Statin Efficacy: How These Cholesterol Drugs Really Work and Who Benefits Most
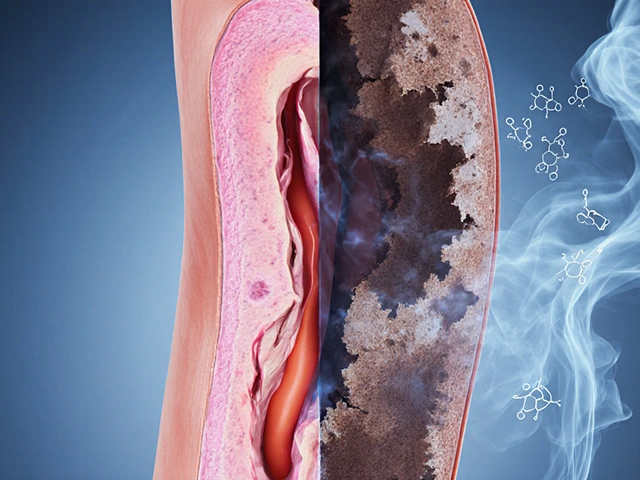
When it comes to lowering cholesterol, statins, a class of prescription drugs that block cholesterol production in the liver. Also known as HMG-CoA reductase inhibitors, they’re among the most prescribed medications worldwide because they don’t just move numbers on a lab report—they cut heart attacks and strokes in half for many people. But not all statins are the same, and not everyone responds the same way. Some see their LDL (bad cholesterol) drop by 50% in weeks. Others feel muscle pain and wonder if the trade-off is worth it.
The real question isn’t just whether statins work—it’s how well they work for you. LDL reduction, the primary measure of statin effectiveness varies by drug type and dose. Rosuvastatin and atorvastatin are the heavy hitters, often dropping LDL by 45–60%. Simvastatin and pravastatin? More modest, around 20–40%. But effectiveness isn’t just about numbers. cardiovascular risk, the chance of having a heart attack or stroke over the next 10 years is what matters most. Studies show that for every 40 mg/dL drop in LDL, cardiovascular events fall by about 20–25%. That’s not theoretical—it’s seen in real patients, including those with diabetes, high blood pressure, or a family history of early heart disease.
Side effects are where things get messy. Muscle aches are the most common complaint, but true muscle damage (rhabdomyolysis) is rare—less than 1 in 10,000. More often, people stop statins because they feel tired, or they blame the drug for symptoms that started years before. statin side effects, including liver enzyme changes and increased blood sugar in some are usually mild and manageable. But they’re real enough that doctors now check in regularly—not just to see if cholesterol dropped, but if you’re still taking the pill. And here’s the twist: if you’re at high risk for heart disease, skipping statins because of fear often does more harm than the drug itself.
Some people try to replace statins with supplements like red yeast rice or plant sterols. But those aren’t replacements—they’re weak imitations. Red yeast rice contains a natural form of lovastatin, but without the safety testing or dosage control. Plant sterols? They might lower LDL by 5–10%, but they don’t cut heart attacks like statins do. And don’t forget: herbal teas, like green tea or grapefruit juice, can interfere with how your body breaks down statins, making side effects worse or the drug less effective.
So who benefits most? People with existing heart disease, type 2 diabetes, very high LDL, or a strong family history. But even healthy people with moderate risk can see big gains—especially if they’re over 50 and have other risk factors. It’s not about being perfect. It’s about staying protected. The posts below dig into real cases: how statins interact with other meds, why some people feel better after switching brands, what labs to track, and how to tell if your body is responding—or pushing back. You’ll find no fluff, no marketing. Just what works, what doesn’t, and what to ask your doctor next time you’re handed a prescription.

- Nov 21, 2025
- Posted by Cillian Osterfield
Night vs Morning Statin Dosing: What Really Matters for Side Effects and Effectiveness
Does taking your statin at night or morning make a difference? For most people today, the answer is no. What matters more is sticking to your schedule every day.
Categories
- Health and Wellness (72)
- Medications (72)
- Health and Medicine (28)
- Pharmacy Services (12)
- Mental Health (9)
- Health and Career (2)
- Medical Research (2)
- Business and Finance (2)
- Health Information (2)
©2026 heydoctor.su. All rights reserved