Chronic diarrhea that won’t go away-no blood, no fever, no obvious cause-is one of the most frustrating health problems people face. For many, it’s not just inconvenient; it’s life-shattering. You’re avoiding social events, dreading long drives, waking up at night to rush to the bathroom. And yet, your colon looks perfectly normal on a colonoscopy. That’s the cruel twist of microscopic colitis.
What Exactly Is Microscopic Colitis?
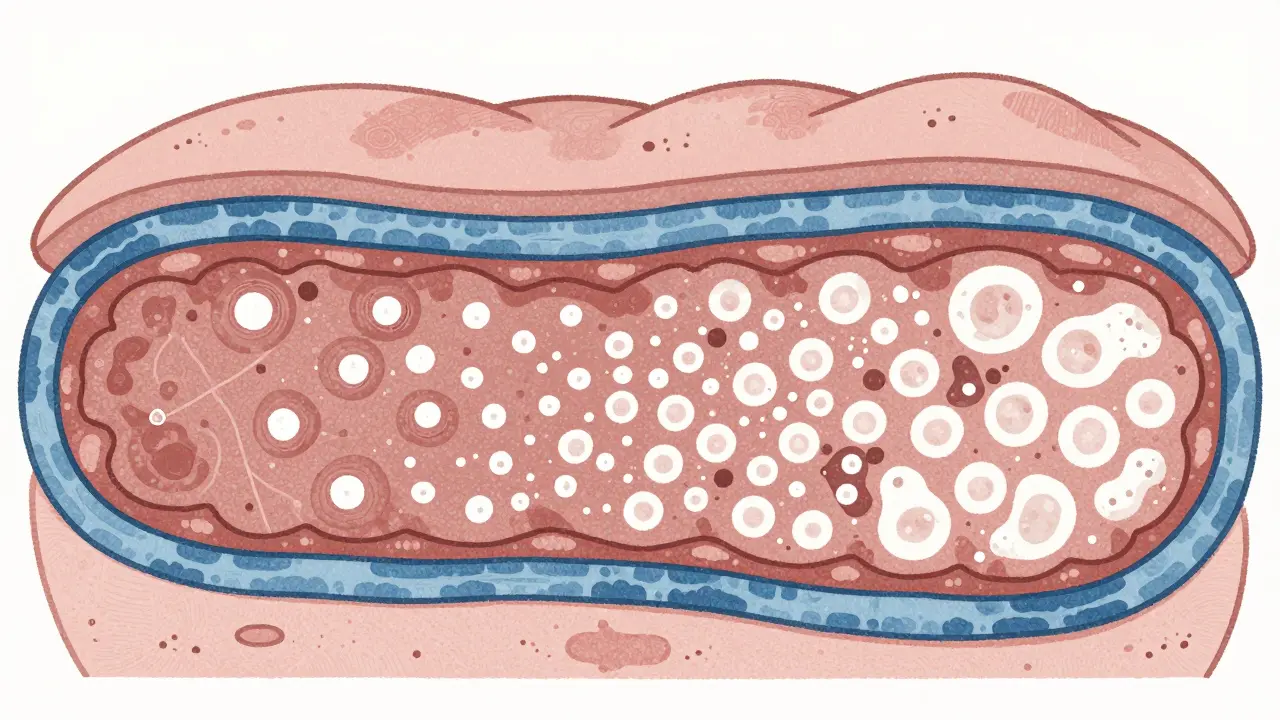
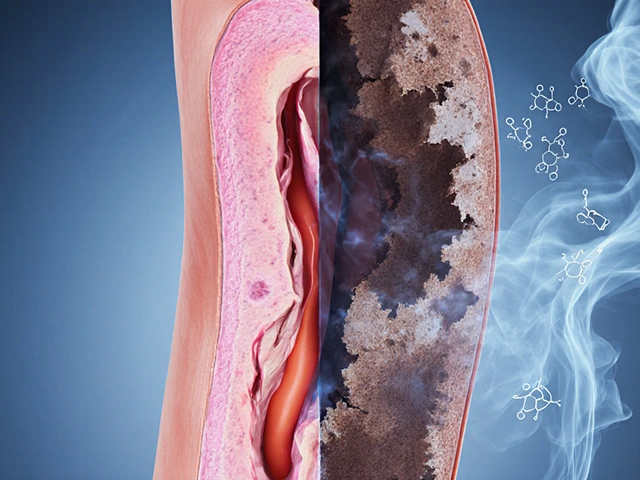
Microscopic colitis isn’t one disease-it’s two. Collagenous colitis and lymphocytic colitis. Both cause the same symptoms: persistent, watery diarrhea, often 5 to 10 times a day. Some people have abdominal cramps, weight loss, or fecal incontinence. Others feel fine except for the constant need to go. The catch? There’s nothing wrong with your colon when your doctor looks inside it. The inflammation is invisible to the naked eye. Only under a microscope, when a biopsy is taken, can you see the problem. In lymphocytic colitis, the lining of the colon is flooded with too many white blood cells-more than 20 per 100 surface cells. In collagenous colitis, there’s a thick band of collagen-like scar tissue-under the surface lining, at least 10 micrometers thick. These changes don’t show up on scans or during a routine colonoscopy. That’s why diagnosis often takes over a year. Many patients are told they have IBS, told to eat less fiber, or given antidiarrheals that barely help. It mostly affects older adults, especially women over 60. About 70% of cases are in women. The reason isn’t clear, but hormones, autoimmune triggers, or reactions to medications like NSAIDs, SSRIs, or proton pump inhibitors might play a role. The number of cases has more than quadrupled since the 1990s, mostly because doctors now know to take biopsies when someone has chronic watery diarrhea-even if they look healthy.Why Budesonide Is the Go-To Treatment
