When you’re struggling to breathe, it’s hard to tell if it’s asthma or COPD. Both make your chest tight, leave you wheezing, and force you to stop mid-sentence to catch your breath. But they’re not the same condition - and treating them the same way can make things worse.
What’s Really Happening in Your Lungs?
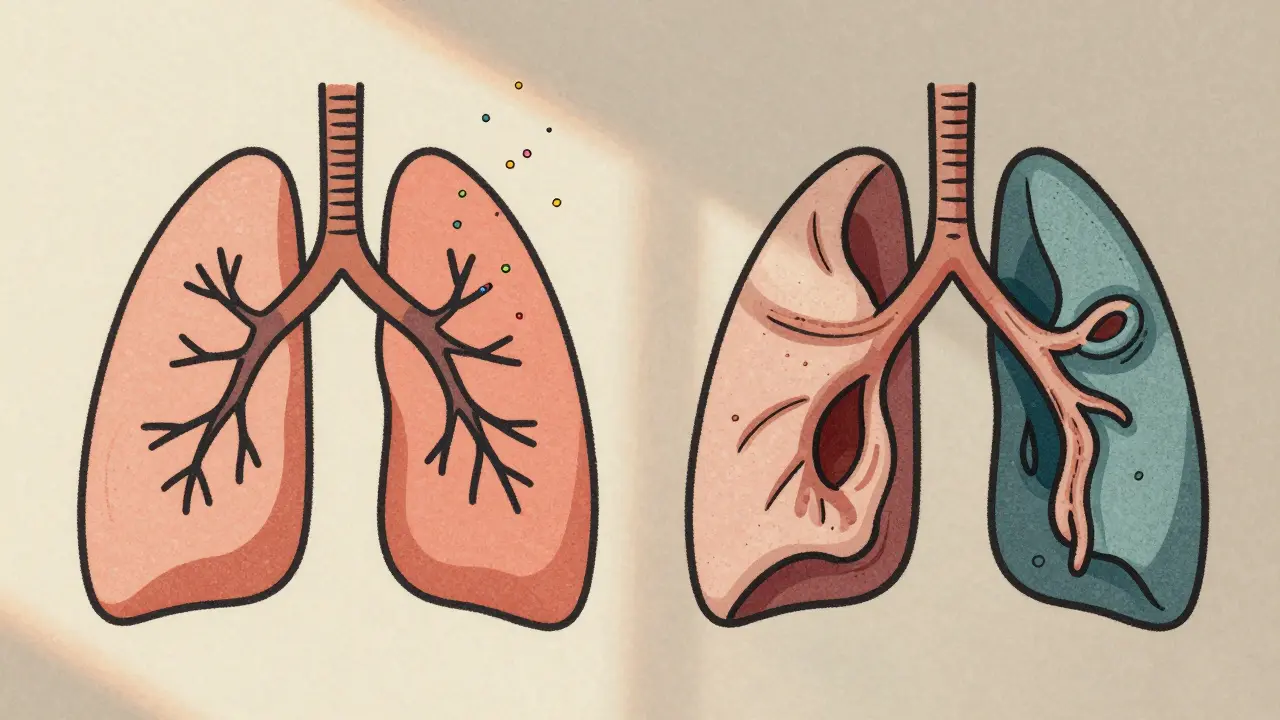
Asthma is an inflammatory condition where your airways react strongly to triggers like pollen, cold air, or exercise. These reactions cause swelling, mucus buildup, and muscle tightening around the airways - but the good news is, this narrowing is usually reversible. Between flare-ups, many people with asthma feel completely normal.
COPD, on the other hand, is a group of diseases - mainly emphysema and chronic bronchitis - that cause permanent damage to the lungs. The air sacs lose elasticity, the airways get scarred and thickened, and mucus clogs them up. This damage doesn’t heal. Even with treatment, your lungs won’t return to how they were before.
The biggest difference? Asthma is often reversible. COPD is progressive and mostly irreversible.
Symptoms: When Do You Feel It?
