Opioid-Antidepressant Interaction Checker
Check if your opioid pain medication is safe to use with your antidepressant. Select your medications below to see if they're a dangerous combination.
It’s not just about pain relief. When you’re taking an opioid for chronic pain or after surgery, you might not realize you’re also risking a dangerous, even deadly, reaction if you’re on certain antidepressants, cough medicines, or other drugs. Serotonin syndrome isn’t rare. It’s underdiagnosed, often mistaken for infections or anxiety attacks - but it can kill you in hours.
What Exactly Is Serotonin Syndrome?
Serotonin syndrome happens when too much serotonin builds up in your brain and nervous system. It’s not an allergy. It’s a pharmacological overload. Your body can’t handle the flood of serotonin signals, and your nerves go haywire. You might start sweating, shaking, or feeling confused. Then your muscles lock up. Your temperature spikes. Your heart races. In severe cases, you can slip into a coma or die. This isn’t just a theory. Between 2015 and 2021, New Zealand’s drug safety agency recorded 41 confirmed cases linked to opioids. The most common culprit? Tramadol. In fact, nearly 60% of those cases involved tramadol combined with an antidepressant. And it doesn’t take much - a single 50mg dose of tramadol on top of venlafaxine was enough to send a 42-year-old woman to the ICU with a fever of 40.1°C and rigid muscles.Not All Opioids Are Created Equal
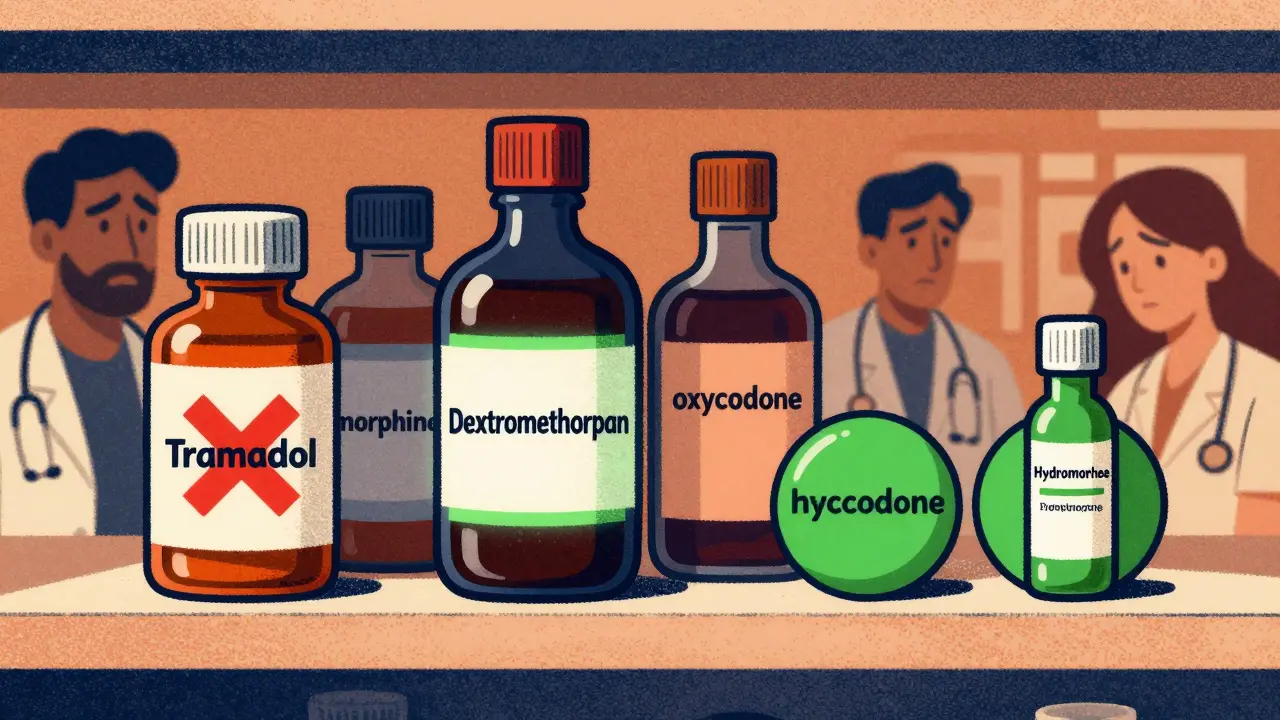
You can’t treat all opioids the same. Some are basically silent when it comes to serotonin. Others are ticking time bombs. High-risk opioids - these are the ones you should avoid if you’re on any antidepressant:- Tramadol: It doesn’t just relieve pain - it blocks serotonin reuptake, just like SSRIs do. That’s why it’s responsible for nearly 80% of all reported opioid-antidepressant interactions.
