When you pick up a prescription for a generic drug, you might not think about how it’s organized in a database, classified by doctors, or grouped by insurance plans. But behind every pill, capsule, or injection is a complex system designed to keep you safe, make prescribing easier, and control costs. These systems aren’t random-they’re carefully built frameworks called generic drug classifications, and understanding them helps you make smarter choices about your health. There are five main ways drugs are classified, each serving a different purpose. Some are used by doctors to decide what to prescribe. Others guide pharmacists in filling prescriptions. Some are legal tools. And a few are purely financial. Knowing how these systems work means you’re not just taking a pill-you’re understanding why it’s prescribed, why it costs what it does, and why sometimes, two identical drugs end up in different places.
Therapeutic Classification: What the Drug Treats
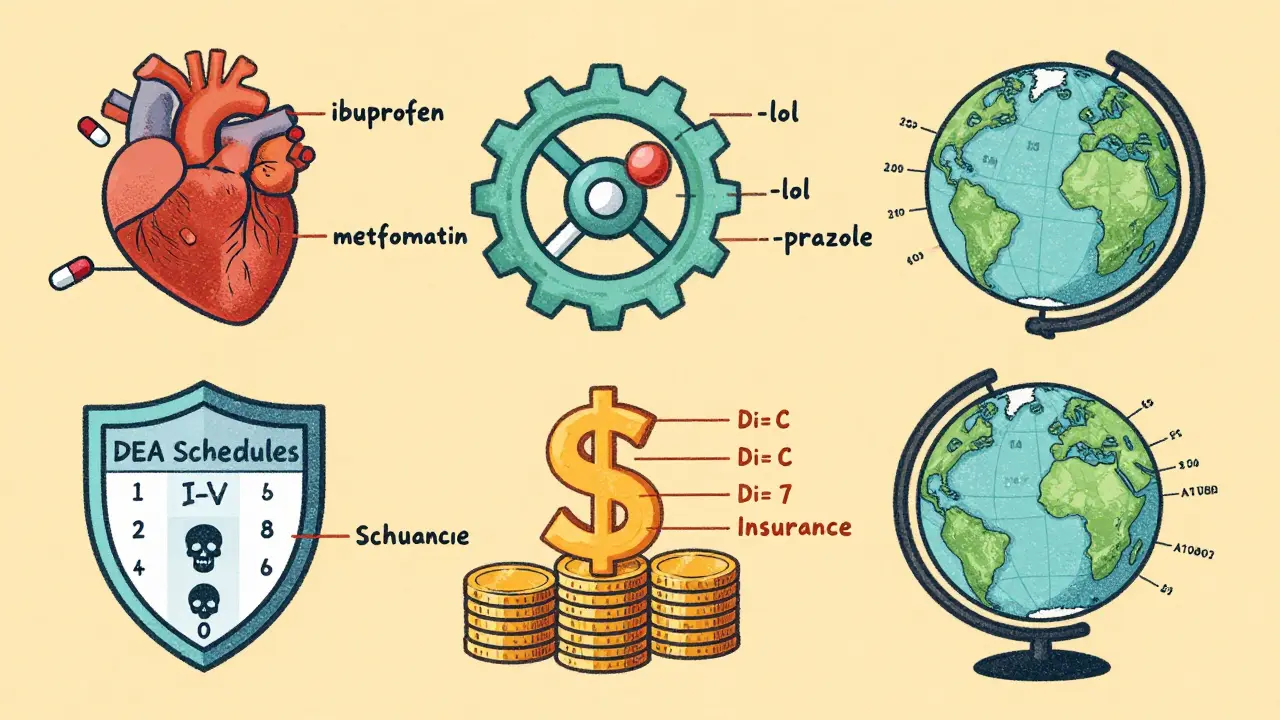
This is the most common way doctors and hospitals group drugs. It’s simple: what condition does it treat? If a drug lowers blood pressure, it’s a cardiovascular agent. If it kills cancer cells, it’s an antineoplastic. If it reduces pain, it’s an analgesic. The FDA and USP (United States Pharmacopeia) maintain the official USP Therapeutic Categories Model, which breaks down drugs into over 300 specific categories. For example, under “Analgesics,” you’ll find subcategories like Non-opioid Analgesics (ibuprofen, acetaminophen) and Opioid Analgesics (oxycodone, morphine). Under “Endocrine Agents,” you’ll see insulin, levothyroxine, and metformin. This system shines in clinical settings. A nurse checking a medication order can quickly tell if a drug belongs in the right category. A hospital formulary uses it to decide which drugs to stock. Studies show hospitals using standardized therapeutic classification reduce medication errors by 31%. But it’s not perfect. Some drugs treat more than one thing. Aspirin, for example, is used for pain, fever, and preventing heart attacks. Do you put it under analgesics or anticoagulants? The system forces a choice, which can confuse prescribers. That’s why the FDA is rolling out Therapeutic Categories Model 2.0 in 2025, allowing drugs to have a primary and secondary indication.Pharmacological Classification: How the Drug Works
While therapeutic classification asks what the drug does, pharmacological classification asks how it does it. This system dives into the science. It groups drugs by their mechanism of action-how they interact with cells, receptors, or enzymes. For instance, beta-blockers like metoprolol and propranolol all block adrenaline receptors in the heart. That’s why their names end in “-lol.” Proton pump inhibitors like omeprazole and pantoprazole all shut down stomach acid production-hence the “-prazole” ending. There