If your symptoms come and go - especially at night or early morning - it’s more likely asthma. You might wake up gasping, or feel tightness after running or being around pets. You might cough, but it’s often dry. Many asthma patients go weeks or months without any symptoms at all.
COPD symptoms are different. They stick around. You’ll likely have a daily cough that brings up phlegm - sometimes thick and yellow or green. You’ll feel out of breath walking up stairs, even if you’ve never been athletic. And unlike asthma, you won’t have clear breaks between flare-ups. Even on “good” days, you’re still working harder to breathe.
Another clue: cyanosis. If your lips or fingernails turn blue, it’s a sign your body isn’t getting enough oxygen. That’s common in advanced COPD, but almost never seen in asthma.
Who Gets It? Age and Risk Factors
Asthma often starts in childhood. Half of all cases are diagnosed before age 10. Many kids outgrow it, but others carry it into adulthood. Genetics play a big role - if your parents have asthma or allergies, your risk goes up. Allergic rhinitis (hay fever) and eczema often come with asthma.
COPD almost always shows up after age 40. Nine out of ten cases are linked to smoking. Long-term exposure to secondhand smoke, air pollution, or chemical fumes can also cause it. Unlike asthma, COPD rarely appears in people under 40 - unless they’ve had serious lung damage from childhood illness or genetic conditions like alpha-1 antitrypsin deficiency.

How Doctors Tell Them Apart
There’s no single test that gives you a yes-or-no answer, but doctors use a few key tools:
- Spirometry: This measures how much air you can blow out and how fast. In asthma, your lung function improves by 12% or more after using a rescue inhaler. In COPD, the improvement is usually less than 12% - because the damage is structural, not just inflamed.
- FeNO test: This measures nitric oxide in your breath. High levels (above 50 ppb) point to eosinophilic inflammation - the kind seen in asthma. COPD patients usually have levels below 25 ppb.
- Blood eosinophil count: If your blood shows more than 300 cells/μL, it suggests asthma or overlap syndrome. Below 100, it’s more likely pure COPD.
- CT scan: Shows emphysema - destroyed air sacs - in 75% of COPD patients. In asthma, you’ll rarely see that kind of damage.
Doctors also look at your history. Do you have allergies? Did you smoke for 20+ years? Do you cough up mucus every morning? These clues help piece together the puzzle.
Treatment: One Size Doesn’t Fit Both
Asthma treatment is built around controlling inflammation and quickly reversing airway narrowing.
- Quick relief: Short-acting beta-agonists (like albuterol) open airways within minutes.
- Long-term control: Inhaled corticosteroids reduce swelling and prevent flare-ups.
- Severe cases: Biologics like omalizumab or mepolizumab target specific immune cells (eosinophils) and can cut attacks by half.
For COPD, the goal is to manage symptoms and slow decline - because you can’t reverse the damage.
- First-line: Long-acting bronchodilators (LABAs and LAMAs) relax airway muscles and make breathing easier all day.
- Only if you have frequent flare-ups: Inhaled steroids are added - but they’re not first choice because they don’t fix the core problem and can increase infection risk.
- Smoking cessation: This is the single most effective treatment. Quitting cuts disease progression by 50%.
- Pulmonary rehab: A structured program with exercise, breathing techniques, and education improves daily function. COPD patients gain about 54 meters in walking distance after rehab - asthma patients barely move the needle.
Here’s the kicker: 89% of asthma patients achieve good control with proper treatment. Only 52% of COPD patients do. Why? Because asthma responds well to medication. COPD doesn’t - it’s about managing damage, not curing it.
What About Asthma-COPD Overlap (ACOS)?
Up to 25% of people with obstructive lung disease have features of both. This is called ACOS. These patients often have a history of asthma and smoking. They get more flare-ups than people with just asthma or just COPD. Their symptoms are worse, and they end up in the ER more often.
ACOS patients usually have:
- Eosinophil counts like asthma (above 300 cells/μL)
- Fixed airflow limitation like COPD (less than 12% reversibility on spirometry)
Treatment for ACOS is a mix: bronchodilators plus inhaled steroids, sometimes even triple therapy (LABA + LAMA + ICS). But evidence is still evolving - and misdiagnosing ACOS as pure asthma or pure COPD can lead to under-treatment.