- Meperidine (pethidine): Used mostly in hospitals, but still found in some pain clinics. It’s a major offender.
- Dextromethorphan: This isn’t a prescription opioid - it’s in cough syrups, cold pills, and sleep aids. A daily 30mg dose (half a typical cough syrup dose) has caused fatal serotonin syndrome in people on SSRIs.
These three are so dangerous together with antidepressants that health agencies in New Zealand, Europe, and the U.S. now say they’re contraindicated - meaning they shouldn’t be used together at all.
Medium-risk opioids - use with extreme caution:
- Methadone: Even though it blocks serotonin reuptake in the lab, real-world data shows its risk is lower than expected - probably because it’s metabolized slowly. Still, it’s not safe with fluvoxamine or other strong CYP inhibitors.
- Fentanyl: Usually considered safe, but high doses (like during surgery) can activate serotonin receptors directly. That’s why anesthesiologists now warn against it in patients on serotonergic drugs.
Low-risk opioids - these are your best options if you need pain relief and are on antidepressants:
- Morphine: No serotonin activity. No reuptake inhibition. Safe.
- Oxycodone: Minimal effect on serotonin. No SERT inhibition in studies.
- Hydromorphone: Same as morphine. Clean profile.
- Codeine: Usually safe - unless you’re a fast metabolizer or taking it with triptans or other serotonergic drugs.
Dr. Kenneth McCarberg put it plainly: “Morphine, oxycodone, and hydrocodone have minimal serotonergic activity. Don’t avoid them just because of fear.”
Why Do Some Opioids Trigger This?
It’s not just one mechanism. Different opioids mess with serotonin in different ways:- SERT inhibition: Tramadol, meperidine, and dextromethorphan block the serotonin transporter. That’s like turning off the vacuum that normally clears serotonin from your brain. Result? Too much serotonin hanging around.
- Receptor activation: Fentanyl and methadone bind directly to 5-HT2A receptors - the same ones targeted by hallucinogens. This can trigger serotonin syndrome even without increasing serotonin levels.
- Metabolism interference: SSRIs like fluoxetine and paroxetine block the CYP2D6 enzyme. That means tramadol can’t turn into its active painkiller form. Instead, it builds up as the parent drug - which is even more potent at blocking serotonin reuptake.
And here’s the scary part: some people have genetic variations in their serotonin transporter gene (SLC6A4). If you’re one of them, even a small dose of tramadol could push you over the edge.
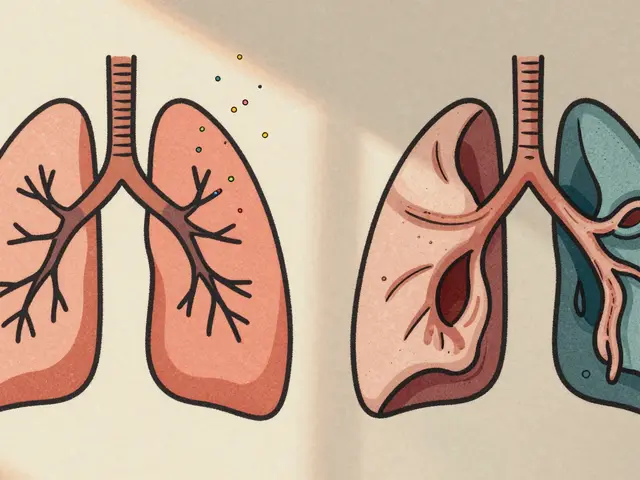
What Does Serotonin Syndrome Look Like?
