Drinking herbal tea feels harmless-warm, soothing, natural. But if you’re on medication, that cup of chamomile or hibiscus could be doing more than calming your nerves. It might be quietly messing with your prescription drugs. You don’t need to stop drinking tea. But you do need to know which ones could be risky.
Why Herbal Teas Aren’t Just ‘Herbal’
Herbal teas aren’t tea in the traditional sense. They don’t come from the Camellia sinensis plant. Instead, they’re made from roots, flowers, leaves, or seeds of other plants-chamomile, peppermint, hibiscus, ginger, St. John’s wort, green tea (yes, green tea is technically an herbal tea in this context), and more. People drink them for sleep, digestion, immunity, or just because they taste good. But these plants contain powerful chemicals. Some act like drugs in your body. And when those chemicals meet prescription medications, things can go wrong.Unlike real medicines, herbal teas don’t go through rigorous safety testing before they hit the shelf. The FDA treats them as food, not drugs. That means no proof of safety, no required labeling about side effects, and no warnings about interactions. You can buy a bag labeled ‘Sleep Aid’ or ‘Heart Support’ without knowing what’s really inside-or how it might react with your blood pressure pill or antidepressant.
Green Tea: The Silent Drug Thief
Green tea is one of the most common herbal teas worldwide. It’s often praised for antioxidants. But its active compound, epigallocatechin gallate (EGCG), is a powerful inhibitor of drug transporters in your gut and liver. This means it can block your body from absorbing certain medications properly.Studies show green tea can slash the effectiveness of the cholesterol drug atorvastatin by up to 39%. It can reduce levels of the beta-blocker nadolol by 85%. That’s not a small drop. That’s enough to make your medication useless. If you’re on nadolol for heart rhythm or high blood pressure, drinking three strong cups of green tea daily could mean your heart isn’t protected.
It doesn’t stop there. Green tea also interferes with fluoroquinolone antibiotics, antiretrovirals for HIV, and even imatinib, a cancer drug. The effect is strongest with concentrated extracts, but even brewed tea-especially if steeped long or strong-can cause issues. If you take any of these medications, talk to your doctor before sipping green tea regularly.
St. John’s Wort: The Mood Booster That Kills Other Meds
St. John’s wort is popular for mild depression. But it’s one of the most dangerous herbal teas when mixed with medications. It triggers enzymes in your liver that break down drugs faster. That means your body clears the medication before it has time to work.It can drop levels of birth control pills so low that you risk pregnancy. It can make antidepressants like SSRIs ineffective-or worse, cause serotonin syndrome, a life-threatening condition. It reduces the effectiveness of cyclosporine (used after organ transplants), warfarin (a blood thinner), and even some HIV drugs. In one study, people on cyclosporine who started St. John’s wort saw their drug levels drop by over 50% in just two weeks.
If you’re taking any prescription drug, especially for mental health, heart conditions, or immune suppression, avoid St. John’s wort tea completely. There’s no safe amount.
Chamomile and Birth Control: A Hidden Risk
Chamomile tea is gentle. It’s often recommended for anxiety or insomnia. But it contains apigenin, a compound that can interfere with how your body metabolizes hormones. Early research suggests it may reduce the effectiveness of oral contraceptives by affecting the CYP3A4 enzyme system-the same system that breaks down estrogen and progesterone.While human studies are limited, the risk is real enough that doctors in Europe and the U.S. now warn women on birth control to avoid large amounts of chamomile tea. One case report described a woman who got pregnant after switching from black tea to chamomile daily. She had no other changes. The tea was the only variable.
If you’re relying on birth control pills, patches, or rings, don’t treat chamomile as harmless. Limit it to occasional sips. And if you’re trying to get pregnant, chamomile might be helping more than you think.

Hibiscus Tea: The Natural Blood Pressure Drop That Goes Too Far
Hibiscus tea is tart, colorful, and often marketed as a natural way to lower blood pressure. And it works. Studies confirm it can reduce systolic pressure by 7-13 mmHg. That sounds great-until you’re already on blood pressure medication.When hibiscus is combined with lisinopril, enalapril, or other ACE inhibitors, the effect can be too strong. There are documented cases of patients dropping their blood pressure below 90 mmHg systolic, leading to dizziness, fainting, and falls. One 72-year-old woman on lisinopril started drinking two cups of hibiscus tea daily. Within a week, she passed out while cooking. Her blood pressure was 84/52.
