What Are Medicaid Substitution Rules?
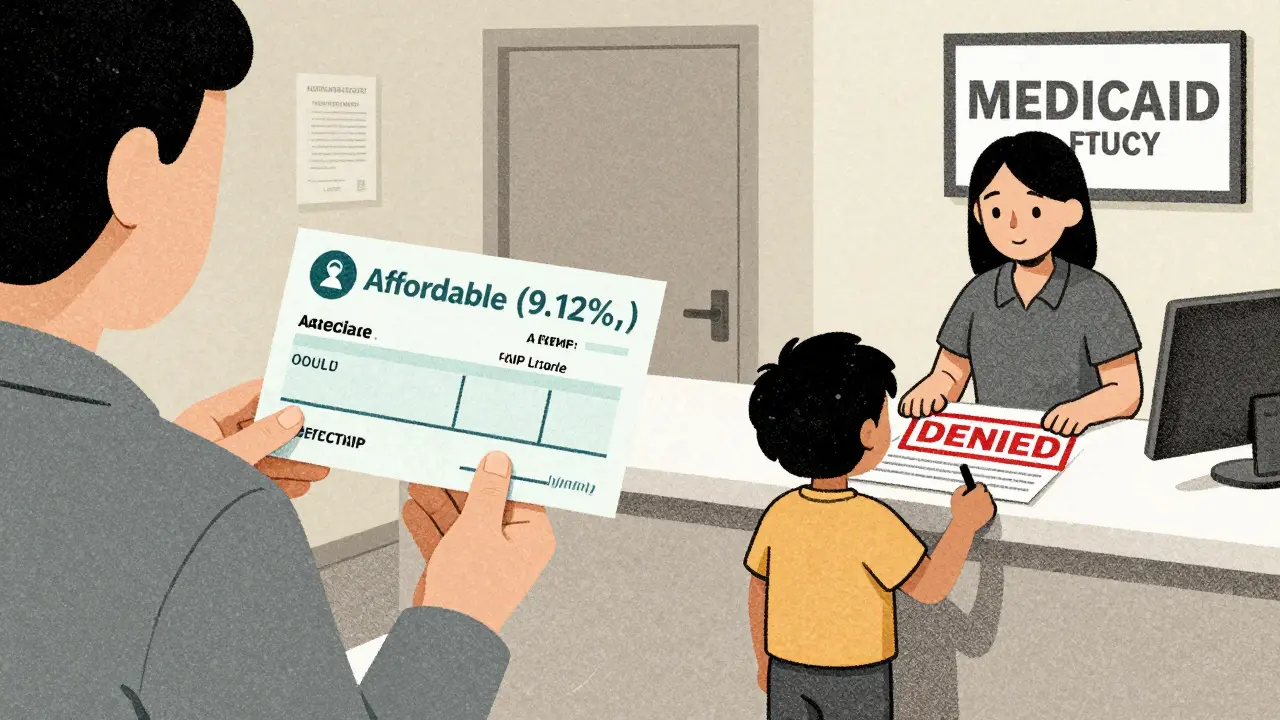
Medicaid substitution rules exist to stop public health programs like Medicaid and CHIP from stepping in when a child already has access to affordable private insurance. These rules aren’t about denying care-they’re about making sure public money goes to families who truly need it. Under federal law, states can’t let CHIP cover a child if that child’s parent has access to employer-sponsored insurance that costs less than 9.12% of the family’s income. This is based on Section 2102(b)(3)(C) of the Social Security Act, updated by the Affordable Care Act in 2010 and tightened again in March 2024 by CMS.
Think of it like this: if your employer offers health insurance and you can afford it, Medicaid shouldn’t pay for your kid’s doctor visits instead. The goal is to protect private insurance markets and keep public funds focused on those without any other options. In 2019, over 1.2 million children were potentially caught in this gray area, and states spent roughly $1.8 billion covering kids who might have had private coverage. Without these rules, that number could jump by $2.1 billion annually.
Mandatory Rules: What All States Must Do
Every state that runs a CHIP program is required by federal law to have substitution prevention measures in place. This isn’t optional. The core rule, spelled out in 42 CFR 457.805(a), says states must design systems to make sure CHIP doesn’t replace private coverage. That means they need clear processes to check whether a child’s family has access to affordable group health insurance.