are over 1,200 distinct pharmacological classes recognized today. The USP has formalized 87 naming stems to help identify these classes just by looking at the drug’s generic name. If you see “-tinib,” you know it’s a tyrosine kinase inhibitor, likely used for cancer. “-gliflozin” means it’s an SGLT2 inhibitor, used for diabetes. This system is powerful for researchers and specialists. It helps predict side effects and drug interactions. But it’s not practical for a busy family doctor. You don’t need to know a drug inhibits a specific kinase to know it helps control blood sugar. That’s why pharmacological classification is more common in clinical trials, pharmacy schools, and drug development labs.DEA Scheduling: Legal Status and Abuse Potential
This is the only classification system with legal teeth. Created under the Controlled Substances Act of 1970, the DEA (Drug Enforcement Administration) divides drugs into five schedules based on their potential for abuse and accepted medical use. - Schedule I: No medical use, high abuse potential (e.g., heroin, LSD). Not prescribed. - Schedule II: High abuse potential, but medical use (e.g., oxycodone, fentanyl, Adderall). Strict prescriptions, no refills. - Schedule III: Moderate abuse potential, accepted medical use (e.g., ketamine, buprenorphine). Up to 5 refills in 6 months. - Schedule IV: Low abuse potential (e.g., alprazolam, zolpidem). Commonly prescribed. - Schedule V: Very low abuse potential (e.g., cough syrups with small amounts of codeine). The DEA system is critical for pharmacies to track controlled substances and for law enforcement to prevent diversion. But it’s often criticized for being outdated. Marijuana remains Schedule I, even though FDA-approved cannabinoid drugs like dronabinol are Schedule II. And while oxycodone causes more overdose deaths than heroin, it’s still in a lower schedule. In 2023, the U.S. House passed the MORE Act to reschedule marijuana to Schedule III. If it becomes law, it will trigger a cascade of changes across insurance formularies, hospital protocols, and prescription monitoring systems.Insurance Tiers: What You Pay Out of Pocket
This isn’t about science or law-it’s about money. Insurance companies group drugs into tiers to control costs. Most plans use a 5-tier system: - Tier 1: Preferred generics (cheapest, often 75% of all generics) - Tier 2: Non-preferred generics (slightly higher copay) - Tier 3: Preferred brand-name drugs - Tier 4: Non-preferred brand-name drugs - Tier 5: Specialty drugs (expensive, often for cancer or rare diseases) Here’s the catch: two identical generic drugs can be in different tiers. One might be on Tier 1 because your insurer negotiated a lower price with the manufacturer. The other, with the same active ingredient, might be on Tier 2 because the pharmacy benefit manager (PBM) has a different contract. A 2022 KFF analysis found patients