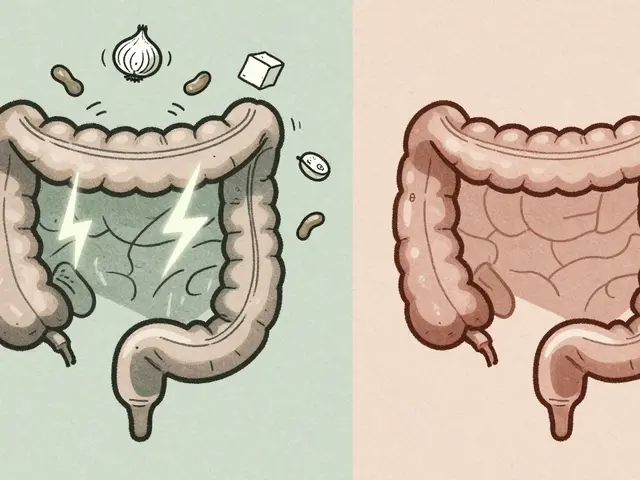
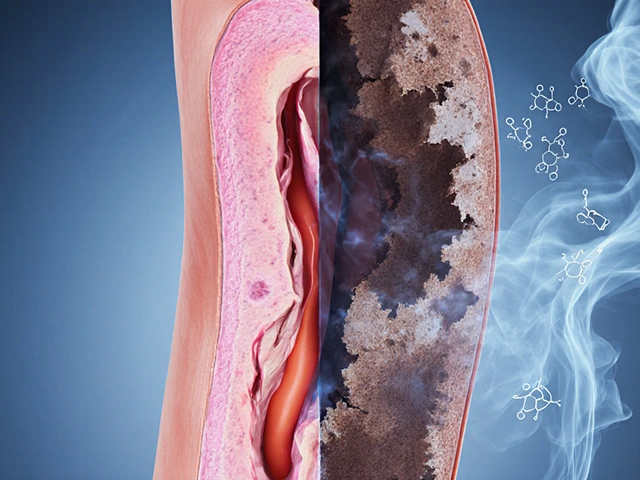
Common Symptoms and How They Evolve
The symptom picture can shift as the condition lingers. Early on, you might notice occasional discomfort and a few missed poops. Over weeks, the colon adapts by pulling more water out of stool, making it even drier. This creates a vicious cycle: harder stools lead to more straining, which can damage the anal muscles and further slow transit.
Typical symptoms include:
- Infrequent bowel movements (fewer than three per week).
- Hard, lumpy stools that look like peanuts.
- Abdominal bloating that can make the belly look distended.
- Feeling of incomplete emptying, often described as “still need to go.”
- Occasional leakage of liquid stool (so‑called “overflow incontinence”).
If any of these persist beyond three months, the condition meets the definition of chronic idiopathic constipation according to the Rome IV criteria. The criteria help doctors standardize diagnosis across clinics.
Why Does It Happen? (Understanding the ‘Idiopathic’ Part)
Even when doctors can’t pinpoint a disease, several factors commonly contribute:
- Low dietary fiber - fiber adds bulk and pulls water into the stool.
- Insufficient fluid intake - water is the lubricant that keeps stool soft.
- Fear of painful bowel movements leads kids to hold stool, letting the colon reabsorb more water.
- Pelvic floor dysfunction - the muscles that should relax during a pooping attempt stay tight.
- Gut microbiota imbalance; some studies show probiotics can help restore balance.
Because no single cause dominates, treatment focuses on correcting each contributing factor.

How Doctors Diagnose the Problem
Diagnosis starts with a thorough history and a physical exam. Pediatricians may ask about:
- Stool diary (frequency, consistency, any pain).
- Dietary patterns - how much fruit, vegetables, and water the child drinks.
- Medication use (e.g., antihistamines or iron supplements can worsen constipation).
If red flags such as severe abdominal pain, weight loss, or blood in stool appear, the doctor might order imaging or labs. Common investigations include:
- Abdominal X‑ray to look for fecal loading.
- Colonic transit study - a specialized test that tracks how long stool takes to move through the colon.
- Rectal exam - to check for muscle tone and rule out anatomical blockage.
In most cases, the diagnosis rests on history, physical findings, and meeting the Rome IV threshold.
Treatment Options: What Works Best?
