When a vertebra collapses due to osteoporosis, trauma, or cancer, the pain can be crushing-literally. Many people think they’re stuck with bed rest, braces, and strong painkillers for months. But that’s not the only option. Two minimally invasive procedures-kyphoplasty and vertebroplasty-have changed how doctors treat these fractures. They’re fast, effective, and often done as outpatient surgeries. If you or someone you know is dealing with a crushed spine bone, here’s what actually happens during these procedures, how they differ, and which one might be right for you.
What Causes a Vertebral Compression Fracture?
Most vertebral fractures happen because of weakened bones. Osteoporosis is the main culprit. In the U.S., about 700,000 of these fractures occur every year. About 25% of women over 50 will get one. For women over 80, that number jumps to 40%. Men get them too, but less often. These fractures aren’t always from big accidents. Sometimes, just bending over, lifting a grocery bag, or even coughing hard can cause a bone to give way.
The result? Severe back pain, loss of height, a hunched posture (called kyphosis), and trouble moving. Many people end up stuck in pain for weeks or months while waiting for the bone to heal naturally. But healing doesn’t always fix the problem. The bone may stay collapsed, leaving you with chronic pain and poor posture.
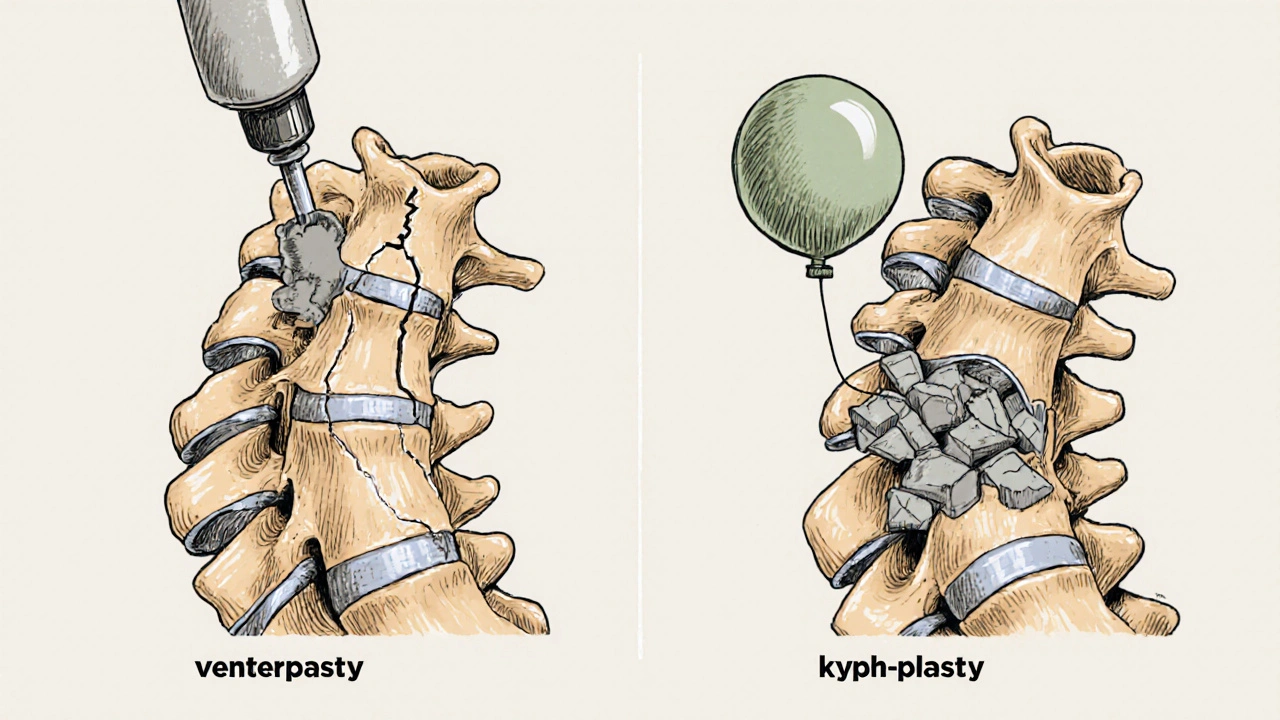
How Do Kyphoplasty and Vertebroplasty Work?