If you have low blood pressure-or are on any blood pressure medication-drink hibiscus tea with extreme caution. Monitor your pressure. If you feel lightheaded, stop immediately.
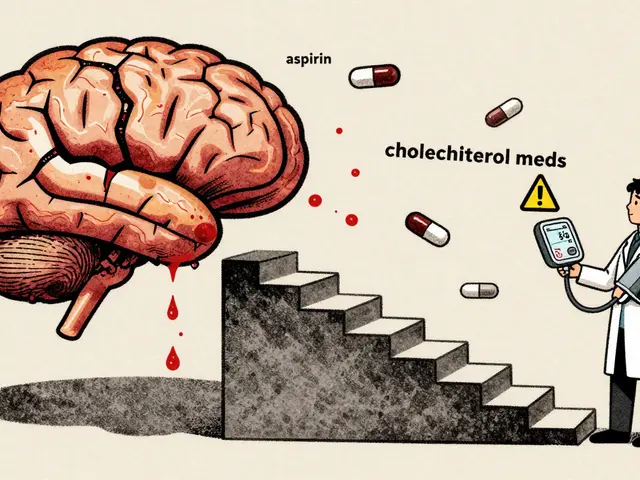
Warfarin and the Bleeding Risk Trio
Warfarin is a blood thinner used to prevent strokes and clots. It has a very narrow safety window. Too little, and you risk a clot. Too much, and you bleed internally. Even small changes in diet or supplements can throw it off.Three herbal teas are known to increase bleeding risk when taken with warfarin: ginkgo biloba, ginger, and chamomile. Ginkgo is especially dangerous. It inhibits platelet function. A 2022 Mayo Clinic review documented multiple cases of brain bleeds and gastrointestinal bleeding in patients who took ginkgo tea while on warfarin.
Garlic and cranberry are also flagged. Some studies say cranberry increases INR (the blood-thinning measure), others say it doesn’t. But the risk isn’t worth guessing. If you’re on warfarin, avoid ginkgo tea entirely. Limit ginger and chamomile to one cup a week. And always tell your doctor what teas you drink.
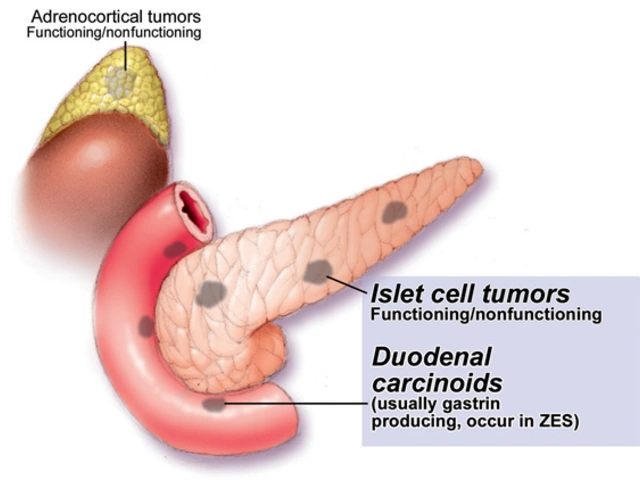
Goldenseal: The Hidden Enzyme Blocker
Goldenseal is often sold as a cold remedy or immune booster. It’s sometimes brewed as a tea. But it’s one of the most potent inhibitors of liver enzymes CYP2D6 and CYP3A4. These enzymes process over half of all prescription drugs.Goldenseal can raise levels of drugs like codeine, metoprolol, and certain antidepressants to toxic levels. It can also make statins, anti-anxiety meds, and some cancer drugs build up dangerously in your blood. A single cup of strong goldenseal tea can last in your system for days.
There’s no safe dose if you’re on medication. Avoid goldenseal tea completely.