It’s not always obvious. Symptoms come on fast - usually within hours of adding a new drug. The classic signs are the “triad”:- Mental status changes: Agitation, confusion, hallucinations, restlessness, or coma.
- Autonomic hyperactivity: Sweating, fever (over 38°C), fast heart rate, high blood pressure, dilated pupils, diarrhea.
- Neuromuscular abnormalities: Muscle rigidity, tremors, twitching, overactive reflexes, shivering.
One case from 2021 involved a woman who started tramadol for back pain. Two days later, she couldn’t walk. Her muscles were locked. She was confused and sweating through her sheets. Her temperature hit 40.1°C. She needed intensive care. She survived - but only because her doctor recognized it fast.
Many doctors miss it. They think it’s a flu, a panic attack, or even a seizure. But if you’re on an antidepressant and start feeling off after starting a new painkiller - especially tramadol, dextromethorphan, or meperidine - don’t wait. Get help.
What Should You Do If You’re on Antidepressants?
If you’re taking an SSRI, SNRI, TCA, or MAOI - and you need pain relief - here’s what to do:- Check your current meds. Look at every pill you take - including cough syrup, sleep aids, and migraine meds. Dextromethorphan is hiding in plain sight.
- Ask your doctor: “Is this pain medication safe with my antidepressant?” Don’t assume it is.
- Choose morphine, oxycodone, or hydromorphone. They’re effective, and they don’t mess with serotonin.
- Avoid tramadol, meperidine, and dextromethorphan at all costs. Even if your doctor says “it’s fine,” push back. The data is clear.
- Know the warning signs. If you feel confused, sweaty, or your muscles start twitching - go to the ER. Don’t wait.
And if you’re on methadone for opioid use disorder? Talk to your provider. Fluvoxamine, fluoxetine, and some antibiotics can spike methadone levels - and serotonin risk - at the same time.
The Bigger Picture
This isn’t just about individual prescriptions. It’s about how we manage pain in a world full of overlapping medications.Since 2020, tramadol use in the U.S. has dropped 18% - not because it’s less effective, but because doctors are finally learning its risks. That’s good news. It means serotonin syndrome cases tied to opioids could fall by 15% over the next five years.
But dextromethorphan? That’s still a problem. Over 28 million OTC doses are sold every year in the U.S. Most people have no idea it’s a serotonin booster. And when someone takes it with their Zoloft or Prozac - they’re playing Russian roulette with their brain chemistry.
The FDA added a black box warning to tramadol-SSRI combos in January 2023. The European Medicines Agency did the same in 2022. That’s not a small step. It’s a red flag.
What If You’ve Already Taken Them Together?
If you’ve accidentally combined a high-risk opioid with an antidepressant and feel fine - you’re probably okay. But monitor yourself closely for 48 hours.If you notice any symptoms - even mild ones like restlessness or sweating - stop the opioid immediately and call your doctor. Don’t wait for a fever or rigidity. Early intervention saves lives.
There’s a specific antidote: cyproheptadine. It blocks serotonin receptors. But it’s not magic. It works best when given early. In severe cases, you’ll need ICU care - sedation, cooling, and breathing support.
The bottom line: you don’t need to live in fear. But you do need to be informed.
Pain is real. Depression is real. But combining the wrong drugs can turn treatment into a crisis. Talk to your doctor. Read the labels. Know what’s in your medicine cabinet. And never assume a drug is safe just because it’s prescribed or sold over the counter.
Can you get serotonin syndrome from just one drug?
Yes, but it’s rare. Most cases happen when two or more serotonergic drugs are combined. However, very high doses of tramadol, dextromethorphan, or meperidine alone - especially in overdose - can trigger serotonin syndrome on their own. The risk is much higher when mixed with antidepressants.
Is codeine safe with SSRIs?