States must also follow specific rules for handling waiting periods. If a parent loses their job or switches employers, there’s often a gap before new coverage kicks in. Federal law allows states to impose a waiting period of up to 90 days before CHIP eligibility starts-but they can’t make it longer. During that time, states must help families transition to other affordable options, like premium tax credits under the ACA. This is required under 42 CFR 457.340(d)(3) and 457.350(i).
States also have to make sure their eligibility systems can verify private insurance. That means checking whether premiums are affordable, whether the plan covers essential benefits, and whether the employer actually offers coverage to the employee. Many states use the National Association of Insurance Commissioners’ database to do this, but not all have the tech to do it in real time. In 2023, 68% of state Medicaid workers said verifying private insurance was their biggest headache, with average verification taking over two weeks.
Optional Rules: How States Go Beyond the Minimum
While the core substitution rule is mandatory, how states enforce it varies widely. One big choice: whether to use a waiting period. As of 2024, 34 states use the 90-day waiting period as their main tool to prevent substitution. That includes big states like California, New York, and Texas. But 16 states don’t use waiting periods at all-they rely on database checks or household surveys to determine if private coverage is available.
Some states go even further. Fifteen states, including Florida, Illinois, and Pennsylvania, have added extra exemptions to the waiting period. For example, if a parent loses hours at work or gets laid off, their child might get immediate CHIP access-even if they technically had insurance before. These exemptions recognize that today’s job market is unstable. A parent might lose coverage on Friday and need help Monday. The old 90-day rule doesn’t fit that reality.
Another optional choice is whether to integrate Medicaid and CHIP eligibility systems. As of 2024, 32 states have combined their systems. That means when a child’s income changes or a parent switches jobs, the system automatically checks eligibility for both programs. These states see 22% fewer coverage gaps than those with separate systems. States like Minnesota, Massachusetts, and Oregon have built automated bridges between programs. In Minnesota’s Bridge Program, real-time data sharing cut substitution-related coverage gaps by 63%.
Why Some States Struggle With Implementation
Even with clear rules, implementation is messy. One major problem: verifying whether private insurance is truly affordable. Employers might offer coverage, but if premiums eat up 12% of a family’s income, it’s not affordable under federal guidelines. But many states still rely on paper forms, faxed documents, or phone calls to confirm this. A Medicaid worker in Ohio told a Reddit thread: “We get families who lose coverage on Friday and need CHIP Monday. But the 90-day rule forces us to deny them for 12 weeks-they often end up uninsured.”
On the flip side, Texas CHIP administrators worry that without waiting periods, parents might drop their employer coverage just to get free CHIP. One administrator said: “We’d see churning-families switching back and forth to game the system.” That’s real. In states with looser rules, some families do drop private insurance to qualify for Medicaid. That costs states millions.