What You Should Do Right Now
You don’t need to quit herbal tea. But you do need to take control.- Make a list of every tea, supplement, or herb you take daily-even if you think it’s harmless.
- Bring it to every doctor’s visit. Don’t wait to be asked. Say, “I drink these teas. Are they safe with my meds?”
- Know your high-risk meds: Warfarin, digoxin, cyclosporine, theophylline, lithium, statins, beta-blockers, antidepressants, birth control, and antiretrovirals. If you take any of these, assume your tea might interact.
- Start low, go slow. If you want to try a new tea, begin with one cup every other day. Watch for dizziness, nausea, unusual bruising, or changes in heart rate.
- Don’t trust labels. “All-natural” doesn’t mean safe. “No caffeine” doesn’t mean no drug interactions.
When to See a Pharmacist or Doctor
If you’re on more than three medications (polypharmacy), you’re at higher risk. Older adults are especially vulnerable. The Mayo Clinic found that nearly 70% of seniors take herbal products, but only a quarter tell their doctors.See a pharmacist if you’re unsure. Pharmacists are trained in drug interactions and can check your tea and meds together. They don’t judge. They help.
Call your doctor immediately if you notice:
- Unexplained bruising or bleeding
- Dizziness, fainting, or rapid heartbeat
- Worsening symptoms of your condition (e.g., higher blood pressure, more anxiety)
- Changes in sleep, appetite, or mood
These could be signs your tea is interfering with your medicine.
The Bottom Line
Herbal teas aren’t the enemy. But they’re not harmless either. They’re active substances. They interact. They change how your body handles medicine. And if you’re on a drug with a narrow therapeutic window-like warfarin, digoxin, or birth control-that change can be dangerous.You don’t need to live in fear. Just be informed. Talk to your provider. Keep a list. Pay attention to your body. And remember: natural doesn’t mean safe. Just because something grows in the ground doesn’t mean it won’t hurt you when mixed with pills.
Can I drink chamomile tea while on birth control?
It’s best to avoid daily chamomile tea if you’re on hormonal birth control. Chamomile may interfere with how your body breaks down estrogen and progesterone, potentially reducing the pill’s effectiveness. Occasional sips are likely fine, but don’t make it a daily habit. Talk to your doctor if you’re unsure.
Is green tea safe with statins?
No, not if you drink it regularly or strongly brewed. Green tea can reduce the absorption of statins like atorvastatin by up to 39%, making them much less effective. If you’re on a statin, limit green tea to one weak cup a day-or avoid it entirely. Ask your doctor for alternatives.
Does hibiscus tea lower blood pressure too much?
Yes, especially if you’re already taking blood pressure medication. Hibiscus tea works like an ACE inhibitor. When combined with lisinopril or similar drugs, it can cause your blood pressure to drop dangerously low-leading to dizziness or fainting. Monitor your pressure closely or avoid it altogether.
Can I drink ginger tea if I’m on blood thinners?
Ginger tea can increase bleeding risk when taken with warfarin or other blood thinners. While small amounts (one cup a week) are usually okay, regular use can raise your INR and lead to bruising or internal bleeding. Avoid daily ginger tea if you’re on anticoagulants.
What herbal teas are safest with medications?
Peppermint, rooibos, and licorice root tea (in moderation) have the lowest known interaction risks. But even these aren’t risk-free. Always check with your doctor or pharmacist before adding any new tea, especially if you take multiple medications.
Why don’t tea labels warn about drug interactions?
Because herbal teas are sold as food, not medicine, in the U.S. and many other countries. The FDA doesn’t require safety testing or interaction warnings before they’re sold. That means you have to be your own advocate. Don’t assume a tea is safe just because it’s labeled “natural.”



14 comments
Jackie R
Stop pretending herbal tea is harmless. If you’re on meds, you’re playing Russian roulette with your life. Natural doesn’t mean safe-your grandma’s remedies got people killed before modern medicine. Wake up.
Chamomile with birth control? That’s not a ‘maybe’-it’s a pregnancy waiting to happen. Green tea with statins? You’re not ‘health-conscious,’ you’re just dumb.
Stop drinking tea like it’s candy. Your body isn’t a lab experiment.