When symptoms are bad enough to disrupt daily life, doctors don’t reach for random remedies. They turn to budesonide. Why? Because it works-and it doesn’t wreck your body like older steroids. Budesonide is a corticosteroid, but it’s designed to act locally in the gut. When you swallow it, 90% of the drug gets broken down by your liver before it ever enters your bloodstream. That means only about 10-15% circulates systemically. Compare that to prednisone, which floods your whole body. With prednisone, you get insomnia, high blood sugar, mood swings, and bone thinning. With budesonide, side effects are mild: maybe a bit of acne, trouble sleeping, or slight mood changes. Serious side effects are rare. Multiple studies show budesonide works. In clinical trials, 75% to 85% of people with microscopic colitis go into remission within 6 to 8 weeks. That’s compared to just 25% to 30% on a placebo. For collagenous colitis, one major trial found 84% of patients had complete symptom relief with budesonide, versus only 38% on placebo. Most people feel better within two weeks. One patient on Reddit wrote, “Went from 10 trips a day to 2 in 10 days. I cried when I slept through the night.” The standard dose is 9 mg once daily for 6 to 8 weeks. That’s it. No long-term use unless you need it. And even then, you don’t stop cold turkey. Doctors taper slowly-drop by 3 mg every two to four weeks-to reduce the chance of symptoms coming back.What Happens After Treatment?
Here’s the hard truth: budesonide doesn’t cure microscopic colitis. It controls it. About half of the people who stop taking it will have symptoms return within a year. For some, it comes back fast. For others, it’s months or even years. That’s why 30% to 40% of patients end up on maintenance therapy-lower doses of budesonide, like 6 mg daily, for several months or even years. It’s not ideal, but it’s better than living with daily diarrhea. The European Microscopic Colitis Group recommends maintenance therapy for people who relapse after stopping. Some doctors use it for up to 12 months, especially in older patients who can’t afford to have flare-ups. But long-term steroid use-even low-dose-raises questions. Are we risking adrenal suppression? Bone loss? Glucose issues? We don’t have perfect data beyond 12 months. Some experts worry we’re treating a chronic condition with a drug not designed for lifelong use. Still, for now, it’s the best tool we have.