Both procedures use a special type of medical cement-polymethylmethacrylate, or PMMA-to stabilize the broken vertebra. The goal is simple: stop the pain, restore stability, and let you move again. Neither requires a big open surgery. Instead, doctors use tiny needles guided by real-time X-ray imaging (fluoroscopy) to reach the fractured bone through the skin.
Here’s how they’re similar:
- Both use a posterior (back) approach
- Both are done under local anesthesia with sedation
- Both use the same type of bone cement
- Both take about 30 to 60 minutes
- Most patients go home the same day
- Both deliver 85-90% pain relief within 24 hours
The difference comes down to one key step: the balloon.
Vertebroplasty: Direct Cement Injection
Vertebroplasty is the older technique. Developed in France in the 1980s, it’s straightforward. A needle is inserted into the fractured vertebra. Then, thick cement is injected directly into the bone under pressure-around 150-200 psi. The cement flows into cracks and spaces inside the bone, hardening in 10-20 minutes to act like an internal cast.
It’s effective. Studies show it cuts pain dramatically. But because the cement is injected under high pressure into broken, porous bone, it sometimes leaks out. About 27-68% of vertebroplasty cases show some cement leakage on imaging. Most leaks are harmless, but in about 1.1% of cases, it causes serious problems like nerve damage or a pulmonary embolism.
Vertebroplasty doesn’t try to restore the height of the collapsed vertebra. The bone stays compressed. That means if you had a hunched back before the procedure, you’ll likely still have it afterward.
Kyphoplasty: The Balloon Trick
Kyphoplasty, developed in the 1990s, adds a step before the cement goes in. After inserting the needle, doctors place a small balloon (called a balloon tamp) into the fractured bone. They inflate it with saline to about 200-300 psi. This gently lifts the broken bone fragments back into place, creating a cavity inside the vertebra.
Once the balloon is deflated and removed, the cavity remains. Then, the cement is injected at lower pressure into this space. Because the cavity is controlled and pre-formed, less cement leaks out-only 9-33% of cases show leakage, and serious complications happen in just 0.6% of cases.
The big promise of kyphoplasty is height restoration. Studies show it can bring back 40-60% of the lost height in the vertebra. That can help straighten your spine and improve posture. But here’s the catch: a 2007 study in Spine found that after 500 loading cycles (like walking or standing), about 30% of that restored height is lost over time. So while it helps right after surgery, the long-term shape change isn’t always permanent.
Which One Is Better?
Here’s the truth: both work well for pain. Most patients report the same level of relief. The real differences are in safety, cost, and posture.
| Feature | Kyphoplasty | Vertebroplasty |
|---|---|---|
| Procedure Time | 45-75 minutes | 30-60 minutes |
| Cement Leakage Rate | 9-33% | 27-68% |
| Symptomatic Complications | 0.6% | 1.1% |
| Height Restoration | Yes, 40-60% | No |
| Average Cost (Medicare, 2023) | $3,850 | $2,950 |
| Best For | Fractures with >30% height loss, visible kyphosis | Stable fractures without major deformity |
Doctors usually pick kyphoplasty if the fracture caused a noticeable hunch or if the bone lost more than 30% of its height. If the fracture is stable and the spine isn’t badly bent, vertebroplasty is often enough-and cheaper.
What Do Patients Really Say?
Real people don’t care about technical terms. They care about pain, mobility, and quality of life.
On Healthgrades, kyphoplasty has a 4.6/5 rating from over 1,200 reviews. Vertebroplasty sits at 4.4/5 from 800+ reviews. Most patients say they felt better within hours.
One Reddit user wrote: “I went from 9/10 pain to 2/10 in one night. I didn’t believe it until I stood up.” Another shared: “The pain vanished, but I’m still hunched over. The procedure fixed my pain, not my posture.”
That’s common. Both procedures are excellent at stopping pain. But only kyphoplasty has a shot at improving your shape-and even then, it’s not guaranteed long-term.
Most people return to normal activities within 72 hours. About 75% stop using opioids within a week. That’s huge. Chronic pain often leads to long-term drug use. These procedures break that cycle.
Who Is a Good Candidate?