pay 25-35% more for Tier 3 generics than Tier 2, even when the drugs are chemically identical. Pharmacists report that 43% of prior authorization requests come from insurance tier disputes-not because the drug doesn’t work, but because it’s not the cheapest option the insurer picked. This system prioritizes cost over clinical need. It’s why you might get a different generic version than your doctor prescribed-because the pharmacy’s contract says so.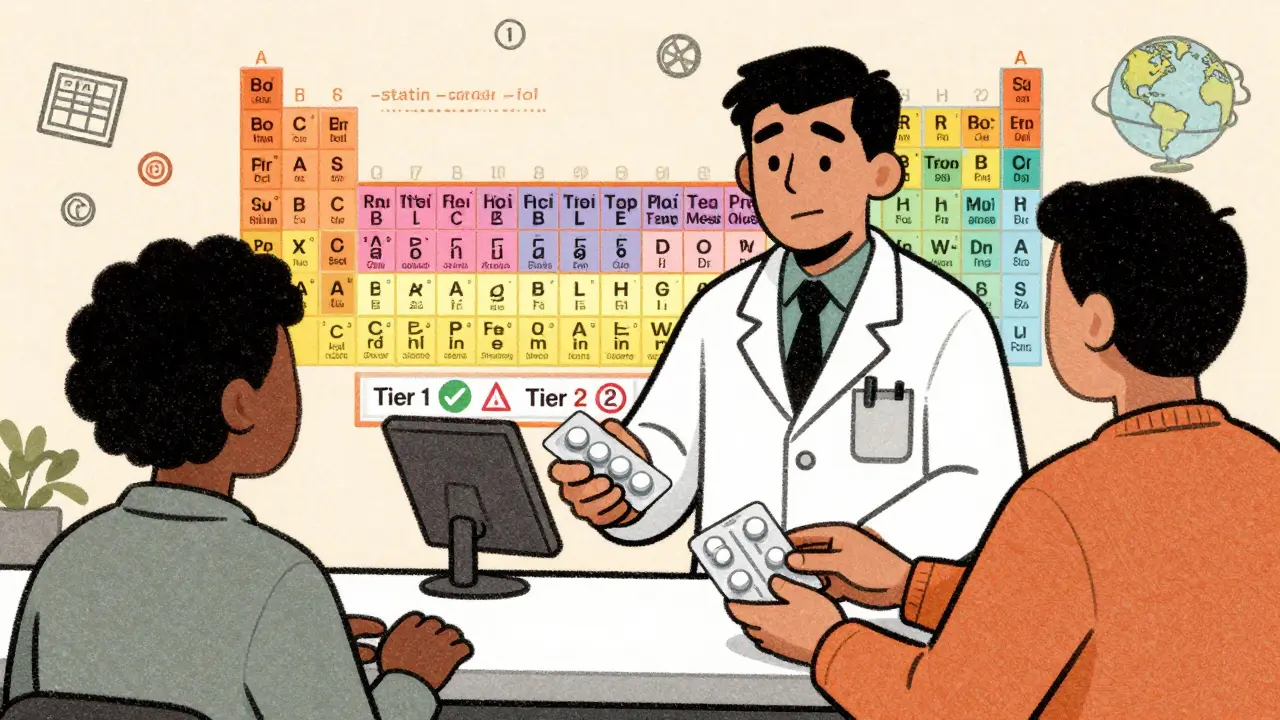
ATC Classification: The Global Standard
If you travel abroad or read international medical research, you’ll see the Anatomical Therapeutic Chemical (ATC) system everywhere. Developed by the World Health Organization, it’s the most comprehensive classification system in the world. The ATC system uses a five-level code: 1. Anatomical group (e.g., A = Alimentary tract and metabolism) 2. Therapeutic subgroup (e.g., A10 = Drugs used in diabetes) 3. Pharmacological subgroup (e.g., A10B = Blood glucose lowering drugs, excluding insulins) 4. Chemical subgroup (e.g., A10BA = Biguanides) 5. Chemical substance (e.g., A10BA02 = Metformin) As of 2023, the ATC system includes over 5,000 drugs across 14 main anatomical groups. It’s used in 143 countries and is the backbone of global drug use studies. The WHO adds 200+ new codes each year to keep up with new drugs. Unlike U.S.-focused systems, ATC doesn’t care about insurance tiers or DEA schedules. It’s purely scientific. That’s why it’s the gold standard for research, public health reporting, and global drug safety monitoring.Why This Matters to You
You might think classifications are just for bureaucrats. But they directly affect your care. - A doctor who confuses therapeutic and pharmacological classes might prescribe a drug that interacts badly with your other meds. - An insurance tier change could mean your $5 generic suddenly costs $30. - A DEA schedule change could make a drug harder to refill. - A new ATC code might mean your cancer drug gets covered under a new policy. Healthcare professionals spend 12-18 minutes per patient just navigating these conflicting systems. Nurses report faster, safer medication checks when classification is consistent. Pharmacists say tier disputes are the #1 reason for delays in filling prescriptions. The good news? Systems are improving. The FDA’s new 2.0 model will handle multi-use drugs better. AI tools like IBM Watson’s Drug Insight platform are learning to predict the best classification with 92% accuracy. And more doctors are using stem names to avoid errors. Understanding these systems doesn’t make you a pharmacist. But it helps you ask better questions: Why is this the preferred generic? Why is my drug in Tier 2? Is this the same as the one I took last year? When you know how drugs are grouped, you’re not just a patient-you’re a partner in your care.What’s Next for Drug Classification?