Other Options-And Why They Fall Short
There are alternatives, but none match budesonide’s effectiveness. Bismuth subsalicylate (Pepto-Bismol) helps about 26% of people. It’s cheap and safe, but it’s not enough for moderate to severe cases. Mesalamine (the same drug used for ulcerative colitis) works in 40-50% of patients, but the response is inconsistent. Cholestyramine can help if bile acid malabsorption is part of the problem-about 60-70% respond-but not everyone has that. Anti-TNF drugs like infliximab? They’re expensive ($2,500-$3,000 per infusion), risky (infections, cancer concerns), and only help 20-30% of people with microscopic colitis. They’re reserved for the rare cases that don’t respond to anything else. And then there’s cost. Generic budesonide costs $150-$250 for an 8-week course. The branded version, Entocort EC, can run $800-$1,200. Without insurance, that’s a barrier for many. Some patients report having to choose between paying for medication or groceries.What Patients Really Say
Online forums like Reddit and PatientsLikeMe are full of stories. About 68% of users report major improvement on budesonide. “I got my life back,” one wrote. “I traveled for the first time in three years.” But 32% had a rougher experience. Some felt worse-insomnia, anxiety, acne. Others got better, then relapsed. One patient wrote: “Worked great for 6 weeks. Then it stopped. Now I’m on maintenance for two years. I don’t know if I’ll ever get off it.” A few found success combining treatments. One user took budesonide plus cholestyramine and finally got relief after three years of suffering. Another switched from budesonide to a low-FODMAP diet and stayed symptom-free. The message? There’s no one-size-fits-all. But budesonide gives most people their best shot.What You Should Know Before Starting
If your doctor prescribes budesonide, ask about these things:- Do you have a baseline bone density scan? Older adults, especially women, should be checked before starting.
- Are you getting your blood sugar monitored? Even low-dose steroids can raise glucose levels.
- How will you taper? Don’t stop suddenly. Slow reduction lowers relapse risk.
- What if it doesn’t work? Have a backup plan-maybe cholestyramine or a diet change.
What’s Next for Treatment?
Researchers are looking at new options. Vedolizumab, a drug that targets gut-specific immune cells, showed 65% remission in early trials and got Fast Track status from the FDA in 2023. It’s not approved yet, but it’s coming. Other studies are exploring genetic markers-like HLA-DQ2/8-to predict who responds best to budesonide. That could mean personalized treatment in the future. For now, budesonide remains the gold standard. It’s not perfect. It’s not a cure. But for most people with microscopic colitis, it’s the difference between living in constant discomfort and living normally again.Can microscopic colitis be cured?
There’s no known cure for microscopic colitis. But most people achieve long-term symptom control with treatment. About half of patients go into remission after a short course of budesonide and never have symptoms return. Others need maintenance therapy or lifestyle changes to stay well. Symptoms often improve over time, even without treatment, but it can take years.
How long does it take for budesonide to work?
Most people notice improvement within 1 to 2 weeks. By week 4, 70-80% of patients have significant symptom reduction. Full remission-no diarrhea, no cramps-usually happens by week 6 to 8. Don’t expect instant results, but don’t wait too long to judge effectiveness either.
Is budesonide safe for long-term use?
Budesonide is much safer than older steroids like prednisone, thanks to its targeted action. But long-term use (beyond 12 months) isn’t well studied. Doctors monitor for bone density loss, blood sugar changes, and adrenal function, especially in older patients. For most, the benefits outweigh the risks when used under supervision.
Can diet help with microscopic colitis?
Yes, diet can help manage symptoms, but it won’t treat the inflammation. Many people benefit from a low-FODMAP diet, avoiding caffeine, dairy, and artificial sweeteners. If bile acid malabsorption is involved, a low-fat diet and cholestyramine can help. Diet is a support tool-not a replacement-for medication like budesonide.
Why do I need a colonoscopy with biopsies if I already have diarrhea?
Because many conditions cause chronic diarrhea-IBS, celiac disease, infections, bile acid issues. Only a biopsy can confirm microscopic colitis. Even if your colon looks normal during the scope, the inflammation is hidden. Without biopsies, you might be misdiagnosed and treated incorrectly. Biopsies are taken from multiple areas of the colon to catch the patchy changes.