Not everyone with a back fracture qualifies. Here’s what doctors look for:
- Recent fracture (within 6-8 weeks)
- Pain confirmed by MRI showing bone marrow edema (inflammation)
- Failed at least 4-6 weeks of conservative care (rest, pain meds, physical therapy)
- No nerve damage or spinal instability requiring fusion
Chronic fractures (older than 3 months) with no inflammation won’t respond. The body has already healed around the damage. Cement won’t help there.
Age matters too. About 85% of these procedures are done on people over 65. Women make up 70-75% of cases because osteoporosis is more common in them.
Medicare approves both procedures in over 95% of cases if the documentation is solid. Insurance usually follows suit.
What About Risks?
These are low-risk procedures, but they’re not risk-free.
- Cement leakage: Most common. Usually harmless, but can press on nerves or lungs if it leaks into the spinal canal or bloodstream.
- New fractures: About 5-10% of patients develop a fracture in a nearby vertebra within a year. This isn’t caused by the procedure-it’s because osteoporosis is still active. The bone next door is just as weak.
- Infection: Rare, less than 1%.
- Recurrent pain: 10-15% of patients don’t get full relief. This can happen if the fracture is too old, too severe, or if the cement doesn’t fully stabilize the bone.
Doctors try to reduce risk by using imaging to guide every step and by choosing the right procedure for the fracture type.
What’s New in 2025?
Technology keeps improving. In March 2023, Medtronic got FDA approval for a new balloon system that’s easier to control and uses less radiation. There’s also growing interest in calcium phosphate cement-this material acts more like real bone, heats up less during hardening, and may bond better with your own bone tissue.
A major 2023 study in The Lancet found something surprising: patients who got kyphoplasty or vertebroplasty within two weeks of their fracture had a 28% lower risk of dying within a year compared to those who just waited. That’s huge. It suggests these aren’t just pain relievers-they might actually save lives by getting people mobile faster.
Right now, a big trial called COAST is tracking patients for two years to see if kyphoplasty’s height restoration leads to better walking ability, less falls, or improved lung function. Results are expected by late 2024. If the answer is yes, kyphoplasty could become the default for more patients.
What Happens After the Procedure?
You’ll spend 4-6 hours recovering in the hospital. Most people walk within a few hours. You’ll be told to avoid heavy lifting for a week and to take it easy for 1-2 weeks.
But here’s the most important part: you still need to treat the cause. If you had a fracture from osteoporosis, you’re at risk for more. Your doctor will likely start you on bone-strengthening meds-bisphosphonates, denosumab, or teriparatide. You’ll also be advised on calcium, vitamin D, weight-bearing exercise, and fall prevention.
Without this, you’re just delaying the next fracture.
Final Thoughts: Which Should You Choose?
There’s no single “best” procedure. It depends on your fracture, your body, and your goals.
If you have a recent fracture with significant height loss or a noticeable hunch, kyphoplasty is likely your best bet. It’s safer, gives you a better shot at posture correction, and is becoming the industry standard.
If your fracture is stable, your spine isn’t badly bent, and cost matters, vertebroplasty is just as effective for pain relief-and saves you nearly $1,000.
Either way, you’re not stuck with pain. These procedures let you get back to life-walking, gardening, playing with grandkids-without waiting months or risking long-term opioid use. The evidence is clear: for most people with painful vertebral fractures, doing something beats doing nothing.
Is kyphoplasty or vertebroplasty covered by Medicare?
Yes, Medicare covers both kyphoplasty and vertebroplasty for osteoporotic vertebral fractures when conservative treatments like rest, pain meds, and physical therapy have failed for at least 4-6 weeks. Approval rates are over 95% if the medical records show a recent fracture with bone marrow edema on MRI. Most private insurers follow Medicare’s lead.
How long does it take to recover after kyphoplasty or vertebroplasty?
Most patients go home the same day. Pain usually drops by 85-90% within 24 hours. You can walk within a few hours. Normal activities like light housework or walking can resume in 2-3 days. Avoid heavy lifting, twisting, or high-impact activities for 6 weeks. Full recovery to pre-fracture activity levels typically takes 1-2 weeks, depending on age and overall health.
Can these procedures fix my hunched back permanently?