Another issue? Documentation. The National Academy for State Health Policy rated 19 states’ substitution guidance as “comprehensive,” but 12 states’ materials were labeled “inadequate for frontline staff.” That means eligibility workers are guessing how to apply the rules. In Louisiana, a strict 2021 policy led to a 4.7 percentage point spike in uninsured children because families couldn’t navigate the bureaucracy.
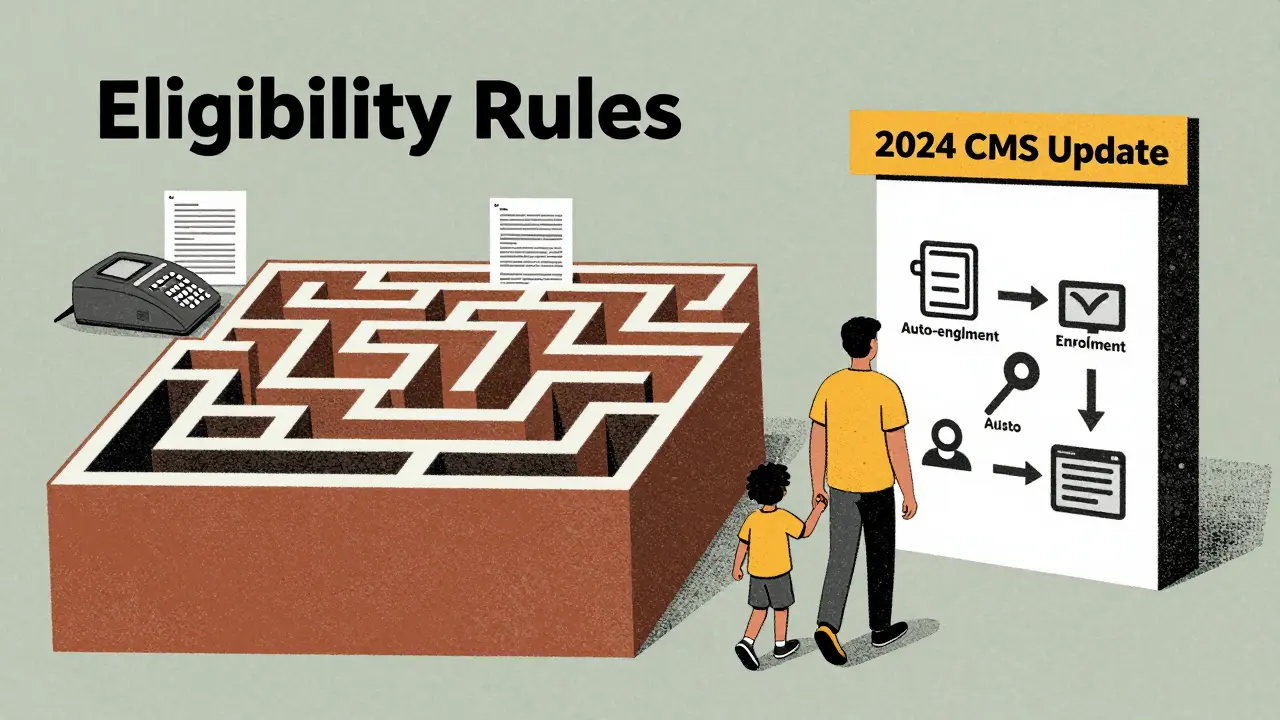
What Changed in the 2024 Rule Update
The big shift came in March 2024, when CMS rolled out its new Medicaid and CHIP Eligibility and Enrollment rule. It didn’t scrap substitution rules-it fixed their flaws. The new rule requires states to create automatic transitions between Medicaid and CHIP. If a child’s income drops and they lose CHIP, they should be enrolled in Medicaid without filling out a new form. Same if they gain income and qualify for private coverage-systems should push them toward it.
States now have to share data between programs. That means if a parent applies for CHIP and their income is just above the Medicaid limit, the system should automatically check if they qualify for premium tax credits. This reduces paperwork and closes coverage gaps. States must have these systems in place by October 1, 2025.
Another change: states must now accept eligibility decisions from other insurance affordability programs. If someone gets approved for a marketplace plan, that counts as proof they have coverage-no need to re-verify. This rule takes full effect by December 31, 2025.
CMS also requires states to start reporting quarterly on substitution-related metrics: how many kids had coverage gaps, how often waiting periods were used, how many exemptions were granted. That transparency will help identify which approaches actually work.
Real-World Impact: Successes and Failures
Some states have cracked the code. Minnesota’s Bridge Program uses real-time data from private insurers to auto-enroll kids in CHIP the moment they lose employer coverage. The result? Coverage gaps dropped from 21% to under 8%. Oregon does something similar, pulling data from hospitals and clinics to catch kids slipping through the cracks.
Meanwhile, failure stories are just as telling. Louisiana’s 2021 crackdown caused a spike in uninsured children. A 2023 Families USA survey found 42% of parents cited “bureaucratic delays” as their main frustration during transitions. But 31% said the rules helped-because they kept employers from dropping coverage they were supposed to offer.
Experts are split. Dr. Leighton Ku of George Washington University says the 90-day waiting period is outdated. “Job changes happen every few months now,” he testified in early 2024. “These rules were made for a world where people stayed at one job for decades.”
But the Medicaid and CHIP Payment and Access Commission (MACPAC) argues the rules still save money-$1.3 billion a year since 2010. Without them, more families would switch from private to public insurance, straining state budgets.
What’s Next for Medicaid Substitution Rules?
CMS plans to update its CHIP eligibility matching guidance in 2025, based on data from the first year of the new rule. Analysts at Manatt Health predict that by 2027, every state will use automated data matching to monitor substitution. That could cut manual verification by 65%.
But there’s a warning: the Urban Institute says if no further updates happen, substitution rules could lose 25% of their effectiveness by 2030. Why? Because the insurance market keeps changing. Short-term plans are growing. Gig work is rising. Employers offer more part-time roles with no benefits. The rules were built for a different economy.