What’s the difference between collagenous and lymphocytic colitis?
They’re diagnosed by different microscopic changes. Collagenous colitis has a thick collagen band under the colon lining (≥10 micrometers). Lymphocytic colitis has too many white blood cells inside the lining. Symptoms are nearly identical, but collagenous colitis is more likely to cause weight loss and is slightly more common in older women. Treatment is the same for both.
Can I take budesonide if I have liver disease?
Not if you have severe liver disease (Child-Pugh Class C). Budesonide is processed by the liver. If your liver can’t break it down, the drug builds up in your blood, increasing side effect risks. Mild to moderate liver disease may be okay with lower doses and close monitoring. Always tell your doctor about any liver conditions.





15 comments
Dusty Weeks
budesonide saved my life. went from 12x a day to 1x. slept through the night for the first time in 4 years 😭
Donna Peplinskie
I’m so glad you shared this. My mom was misdiagnosed with IBS for 3 years before they did the biopsy. She’s been on 3mg maintenance for 18 months now and finally feels like herself again. It’s not perfect, but it’s peace.
jaspreet sandhu
people always blame meds but nobody talks about how the modern diet is full of fake sugars and processed junk that wreck your gut. budesonide just masks the problem. you need to go back to real food like our grandparents did. no more gluten no more soy no more sugar. simple. done.
Ann Romine
I’ve been on budesonide for 6 months now. The insomnia is real. But honestly? I’d rather lose sleep than lose my social life. I went to my niece’s wedding last month. I didn’t hide in the bathroom the whole time. That’s worth it.
Austin Mac-Anabraba
Let’s be honest. This is just another example of Big Pharma pushing a steroid under a fancy name. Budesonide isn’t magic. It’s just prednisone with a better marketing team. And now we’re normalizing long-term steroid use in older women like it’s vitamin D. We’re not curing anything. We’re just managing a system failure.
LIZETH DE PACHECO
To anyone reading this and scared: you’re not alone. I was terrified to start budesonide too. But I talked to my doctor, got my bone scan, and took it slow. It worked. And if it doesn’t? There are other options. You’ve got this.
Layla Anna
my sister tried cholestyramine after budesonide failed. it worked for her. weirdly. she says it tastes like chalk and makes her feel like a science experiment but no more accidents. i think she’d take chalk every day if it meant she could travel again. 🤍
sharad vyas
in india, many still think this is just stress. no one believes you until you collapse. i waited 5 years. my doctor laughed when i asked for biopsy. now i take budesonide. quiet. no drama. just peace.
Olukayode Oguntulu
the real tragedy isn't the disease-it's the epistemological vacuum in gastroenterology. We treat symptoms with pharmacological band-aids while ignoring the ontological rupture between biopolitics and embodied suffering. Budesonide is a neoliberal palliative. We need systemic re-ontologization of gut health, not molecular bandages.
Paul Ong
i was on budesonide for 8 weeks and felt like a new person. then i stopped cold because i was scared of side effects. boom. back to 8 trips a day. learned my lesson. now i taper slow. life is better. don’t be dumb like me
Alex Warden
why are we letting foreigners dictate our medicine? budesonide is made in Germany. we have turmeric. we have ginger. we have ayurveda. why are we swallowing pills from Europe when our grandmas knew how to fix this with tea and fasting?
Kristen Russell
this post helped me so much. i finally feel seen. thank you.
Phoebe McKenzie
if you’re still on budesonide after a year, you’re not healing-you’re addicted. stop blaming the disease and start taking responsibility. your gut isn’t broken, your lifestyle is. go vegan. go keto. go raw. stop taking steroids like they’re candy.
Heather Josey
I appreciate the thorough breakdown. For those considering maintenance therapy, please know it’s not a failure. It’s strategy. Many of us are managing chronic conditions, not chasing cures. And that’s okay. Your worth isn’t tied to being drug-free.
Lee M
the fact that we need a steroid to fix a problem caused by other drugs (PPIs, SSRIs) is the real indictment. we’re treating side effects of side effects. the system is broken. we’re just rearranging deck chairs on the Titanic.