The future of drug classification is moving fast. As personalized medicine grows, drugs are being designed to work on multiple pathways at once. A single pill might treat depression, chronic pain, and inflammation. Traditional systems can’t handle that easily. Experts predict that by 2028, 65% of new drugs will need hybrid classification systems that combine therapeutic use, pharmacological action, and even genetic markers. Academic centers are already testing models that link drug response to DNA variants. Meanwhile, regulatory pressure is mounting. The 21st Century Cures Act requires standardized therapeutic classification in all electronic health records by 2025. Hospitals are spending $120,000-$200,000 to update their systems. One thing is clear: classification systems aren’t going away. They’re evolving. And if you want to understand your medications, you’ll need to understand how they’re organized.
How to Use This Knowledge
You don’t need to memorize all 300 therapeutic categories. But here’s how to use this info in real life:- When your doctor prescribes a generic, ask: “Is this the preferred generic on my insurance plan?”
- If your copay jumps unexpectedly, check if the drug moved tiers. Call your insurer.
- Look at the generic name. Does it end in “-prazole,” “-lol,” or “-statin”? That tells you its class and likely use.
- If you’re on a controlled substance, know your DEA schedule. Schedule II drugs can’t be refilled; Schedule IV can.
- When switching pharmacies, ask if they carry the same generic version. Sometimes, it’s the same drug, just a different manufacturer.
Common Confusions and How to Avoid Them
Many patients and even some providers mix up these systems. Here are the top 3 misunderstandings:- “If it’s generic, it’s always cheaper.” Not true. Two identical generics can be in different insurance tiers. Always check your plan’s formulary.
- “Schedule I means it’s dangerous.” Not exactly. Schedule I means the government says it has no medical use-despite growing evidence. That’s a legal label, not a medical one.
- “The brand name is better than the generic.” By law, generics must be bioequivalent. They work the same. The difference is usually just in the filler ingredients or packaging.
Resources to Learn More
If you want to dig deeper:- Check your insurer’s formulary online (they list drug tiers and preferred generics).
- Use the FDA’s Drug Shortage Database to see if your generic is affected.
- Search the WHO’s ATC index to see how your drug is classified globally.
- Download the DEA’s Controlled Substance Index for legal status updates.
What’s the difference between therapeutic and pharmacological classification?
Therapeutic classification groups drugs by the medical condition they treat-like blood pressure or diabetes. Pharmacological classification groups them by how they work in the body-like blocking receptors or inhibiting enzymes. One tells you what the drug does; the other tells you how it does it.
Why are two identical generic drugs in different insurance tiers?
Insurance companies negotiate prices with drug manufacturers. Even if two generics have the same active ingredient, one might be cheaper because the insurer struck a better deal with that maker. The drug in the lower tier gets preferred status, even if it’s chemically identical.
Does the DEA schedule affect whether a drug is covered by insurance?
Not directly. Insurance coverage depends on formulary tiers, not DEA schedules. But if a drug is Schedule II, insurers may require extra documentation or limit refills, which can delay access. Some plans won’t cover Schedule I drugs at all because they’re illegal.