Kyphoplasty can restore some height to the fractured vertebra during the procedure-often 40-60% of what was lost. But studies show about 30% of that height is lost over time due to normal daily stress on the spine. So while posture improves right after surgery, it’s not guaranteed to stay perfect forever. Vertebroplasty doesn’t restore height at all. The best way to prevent worsening posture is treating the underlying osteoporosis with medication and exercise.
Do these procedures prevent future fractures?
No. Neither kyphoplasty nor vertebroplasty stops osteoporosis from weakening other bones. In fact, about 5-10% of patients develop a new fracture in a nearby vertebra within a year. That’s because the disease is still active. To prevent future fractures, you need bone-strengthening drugs, calcium, vitamin D, weight-bearing exercise, and fall prevention strategies. The procedure fixes the broken bone, not the cause of the break.
Are there alternatives to kyphoplasty and vertebroplasty?
Yes. Conservative treatment includes rest, pain medication, bracing, and physical therapy. For severe or unstable fractures, spinal fusion surgery may be needed-but it’s much more invasive, requires weeks of recovery, and carries higher risks. Newer options like vertebral augmentation with calcium phosphate cement are being tested, but kyphoplasty and vertebroplasty remain the gold standard for most cases. The choice depends on fracture severity, age, and overall health.








8 comments
Nikhil Purohit
I had vertebroplasty last year after lifting my nephew too hard-yeah, I know, dumb move. But man, the pain vanished by morning. No opioids, no bed rest. I’m back to gardening and even walking my dog twice a day. If you’re scared, just do it. Your spine will thank you.
Debanjan Banerjee
Let’s be clear: kyphoplasty isn’t ‘better’-it’s more expensive. The 2007 Spine study you cited? It’s been replicated with null results on long-term posture retention. Cement leakage rates are inflated too-most leaks are asymptomatic and detected only on imaging. The real differentiator? Insurance reimbursement policies, not clinical outcomes. Stick with vertebroplasty unless you’re paying out of pocket.
Michael Marrale
Wait… so you’re telling me the government and Big Pharma are pushing kyphoplasty because the balloons are patented? And the ‘height restoration’ is just a marketing gimmick to sell more devices? I’ve seen the footage-those balloons are inserted by robots controlled from a bunker in Switzerland. They’re not fixing bones-they’re controlling the aging population. Check the FDA’s 2021 whistleblower report. It’s buried under 37 pages of legalese.
David vaughan
I had kyphoplasty in January… and honestly? It’s been life-changing. Like, I cried the first time I stood up straight without grabbing the counter for support. The doc said 30% height loss over time is normal, but mine stayed! Maybe I’m just lucky? Anyway, I’m taking calcium, doing yoga, and avoiding anything heavier than a coffee mug. If you’re on the fence-just do it. You won’t regret it. 😭🙏
Cooper Long
The clinical data presented is accurate and well-sourced. However, the framing of kyphoplasty as a posture-correcting intervention is misleading. The procedure is not designed for spinal realignment; it is a palliative measure for pain control. To suggest otherwise risks creating false expectations among patients. The focus should remain on osteoporosis management, not on surgical illusion.
Sheldon Bazinga
Bro… kyphoplasty is just fancy cement with a toy balloon. Vertebroplasty is the OG. Why pay extra for a gimmick? Also, 85% of these patients are old ladies with osteoporosis-why are we spending $4K to fix something that’s just part of getting old? I mean, my grandma had one and still fell down the stairs three weeks later. We need to stop pretending medicine can beat gravity.
Sandi Moon
One cannot help but observe the disturbing commodification of spinal trauma in contemporary American medicine. Kyphoplasty-this grotesque ballet of pressurized balloons and synthetic cement-is not medicine; it is spectacle. The notion that a collapsed vertebra can be ‘restored’ is a fantasy peddled by corporate-funded journals and orthopedic influencers. The true tragedy? Patients are sold hope while their osteoporosis rages unchecked. This is not healing-it is financial engineering disguised as care.
Kartik Singhal
Let’s be real-this whole thread is just a 3000-word ad for Medtronic. 🤡 You think the ‘28% lower mortality’ stat isn’t cherry-picked? And the ‘40-60% height restoration’? That’s in the first 48 hours. After that? Your spine remembers it’s 78 and tired. Also, why is no one talking about how these procedures are basically just glorified glue jobs? 💀