And if you’re one of those ‘I drink it for the taste’ people? You’re the reason this post needed to exist.
Stop.
Just stop.
Josh Arce
bro but what if i just drink one cup a week? like, i dont drink it daily. its just for chillin. like, its not like i’m chugging it. its tea. not a pill. why are we making this so hard?
also green tea has antioxidants. how is that bad? isnt that good? idk man.
Eli Grinvald
thank you for writing this 🙏 i’ve been on warfarin for 3 years and had no idea ginger tea could be risky. i’ve been drinking it every morning for ‘digestion’ 😅 i’m switching to rooibos now. also-why does no one tell you this stuff? it’s wild.
ps: i cried reading the hibiscus story. that poor woman. ❤️
Alexis Hernandez
Okay real talk: herbal tea isn’t the villain here. The system is. Why are we letting companies sell ‘Sleep Aid’ tea with zero labeling? Why does the FDA treat this like it’s a bag of chips?
I get it-you want to feel in control of your health. But if you’re on meds and you’re sipping ‘natural’ stuff without checking, you’re not being proactive-you’re being vulnerable.
Here’s what I do: I keep a little notebook. Every tea, every supplement, every ‘herbal remedy’ I take. I bring it to my pharmacist every 3 months. They don’t judge. They just say, ‘Dude, don’t do that with your blood pressure med.’
And honestly? That’s the real hero here: the pharmacist. Not the tea. Not the doctor who forgets to ask. The pharmacist.
Go talk to one. Seriously. They’re the unsung heroes of modern medicine.
Also-rooibos is your new best friend. Tastes like caramel. Zero drama.
And no, I’m not sponsored. I just don’t want you to end up in the ER because you thought ‘herbal’ meant ‘harmless.’
brajagopal debbarma
lol so now even tea is dangerous? next they will say water is bad for your kidneys if you take pills. why not just take pills and stop drinking anything? then you will be safe. ha ha.
my grandma drank hibiscus tea for 60 years. she is 92 and still beats me at chess. what do you say to that?
Carly Smith
so you’re saying i can’t drink my hibiscus tea anymore? like… seriously? i like the color. it’s pretty. and it makes me feel like i’m in a nature documentary. now i have to worry about my blood pressure? i don’t even know what my blood pressure is. why do you make everything so complicated? i just want to sip something warm and red and feel fancy.
also why is everyone so scared of chamomile? it’s like a hug in a cup. chill out.
and stop telling me what to do. i’m an adult.
also i don’t have a doctor. so what now? i guess i’ll just keep drinking my tea and hope for the best.
thanks for the guilt trip
Kurt Stallings
Regulatory arbitrage at its finest. The FDA’s classification of botanicals as food is a legal fiction that enables corporate negligence. The pharmacokinetic interactions are well-documented in peer-reviewed literature, yet consumer awareness remains negligible due to market-driven ignorance.
Green tea’s inhibition of CYP3A4 and P-gp is not speculative. It’s quantifiable. The 39% reduction in atorvastatin bioavailability is not a suggestion. It’s a clinical reality.
People who drink tea for ‘wellness’ are participating in a performative pseudoscience. The ritual is comforting. The risk is not.
Stop romanticizing plants. They are biochemical agents. Treat them like it.
Angie Creed
Let’s be real-this isn’t about tea.
This is about control.
We’ve been conditioned to believe that if it’s ‘natural,’ it’s good. If it’s ‘chemical,’ it’s evil. But the truth? The only thing that matters is the molecule. Whether it came from a lab or a leaf-it doesn’t care. It interacts the same way.
St. John’s Wort isn’t evil. It’s just a very efficient enzyme inducer. Chamomile isn’t a villain-it’s a CYP3A4 modulator. The problem isn’t the tea. It’s the illusion that we can outsmart biochemistry with a cozy ritual.
We want to believe that we can heal ourselves with warmth and scent. But medicine isn’t poetry. It’s physics.
And physics doesn’t care how you feel about it.
So yes. You can drink your tea.
But stop pretending it’s innocent.
And if you’re on warfarin? Don’t be the person who says ‘I didn’t know.’
You knew.
You just didn’t want to face it.