Below is a quick‑look comparison of the most common approaches. The goal is to soften stool, establish a regular rhythm, and break the fear‑of‑pain cycle.
| Approach | How It Works | Typical Dose (Kids) | Pros | Cons / Cautions |
|---|---|---|---|---|
| Increased dietary fiber | Adds bulk, retains water | 5‑10g per day per 10kg body weight | Natural, no side effects | May cause gas if increased too quickly |
| Fluid optimization | Hydrates stool matrix | 1L per 10kg weight (adjust for activity) | Simple, cheap | Requires vigilance at school |
| Osmotic laxatives (e.g., polyethylene glycol (PEG)) | Draws water into colon | 0.4g/kg once daily | Highly effective, safe long‑term | May cause mild bloating |
| Stimulant laxatives (e.g., bisacodyl) | Triggers intestinal contractions | 0.1‑0.2mg/kg as needed | Works fast for breakthrough cases | Potential for dependence if overused |
| Behavioral therapy / toilet training | Teaches child to relax pelvic floor | 3‑times‑weekly sessions for 4‑6weeks | Addresses underlying fear | Requires consistent parental involvement |
| Probiotic supplementation | Modulates gut microbiota | 1‑2billion CFU daily | May improve stool frequency | Evidence still emerging |
Most pediatric guidelines start with fiber, fluids, and an osmotic laxative like PEG. If stool still resists, a short course of a stimulant can break the stalemate. Behavioral therapy shines when fear of pain keeps the child holding stool.
Practical Home Management Tips
Even after a doctor prescribes a plan, daily habits make or break success. Try these simple tricks:
- Set a regular “toilet time” after meals - the gastrocolic reflex naturally stimulates the colon.
- Use a footstool so knees are higher than hips; this position straightens the rectum.
- Offer high‑fiber snacks like apple slices, berries, or whole‑grain crackers.
- Keep a water bottle handy at school; refill it often.
- Reward the child for successful bathroom trips with stickers, not candy.
Consistency is key. A child can feel better within days, but establishing a habit takes a few weeks.
When to Call a Pediatric Gastroenterologist
Most cases improve with primary‑care guidance, but be ready to seek specialist care if you notice any of the following:
- Severe abdominal pain that wakes the child at night.
- Weight loss or stalled growth on the growth chart.
- Visible blood in stool that doesn’t stop.
- No response to PEG after two weeks of proper dosing.
- Signs of megacolon on an X‑ray (extreme dilation of the colon).
Specialists can run advanced testing, prescribe prescription‑strength meds, and coordinate biofeedback therapy for pelvic floor dysfunction.

Frequently Asked Questions
How long does it take for a laxative like PEG to work?
Most children notice softer stools within 24‑48hours. Full regularity often appears after three to seven days of consistent dosing.
Can constipation cause urinary problems?
Yes. A full colon can press on the bladder, leading to frequent urges or nighttime bedwetting. Treating constipation often resolves the urinary symptoms.
Is it safe to give my child over‑the‑counter laxatives long‑term?
Osmotic agents like PEG have a solid safety record for long‑term use under pediatric supervision. Stimulant laxatives should be limited to short bursts because of dependence risk.
My child refuses to sit on the toilet. What can I do?
Make bathroom time fun and low‑pressure. Use a timer for 5‑minute sessions, play a favorite song, and praise effort rather than outcome. If fear persists, a brief session with a child therapist can help.
Do probiotics really help?
Research shows certain strains (e.g., Bifidobacterium infantis) can improve stool frequency in some kids, but results vary. They’re a safe adjunct, especially if your child has taken antibiotics recently.





18 comments
Faith Leach
Wake up, folks! The pharma giants are using these "fluid calculators" to push sugary drinks while pretending it's health advice. They hide the real agenda behind cute graphics and a friendly tone. Don't be fooled by the slick marketing.
Eric Appiah Tano
Hey everyone, great tool for figuring out how much water kids need each day. Just plug in the weight and you get a solid baseline. Staying hydrated really does keep stools soft and eases constipation. Keep an eye on juice intake though – too much can backfire.
steve wowiling
Honestly, this calculator feels like a philosophical experiment – "What is fluid?”? Kids will ignore the numbers and go straight for soda. The drama of a kid’s thirst is far more complex than a simple formula.
Kelly Aparecida Bhering da Silva
America's health crisis is invisible until you look at the numbers, and this tool proves it. Kid after kid is dehydrated because schools push sugary snacks over water. We need to demand real change, not just a cute widget.