Prognosis: What’s the Long-Term Outlook?
Asthma has a much better survival rate. The 10-year survival for moderate asthma is 92%. For moderate COPD, it’s 78%. That’s a big gap.
But here’s something surprising: long-term asthma (over 20 years) can lead to permanent airflow limitation in 15-20% of people. That’s why some older adults with lifelong asthma end up looking like they have COPD. It’s not the same disease - but the lungs can change over time.
Smoking changes everything. If you have asthma and smoke, your risk of developing COPD jumps. If you have COPD and keep smoking, you’ll decline faster. Quitting is the best thing you can do - no matter which diagnosis you have.
Can You Have Both?
Yes. And if you do, you’re in the ACOS group. But many people are misdiagnosed - especially over 40. A 2023 study found that 25% of people with respiratory symptoms got the wrong diagnosis at first. That’s why accurate testing matters.
If you’ve been told you have asthma but your inhaler doesn’t help much, or you’ve been told you have COPD but you’ve never smoked - get a second opinion. Ask for spirometry with reversibility testing, FeNO, and blood eosinophil counts. Don’t accept a label without evidence.
Bottom Line: Know Your Lungs
Asthma and COPD both affect your breathing - but they’re not interchangeable. Asthma is often triggered, reversible, and starts young. COPD is persistent, progressive, and tied to long-term smoke exposure.
Treatment is different. So is outlook. And if you’re unsure, don’t guess. Get tested. Ask questions. Your lungs are counting on it.







8 comments
swarnima singh
i swear i thought i had asthma til i started coughing up green stuff every morning... turns out i smoked for 15 years and now my lungs are just... done. no magic inhaler fixes this. why do people act like it's all the same?
Isabella Reid
This is such a clear breakdown. I work in primary care and see so many patients misdiagnosed because doctors skip spirometry. The FeNO test alone could save so many people from unnecessary steroids. Seriously, if you're over 40 and have breathing issues - get tested properly. It's not just about labels, it's about survival.
waneta rozwan
OMG. I just read this and I'm crying. 😭 My mom had COPD and they kept giving her asthma meds for YEARS. She was 52 when she finally got the right diagnosis. By then? The damage was done. And now I'm terrified I'll end up like her. I don't even smoke anymore but I still feel like I'm breathing through a straw sometimes. Why is this so poorly understood?
Cheryl Griffith
I used to think asthma was just 'bad allergies' until my brother had a near-fatal attack at 19. He’s 34 now and still uses his inhaler daily. But my uncle? He’s 67, smoked since 15, and his lungs are basically Swiss cheese. Two different worlds. The fact that ACOS exists makes me wonder how many of us are just... stuck in the middle, getting half the help we need.
Allen Davidson
If you're reading this and you're still smoking - stop. Not tomorrow. Not next week. Today. Even if you've had COPD for 10 years, quitting now gives you back 50% of your decline rate. That's not a miracle. That's math. And your future self will thank you.
Stephen Tulloch
LMAO at people who think inhalers are just 'magic breath candy'. 😂 I got my spirometry done last year - turned out I had ACOS. My doctor was like 'oh you're basically asthma but with a side of ruined lungs'. I'm on triple therapy now and honestly? I feel like I'm finally breathing again. No more pretending I'm fine.
Joie Cregin
I used to be the person who said 'just breathe deeper' to someone wheezing. I was so clueless. Now my best friend has asthma and I carry her rescue inhaler in my purse like it's a spare key. And my dad? COPD. He walks slower now. I don't say 'you're fine' anymore. I just hold the door open a little longer. These diseases don't care how tough you are. They just take.
Melodie Lesesne
My sister was diagnosed with asthma at 7. I was diagnosed with COPD at 48 - after 20 years of secondhand smoke at work. We both use inhalers. But hers works like a charm. Mine? Just slows the fall. I wish people knew how different they really are. It’s not just 'lung problems'. It’s two different battles.