Some advocates, like Joan Alker from Georgetown, argue these rules punish working families. “If you hold two jobs to make ends meet, you’re penalized for it,” she says. Others, like NASHP, say states need more flexibility to design rules that fit their local markets.
CMS Administrator Chiquita Brooks-LaSure said in May 2024 that the agency will review the first year of data and decide if more changes are needed-possibly by late 2026. The goal isn’t to eliminate substitution rules. It’s to make them smarter, faster, and fairer.
How Families Can Navigate These Rules
If you’re a parent trying to get CHIP for your child:
- Know your employer’s coverage details-premiums, deductibles, and whether it’s considered affordable (under 9.12% of income).
- If you lost a job, ask if your former employer offers COBRA or if you qualify for a special enrollment period on the marketplace.
- Apply for CHIP immediately-even if you think you might be denied. Some states have automatic exemptions you don’t know about.
- Ask your state Medicaid office if they have a “bridge program” or real-time data system. States like Minnesota and Oregon have them.
- If you’re denied and believe it’s wrong, file an appeal. Many denials happen because of paperwork delays, not actual ineligibility.
The system isn’t perfect, but it’s getting better. The 2024 rule is the biggest step forward in over a decade. What matters now is whether states have the resources and will to make it work.
Are Medicaid substitution rules the same in every state?
No. While all states must follow the federal mandate to prevent CHIP from replacing affordable private insurance, how they do it varies. Thirty-four states use a 90-day waiting period, while 16 rely on database checks or surveys. Fifteen states offer extra exemptions for job loss or reduced hours. Some have integrated Medicaid-CHIP systems that auto-enroll kids; others still use paper forms.
Can a family be denied CHIP just because they have employer coverage?
Only if that coverage is considered affordable-meaning the employee’s share of premiums is less than 9.12% of household income for 2024. If the plan is too expensive, or if the employer doesn’t offer it to the employee (only to dependents), the child may still qualify for CHIP. States must verify affordability before denying coverage.
What happens if a parent loses their job and their child loses private insurance?
If the parent loses coverage due to job loss, many states allow immediate CHIP enrollment-even if a waiting period normally applies. Fifteen states, including Illinois and Pennsylvania, have added this exemption. But in states without it, families may face a 90-day gap. The 2024 CMS rule now requires states to help families transition to other affordable options during that time, like marketplace subsidies.
Why do some states have longer delays in approving CHIP?
Delays usually come from manual verification. States that still rely on paper forms, faxes, or phone calls to confirm private insurance can take up to 14 days to verify coverage. States with automated systems that pull data directly from insurers process applications in hours. The 2024 rule pushes all states toward automation by October 2025.
Do substitution rules make children more likely to be uninsured?
Yes, in some cases. Before the 2024 rule, 21% of children experienced coverage gaps when switching between Medicaid and CHIP. In states with strict waiting periods and poor support systems, like Louisiana in 2021, the uninsured rate for low-income children spiked. But states with automated transitions, like Minnesota, kept gaps below 8%. The problem isn’t the rule-it’s how it’s enforced.






14 comments
Aboobakar Muhammedali
I've seen families in my neighborhood get denied CHIP because their employer 'offered' insurance that cost 11% of their pay. They worked two jobs just to make ends meet, and now the kid's asthma meds are on hold. This isn't policy-it's cruelty disguised as fiscal responsibility.
Why do we punish people for trying?
anthony funes gomez
The structural inefficiency inherent in state-level Medicaid-CHIP substitution enforcement mechanisms is a classic case of regulatory misalignment with labor market dynamics. The 90-day waiting period-originally predicated on stable, full-time employment paradigms-is now functionally obsolete in the context of gig economy volatility, contingent labor arrangements, and non-standard work hours. The ACA’s 9.12% affordability threshold, while mathematically precise, fails to account for income volatility, non-wage benefits, and the psychological burden of administrative burden on low-income households. Without real-time, interoperable data infrastructure, we're applying 20th-century logic to 21st-century socioeconomic realities.
Kathryn Featherstone
If you're a parent and you're reading this, don't give up. Apply anyway. Even if you get denied, ask for a written explanation and file an appeal. I’ve helped three families in my town get CHIP after they were turned down-turns out, the worker just missed the exemption for job loss. It’s not perfect, but the system *can* work if you push back.
You’re not being a burden. You’re fighting for your kid.