Michael Ferguson
Look, I’ve been on six different meds for the last 12 years. I’ve been on warfarin, statins, antidepressants, thyroid meds, blood pressure pills, and a couple others I can’t even remember the names of. I’ve read every single study. I’ve talked to three different pharmacists. I’ve even emailed the FDA. And here’s what I know: people are dying because they think ‘herbal’ means ‘safe.’
And it’s not just tea. It’s turmeric capsules, ashwagandha gummies, garlic pills, even CBD oil. Everyone thinks they’re ‘boosting their immunity’ or ‘cleansing their liver’ like it’s a TikTok trend.
But here’s the thing: your liver doesn’t care if it’s ‘organic’ or ‘cold-pressed.’ It only cares about the chemical structure. And if you’re on anything with a narrow therapeutic window-warfarin, digoxin, cyclosporine, lithium-you are playing with fire.
I lost a friend last year. 68. Healthy. Ate clean. Drank chamomile tea every night. Took blood thinners. Got a brain bleed. No warning. No symptoms. Just… gone.
So no. I’m not being dramatic. I’m being real.
You think you’re being healthy? You’re being reckless.
And if you’re one of those people who says ‘I’ve been doing it for years and I’m fine’? You’re just lucky. Not smart.
And luck runs out.
So make the list. Talk to the pharmacist. Stop treating your body like a DIY project.
Because when it breaks, you won’t be able to Google your way out of it.
Patrick Klepek
Interesting. I’ve been drinking ginger tea with my warfarin for years. Never had a problem. But I also check my INR every two weeks. Maybe that’s the difference? Not avoiding the tea-but monitoring the outcome.
Also, I think the real issue isn’t tea. It’s that we’re not taught how to talk to our doctors about supplements. They don’t ask. We don’t say. And then we’re surprised when things go wrong.
Maybe we need a ‘tea and meds’ checklist at pharmacies? Like, ‘Did you drink any herbal teas this week?’
Just a thought.
Also-rooibos is delicious. Try it. No caffeine. No drama. Just sweet, earthy goodness.
Sebastian Brice
I’m a nurse. I’ve seen this happen too many times. A patient comes in with a bleeding ulcer. Turns out they’ve been drinking three cups of ginger tea a day and taking warfarin. They didn’t think it mattered.
Another one had a stroke because their birth control stopped working after switching to chamomile. She thought it was ‘just a calming tea.’
Here’s what I tell my patients: if you wouldn’t give it to your dog without checking with your vet, don’t give it to yourself without checking with your pharmacist.
And yes, I know it’s annoying. I know it’s ‘just tea.’ But medicine isn’t about convenience. It’s about survival.
So make the list. Bring it to your next appointment. Ask the question.
It’s not about fear.
It’s about being smart.
And honestly? You’re already doing better than most people just by reading this post.
Jim Aondongu
in nigeria we drink ginger tea with everything and no one dies. my uncle takes blood pressure pills and drinks hibiscus every day. he is 78 and still runs his shop. you americans make everything a crisis. tea is tea. if you are sick go to hospital not internet.
also why is everyone so scared of natural things? in africa we use herbs for medicine because they work. why is your system so broken that you fear what grows in the ground?
Michael Schaller
My mom took warfarin for 10 years. She drank one cup of chamomile tea every night. Never had an issue. But she also had her INR checked every week. She kept a log. She told her doctor every time she added something new.
It’s not about banning tea. It’s about awareness. And consistency.
If you’re on meds and you’re not monitoring your body’s response, you’re not being careful-you’re being careless.
But if you’re informed? You can still enjoy your tea.
Just don’t pretend it’s magic.
It’s medicine. Even the quiet stuff.
Jackie R
And yet, people still don’t get it. You don’t get to cherry-pick science when it fits your lifestyle. If you’re on warfarin and you drink ginger tea, you’re not ‘living your truth.’ You’re gambling with your organs.
And if you think your uncle in Nigeria is proof it’s safe? He’s lucky. Not right. One in a million. That’s not a rule-it’s an accident waiting to be repeated.
Stop glorifying ignorance. It’s not cultural. It’s dangerous.