Michelle Dela Merced
Totally agree! 💧💪 The more we hydrate, the stronger our kids become. Let's flood the schools with water fountains and ban the soda machines! 🚰✨
Mark Conner
Kids need more water, period.
Charu Gupta
Proper hydration is essential for gastrointestinal motility; insufficient fluid intake can exacerbate constipation. Please ensure your child drinks the recommended amount daily.
Abraham Gayah
Wow, another calculator? Like we need a PhD to figure out how much water to drink. This is absurdly over‑engineered.
Caley Ross
Honestly, I think it's fine. If parents use the tool, it might help them keep track without stress. It's just another option.
George Frengos
Great job on making this accessible! Encouraging kids to sip water throughout the day can be a game‑changer for bowel health. Let’s spread the word and keep the momentum going.
Jonathan S
While the intentions are noble, many parents still overlook basic nutrition principles. It’s not enough to hand over a calculator and expect miracles; consistent habits matter more. Moreover, the over‑reliance on technology can distract from real education about food and fiber. Let’s remember that water is only one piece of the puzzle. 🙄
Charles Markley
From a bio‑psycho‑social perspective, fluid dynamics intersect with enteric neural pathways, modulating peristaltic efficacy. Inadequate intake precipitates osmotic imbalances, leading to increased colonic transit time. Thus, quantifying hydration is not merely a convenience but a clinical imperative.
L Taylor
Water is a basic need its not rocket science we all know kids need it keep them drinking don't overthink it
Matt Thomas
i cant believe people still need a fancy tool for water dont just knw the basics!
Craig Stephenson
Let’s keep the conversation positive! Small steps, like a water bottle on the bedside table, can make a big difference. Together we can help kids stay healthy and happy.
Jonathan Lindsey
Ah, the noble pursuit of quantifying hydration for our young progeny – a task most fitting for the modern parent armed with a calculator and a smirk. One must first acknowledge the sheer audacity of assuming that a mere numeric output can resolve the labyrinthine complexities of pediatric constipation, a condition steeped in multifactorial etiology.
Nonetheless, let us proceed, for the sake of thoroughness; first, the recommended intake of approximately one liter per ten kilograms is, in fact, a well‑established guideline derived from rigorous epidemiological studies, not some capricious internet meme.
Second, the tool’s user‑friendly interface, boasting generous padding and a verdant #4CAF50 border, serves to distract the weary caregiver from the underlying pathophysiology, a clever tactic indeed.
Third, one must consider the role of dietary fiber – a component conspicuously absent from the calculator’s scope, yet vital for augmenting stool bulk and reducing transit time.
Fourth, the importance of establishing regular bathroom routines cannot be overstated; a child who learns to heed bodily signals is less likely to develop chronic idiopathic constipation.
Fifth, let us not forget the psychological dimension – anxiety surrounding bowel movements can precipitate a vicious cycle of withholding and further impaction.
Sixth, the calculator’s reliance on weight alone ignores the influence of activity level, which can markedly affect gastrointestinal motility.
Seventh, the water quality itself matters; filtered or mineral‑rich water may confer additional benefits over tap water in certain regions.
Eighth, while the calculator offers a static figure, hydration needs fluctuate with temperature, illness, and exertion, demanding a dynamic approach.
Ninth, caregivers should be wary of hidden sugars in flavored drinks that masquerade as hydration but exacerbate constipation.
Tenth, the recommended fluid intake is a ceiling, not a floor; encouraging consistent sipping throughout the day is preferable to a single binge.
Eleventh, the role of probiotics, though not quantified here, may assist in establishing a healthy gut microbiome conducive to regular stools.
Twelfth, one must critique the absence of a symptom tracker – a simple diary could illuminate patterns unseen by mere numbers.
Thirteenth, the tool’s apparent lack of accessibility features, such as screen reader compatibility, marginalizes a segment of the population.
Fourteenth, the therapeutic options – laxatives, stool softeners, behavioral therapy – remain unexplored in this digital vignette.
Fifteenth, a reminder that chronic constipation can occasionally herald underlying organic disease, necessitating medical evaluation.
In summation, while the calculator is a commendable adjunct, it is but a single brushstroke in the grand canvas of pediatric gastrointestinal health.
Faith Leach
Wow, that was a marathon of a comment – impressive stamina. It really drives home how many factors we need to juggle.
Eric Appiah Tano
Exactly, staying hydrated is just one piece of the puzzle, but it’s a crucial one. Let’s keep sharing practical tips.