Generally, yes - codeine has very low serotonin activity. But there are exceptions. If you’re a fast metabolizer of codeine (due to genetics), your body turns more of it into morphine, which can still trigger issues. Also, if you’re taking codeine with triptans (for migraines) or other serotonergic drugs, the risk goes up. It’s not zero, but it’s far lower than tramadol or dextromethorphan.
What over-the-counter medicines contain dextromethorphan?
Many common cold and cough products include dextromethorphan, including Robitussin, Delsym, NyQuil, Theraflu, and store-brand equivalents. Always check the “active ingredients” list. Even small doses - like 30mg daily - can be dangerous if you’re on an SSRI or SNRI.
How long does it take for serotonin syndrome to develop?
Usually within 2 to 48 hours after starting or increasing a serotonergic drug. Symptoms can appear as quickly as 30 minutes after taking a high dose of dextromethorphan or tramadol, especially if you’re already on an antidepressant. Don’t wait for symptoms to get worse - act fast.
Can you die from serotonin syndrome?
Yes. Between 2015 and 2021, at least three people died from serotonin syndrome caused by dextromethorphan combined with SSRIs. Death usually results from extreme hyperthermia (body temperature over 41°C), muscle breakdown, kidney failure, or cardiac arrest. Early recognition and treatment are critical.
Should I stop my antidepressant if I need an opioid?
No - never stop an antidepressant without medical supervision. Abruptly stopping SSRIs can cause withdrawal symptoms or make depression worse. Instead, switch to a safer opioid like morphine, oxycodone, or hydromorphone. Your doctor can help you adjust safely without risking your mental health.





15 comments
Herman Rousseau
Man, I had no idea dextromethorphan was this dangerous with SSRIs. I’ve been taking NyQuil every time I get a cold for years. 😳 Just checked my cabinet - yep, three bottles. Gonna toss ‘em and switch to saline rinses and rest. Thanks for the wake-up call.
Gabriella da Silva Mendes
Wow, so now we’re supposed to trust Big Pharma’s ‘safe’ opioids but avoid the OTC stuff that’s been around since the 90s? 🤡 I’ve been on Lexapro for 12 years and took tramadol after my knee surgery - I’m still here, ain’t I? They’re just trying to scare people so they can sell more expensive meds. Also, morphine? That’s what they gave my grandpa in the 70s. He died of cancer, not serotonin syndrome. 😴
Johnnie R. Bailey
This is one of the clearest, most medically accurate posts I’ve seen on Reddit in years. The breakdown of SERT inhibition vs. receptor activation is spot-on. Most people don’t realize that fentanyl’s risk isn’t from serotonin reuptake - it’s from direct 5-HT2A binding, which is why it’s sneaky. Even anesthesiologists miss that. And the genetic angle with SLC6A4? Brilliant. If you’re a fast metabolizer of tramadol and on an SSRI, you’re essentially turning a 50mg dose into a 150mg serotonin bomb. This isn’t fearmongering - it’s pharmacokinetics.
Also, props for calling out dextromethorphan. It’s everywhere. My pharmacy tech niece says half her customers don’t even know it’s an opioid analog. We need public health campaigns, not just doctor warnings.
Kathryn Weymouth
I appreciate the thoroughness of this post. However, there’s a small typo in the section about codeine: ‘hydromorphone’ is misspelled as ‘hydrocodone’ in the final sentence of the low-risk list. Also, the FDA’s black box warning was issued in January 2023 for tramadol-SSRI combinations - not for dextromethorphan. Just wanted to clarify for accuracy. This information is vital, and precision matters when lives are at stake.
Vikrant Sura
So you’re saying if I take Robitussin with my Zoloft, I could die? Cool. And I thought my boss giving me a hard time was the biggest threat to my health. 😏
Art Van Gelder
I used to work in ER. Saw a guy come in with rigidity, fever, and hallucinations. Thought it was a bad LSD trip. Turned out he was on fluoxetine and took four cough drops with dextromethorphan because he had a cold. He was 19. We had to intubate him. He woke up three days later asking why his legs felt like concrete. That’s not a myth. That’s Tuesday in the ER.
