Obesity Treatment: What Actually Works and What to Avoid
When we talk about obesity treatment, a medical approach to managing excessive body fat that reduces health risks. Also known as weight management therapy, it’s not just about losing pounds—it’s about fixing how your body stores energy, responds to food, and handles hormones. Too many people think it’s simply a matter of eating less and moving more. But that’s like trying to fix a leaky pipe by mopping the floor. The real problem is deeper—and so are the solutions.
Weight loss medications, prescription drugs that help reduce appetite or slow fat absorption like semaglutide and tirzepatide have changed the game. They don’t magic away fat, but they help your brain stop screaming for food when you’re already full. These aren’t quick fixes—they’re tools for people who’ve tried everything else and still struggle with hunger signals that won’t shut off. Then there’s bariatric surgery, procedures like gastric bypass or sleeve gastrectomy that physically change how your stomach and intestines work. It’s not for everyone, but for those with severe obesity and related conditions like type 2 diabetes, it’s often the only thing that leads to lasting results. Studies show people who get surgery lose 20–30% of their body weight and keep it off longer than with diet alone.
But here’s what most guides skip: lifestyle changes, daily habits like sleep, stress management, and meal timing that affect metabolism are the foundation—even if you’re on meds or considering surgery. You can’t out-drug a 3 a.m. snack habit or chronic stress. Sleep loss raises ghrelin, the hunger hormone. Stress spikes cortisol, which stores fat around your belly. And skipping meals? That slows your metabolism down for hours. These aren’t side notes—they’re the engine.
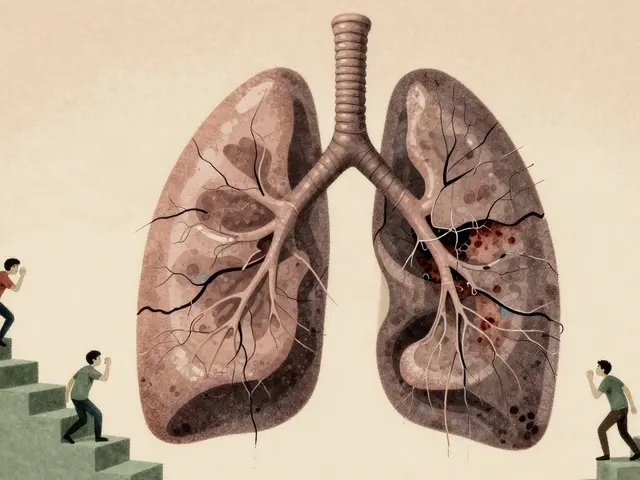
And let’s talk about metabolic health, how well your body processes sugar, fat, and energy. Someone can be overweight and metabolically healthy—or thin and dangerously insulin resistant. That’s why doctors now look at blood pressure, triglycerides, and fasting glucose—not just BMI. If your liver is fatty or your insulin is high, no amount of treadmill running will fix it without targeting the root cause.
What you won’t find in this collection are miracle teas, detox cleanses, or apps that promise 20 pounds in 2 weeks. What you will find are real stories and science-backed guides: how to read your prescription labels if you’re on weight-loss meds, what to expect before and after bariatric surgery, how sleep and stress quietly sabotage your efforts, and why some people gain weight even when they eat salads. These aren’t theoretical—they’re from people who’ve been there, and from doctors who’ve seen what actually works in the real world.
If you’re tired of being told to just "try harder," you’re in the right place. This isn’t about willpower. It’s about understanding your body, choosing the right tools, and avoiding the traps that make obesity treatment feel impossible. Below, you’ll find practical advice that matches the complexity of your situation—not a one-size-fits-all checklist.

- Dec 1, 2025
- Posted by Cillian Osterfield
Obesity Comorbidities: How Diabetes, Heart Disease, and Sleep Apnea Connect and What to Do About It
Obesity doesn't just mean extra weight-it triggers diabetes, heart disease, and sleep apnea in a dangerous cycle. Learn how these conditions connect, why treating one helps the others, and what actually works to break the pattern.
Categories
- Health and Wellness (72)
- Medications (69)
- Health and Medicine (28)
- Pharmacy Services (12)
- Mental Health (9)
- Health and Career (2)
- Medical Research (2)
- Business and Finance (2)
- Health Information (2)
©2026 heydoctor.su. All rights reserved