How do drug names tell you what class they’re in?
Generic names often end in standardized suffixes called stems. For example, drugs ending in “-lol” are beta-blockers (like metoprolol), “-prazole” are proton pump inhibitors (like omeprazole), and “-statin” are cholesterol-lowering drugs (like atorvastatin). These stems help doctors and pharmacists quickly identify a drug’s class.
Is the ATC system used in the U.S.?
Yes, but not as the primary system. U.S. hospitals and pharmacies mainly use the FDA’s USP Therapeutic Categories. But the ATC system is used globally and is the standard in research, international drug databases, and public health reporting. Many U.S. drug information tools include ATC codes alongside local classifications.





12 comments
Sheila Garfield
I never realized how much paperwork goes into something as simple as picking up a pill. My grandma used to say 'if it works, don't question it' but now I get why she'd get confused when her meds changed without warning.
Shawn Peck
Bro this is just corporate BS dressed up as science. Insurance tiers? DEA schedules? Who cares. If it lowers my blood pressure and doesn't kill me, that's all I need to know.
Kelly Weinhold
This actually made me feel way more in control of my own health. I used to just take whatever the pharmacy gave me but now I ask about tiers and stems. Last week I asked why my metformin was $3 more and they switched me to the same drug in Tier 1. Felt like a boss.
April Allen
The real issue isn't classification systems-they're necessary tools. It's that they're fragmented, contradictory, and weaponized by profit-driven entities. Therapeutic categories prioritize clinical logic. ATC is global and coherent. DEA is political. Insurance tiers are financial warfare. And we're expected to navigate this maze while sick, scared, or in pain. No wonder people distrust healthcare. It's not the science-it's the architecture of exploitation.
Jason Xin
I work in pharmacy and let me tell you-tier disputes are the #1 reason prescriptions sit unfulfilled for days. A patient gets prescribed lisinopril. We have two generics. One’s Tier 1, one’s Tier 3. The patient doesn’t care. The doctor doesn’t care. But the PBM? They care a lot. So we call. We wait. We argue. And the patient walks out frustrated. Not because the drug doesn’t work. Because the system does.
calanha nevin
The ATC system is the only one that makes sense globally. Why does the US cling to outdated bureaucratic frameworks when a standardized scientific model exists? The answer is simple: money. Standardization reduces profit margins for PBMs and insurers. The system is designed to confuse you so you don’t ask why your $5 drug suddenly costs $30.
Lisa McCluskey
I’ve been on 7 different generics for my thyroid over the past 5 years. All the same active ingredient. All labeled identical. But my heart races on one and I’m sluggish on another. Turns out fillers matter more than we’re told. The system says they’re interchangeable. My body says otherwise. Always ask for the brand if you feel off. It’s not paranoia. It’s physiology.
Diana Dougan
So let me get this straight. A drug that cures cancer is Schedule II but weed that helps with chemo nausea is Schedule I? And we wonder why people don’t trust the FDA? This is a joke. I’m not even mad. I’m just disappointed we still live in 1970.
Rohit Kumar
In India we use ATC as our primary system. It’s not perfect but at least it’s consistent. Here in the US I’ve seen doctors prescribe a drug based on insurance tier not clinical need. That’s not medicine. That’s supply chain management with a stethoscope. We need to fix the system not just explain it.
Jodi Olson
The real tragedy is that patients internalize the chaos. If your copay jumps you assume the drug stopped working. If your refill is denied you assume the doctor made a mistake. The system doesn’t just complicate care-it erodes trust. And trust is the foundation of healing.
Marc Bains
I teach med students and I always tell them: learn the stems. If you know -prazole, -sartan, -vastatin you can guess 70% of what a drug does before you even look it up. It’s not magic. It’s just smart design. The problem is most of them are too busy memorizing brand names to care. We’re training doctors to be pharmacists' assistants not clinicians.
Kimberly Reker
I used to think all generics were the same until my anxiety meds changed and I felt like I was drowning. Turned out the filler was different. I asked my pharmacist if they could get me the old one. She said sure but it’s Tier 2 so $15 more. I paid it. My mental health isn’t negotiable. This system is broken but knowing how it works lets you fight back.