And yeah, doctors still don’t ask about OTC meds. They ask about ‘drugs’ like cocaine or heroin - but not NyQuil. It’s insane.
Ajay Brahmandam
Hey, I’m on sertraline and took tramadol for a back flare-up last year. Felt a little weird for a day - sweaty, jittery - but thought it was just stress. Now I know. I’ll switch to oxycodone next time. Thanks for the heads-up. This is the kind of info that actually saves lives. 🙏
jenny guachamboza
Wait so you’re saying the government is hiding the truth about opioids?? Like, they let tramadol on the market because they want us to get addicted?? And dextromethorphan? That’s just Big Pharma’s sneaky way to get us hooked on cough syrup!! 😱 I read on a forum that the CDC is secretly tracking serotonin syndrome deaths to justify banning all OTC meds!! I’m not taking anything anymore!!
Aliyu Sani
Bro, this is deep. SERT inhibition? 5-HT2A binding? CYP2D6 polymorphisms? You’re speaking my language. In Nigeria, we call tramadol ‘somo’ - everyone uses it. No one knows it’s a serotonin trap. I’ve seen guys on fluoxetine pop tramadol like candy for energy. They call it ‘killing two birds.’ But when they start twitching and sweating like they’re possessed? We just think it’s ‘spiritual attack.’ This post? It’s a public service. We need this translated into pidgin.
Tony Du bled
I used to be a pharmacist. I’ve seen this play out too many times. A patient on venlafaxine picks up tramadol because their doctor said ‘it’s not a real opioid.’ They don’t even know what ‘real opioid’ means. I’ve had to pull scripts, call doctors, explain serotonin syndrome to grandmas who thought cough syrup was harmless. The system is broken. Patients are left to Google it - and half the time, they find TikTok videos saying ‘it’s fine.’
Knowledge is power. But access? That’s the real issue.
Jeremy Hendriks
It’s not about the drugs - it’s about the illusion of control. We think we’re managing our pain and our mood, but we’re just juggling chemical grenades. The real tragedy? We’re taught to trust prescriptions like they’re divine decrees. But the body doesn’t care about your doctor’s signature. It cares about receptors, transporters, enzymes. You’re not ‘taking medicine.’ You’re conducting a biochemical experiment on yourself. And most of us are amateurs with a flamethrower.
Candy Cotton
While I appreciate the intent behind this communication, I must emphasize that the casual tone and colloquial phrasing employed herein are wholly inappropriate for a medical advisory of such gravity. The use of emoticons, contractions, and informal syntax undermines the seriousness of serotonin syndrome. A formal, peer-reviewed dissemination of this information - preferably through the AMA or CDC - would be more befitting of the stakes involved. Sincerely, Dr. Candy Cotton, MD, MPH.
Kiranjit Kaur
This is exactly why we need better patient education. I’m a nurse in Delhi, and I’ve seen so many patients on SSRIs take over-the-counter cold meds without a second thought. They trust the packaging. They don’t read the tiny print. We need pamphlets in local languages, posters in pharmacies, maybe even radio ads. This info shouldn’t be hidden in a Reddit thread. It should be on every medicine bottle. ❤️
Jim Brown
There is a profound philosophical dimension to this issue. We have constructed a medical paradigm in which the body is reduced to a chemical ledger - balance this receptor, inhibit that transporter - and yet we remain profoundly disconnected from the lived experience of the patient. The fear of serotonin syndrome is not merely pharmacological; it is existential. We are told to trust science, yet we are given no language to speak of our own bodily sensations. The irony? The very drugs meant to restore equilibrium - antidepressants, analgesics - become agents of chaos when their mechanisms are misunderstood. Perhaps the real crisis is not in our pharmacology, but in our epistemology: we know how drugs work, but we have forgotten how to listen to our bodies.
Sai Keerthan Reddy Proddatoori
India banned tramadol in 2018. Why? Because Americans brought it here and sold it like candy. Now you’re telling us it’s dangerous? We knew. We saw the bodies. But you in America keep selling it. You don’t care. You only care when it affects you. This isn’t science - it’s hypocrisy.