Mark Able
Wait so you're telling me Texas is worried about people gaming the system but doesn't have the tech to verify insurance in under two weeks? That’s not a policy problem-that’s a government incompetence problem. Why are we still faxing documents in 2024? I’ve got a 2018 iPhone that does more than half these state systems.
Someone’s getting paid to keep this broken.
Dorine Anthony
I work in a pediatric clinic. We see the fallout every day. Kids show up with untreated asthma because their mom got denied CHIP while waiting for COBRA to kick in. Or worse-they get denied because the system says 'affordable insurance' exists, but the parent can’t afford the deductible. The rules are fine. The implementation? A disaster.
Marsha Jentzsch
Oh my GOD. I just found out my cousin’s kid got denied because the state said the dad had ‘access’ to insurance-BUT THE DAD WORKS NIGHTS AND THE PLAN ONLY COVERS DAYTIME CLINICS. So the kid can’t even use it. And now they’re paying $800 a month out of pocket. This isn’t about saving money-it’s about punishing poor people for being poor. Who designed this? A robot? A politician on a yacht?
Henry Marcus
You think this is about money? Nah. This is a covert plan by private insurers to keep Medicaid weak so they can jack up premiums. The 9.12% rule? A trap. They engineer employer plans to look ‘affordable’ by cutting coverage to the bone-then when you need real care, you’re screwed. The government’s just doing their bidding. Watch. By 2027, all Medicaid data will be sold to insurers. They’re already testing it in Arizona.
Carolyn Benson
The fact that we’re still debating whether a 90-day waiting period is ‘too long’ proves how detached we are from reality. We live in a world where people change jobs every 18 months, where gig platforms drop coverage like trash, and yet we’re clinging to a bureaucratic relic from the Reagan era. This isn’t fiscal responsibility-it’s ideological laziness. We don’t need more rules. We need to abolish the entire substitution framework and treat healthcare as a human right, not a conditional benefit.
Aadil Munshi
Let’s be real-this whole system is designed to make poor people jump through hoops so the rich don’t have to pay taxes. The 1.2 million kids caught in the gray zone? They’re not ‘potential’ cases-they’re real kids with real asthma, diabetes, ADHD. And the $1.8 billion spent? That’s chump change compared to what we waste on tax breaks for billionaires. You know what’s cheaper than CHIP? Preventing kids from ending up in ERs because they went untreated for six months. But hey, let’s keep punishing parents for working hard.
Danielle Stewart
If you’re applying for CHIP and you’re stuck in limbo, call your state’s Medicaid ombudsman. They exist for a reason. Most people don’t know they’re there. I used to work for one. We helped 700 families last year just by walking them through the appeals process. You’re not alone. And yes, Minnesota’s Bridge Program works. It’s not magic-it’s just data sharing. Why can’t every state do it? Because they don’t want to.
But you can still fight for your kid.
mary lizardo
The grammatical and syntactical incoherence of state-level eligibility documentation is symptomatic of a broader institutional decay. The use of ‘affordable’ as a proxy for ‘accessible’ is a lexical fallacy. Furthermore, the conflation of ‘employer-sponsored insurance’ with ‘adequate pediatric coverage’ constitutes a category error of alarming magnitude. One cannot, in good faith, assert that a plan with a $10,000 deductible and no pediatric specialist network is ‘affordable’-it is merely non-zero.
Sajith Shams
You think Louisiana’s spike in uninsured kids was because of bureaucracy? Nah. It’s because they stopped giving free snacks to the Medicaid workers. Jk. But seriously-why do we treat parents like criminals? If you’re working two jobs and still can’t afford insurance, you’re not a fraud. You’re the American dream. And we’re punishing you for it.
shivam seo
Australia doesn’t have this mess. We have Medicare. If your kid needs a doctor, they get one. No forms. No waiting. No ‘affordability thresholds’. You want to know why we don’t have uninsured kids? Because we don’t let capitalism decide who lives or dies. This US system is a joke. A sad, expensive, bureaucratic joke.
Andrew Kelly
Let’s not forget who benefits here. The insurance lobbyists. The hospital chains. The private equity firms that buy up Medicaid contracts. This isn’t about saving money-it’s about control. The 2024 rule? A PR stunt. They’ll automate the system just enough to look good, then quietly gut the exemptions. Wait till 2026. Watch how ‘flexibility’ disappears when the next election rolls around.