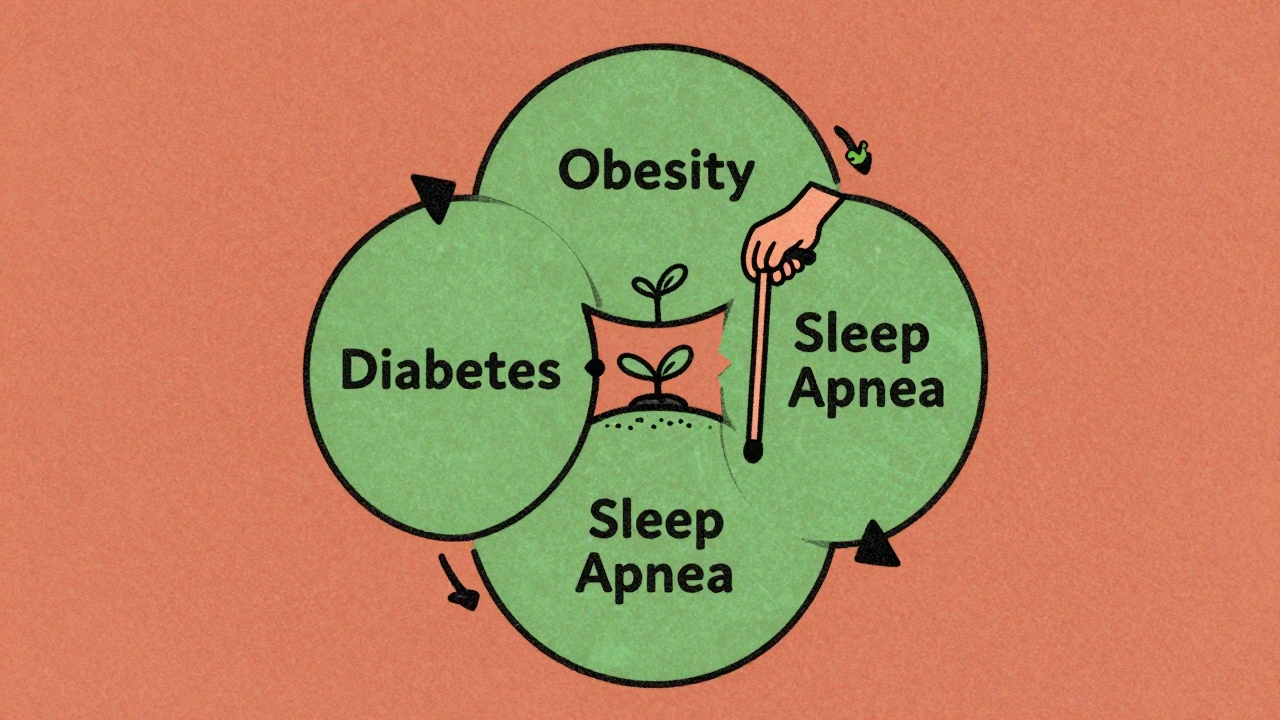
When you hear the word obesity, most people think of weight alone. But for millions, it’s not just about the number on the scale-it’s about what that extra weight is doing to your body behind the scenes. Obesity doesn’t just change how you look. It rewires your metabolism, strains your heart, disrupts your sleep, and sets the stage for serious, life-threatening conditions. Three of the most common and dangerous companions of obesity are type 2 diabetes, heart disease, and obstructive sleep apnea. Together, they form a dangerous trio that feeds off each other, making each condition worse than if they appeared alone.
The Hidden Web: How Obesity Triggers Diabetes, Heart Disease, and Sleep Apnea
Obesity isn’t just a symptom-it’s the root. When fat builds up, especially around the belly, it doesn’t just sit there. It becomes active, releasing inflammatory chemicals that spread through the bloodstream. These chemicals mess with how your body uses insulin, clog arteries, and narrow your airways. That’s why someone with obesity is far more likely to develop diabetes, heart disease, and sleep apnea-not because they’re lazy or eating too much, but because their body’s biology has changed.
Take type 2 diabetes. In a person with normal weight, insulin works like a key that unlocks cells so sugar can enter and be used for energy. In obesity, those cell locks get gummed up. Fat tissue produces substances that block insulin’s action. The result? Blood sugar climbs. By the time someone is diagnosed with diabetes, they’ve often had insulin resistance for years. Studies show obese individuals have 30-50% higher levels of inflammation markers like C-reactive protein, which directly interfere with insulin signaling.
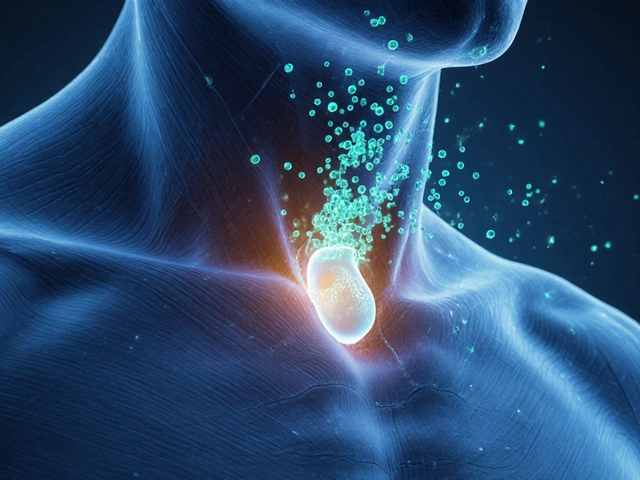
Now add sleep apnea. When you sleep, your throat muscles relax. In someone with obesity, extra fat around the neck and tongue pushes down on the airway. The result? Breathing stops for 10 seconds or more, dozens of times a night. Each pause drops oxygen levels, triggering stress responses that spike blood pressure and release adrenaline. Over time, this pattern damages blood vessels and increases insulin resistance even further. The Sleep Heart Health Study found that people with severe sleep apnea (more than 30 breathing pauses per hour) have a 60% higher risk of developing diabetes-even after accounting for their weight.
And then there’s heart disease. Obesity makes the heart work harder. The heart muscle thickens, blood pressure rises, and cholesterol levels shift toward harmful types. Sleep apnea adds another layer: each time breathing stops, blood pressure surges by 15-25 mmHg. These nightly spikes wear down artery walls. Meanwhile, diabetes accelerates plaque buildup in those same arteries. The combination? A 3.2-fold higher risk of heart attack compared to someone with normal weight and none of these conditions.
The Vicious Cycle: How One Condition Makes the Others Worse
This isn’t just a list of three separate problems. It’s a cycle. Each condition makes the others stronger, and the cycle keeps spinning.
Obesity → Sleep Apnea: Every extra kilogram of body weight increases sleep apnea risk by 14%. Waist size matters even more than overall weight. For every centimeter your waist grows, your chance of sleep apnea rises by 12%. That’s because belly fat pushes up on the diaphragm, making it harder to breathe deeply-even when awake.
Sleep Apnea → Diabetes: When you stop breathing at night, your body goes into survival mode. Stress hormones flood your system, telling your liver to pump out more sugar. Your muscles become resistant to insulin. A 2021 study showed that obese people with untreated sleep apnea had 25-30% worse insulin resistance than those without it. That’s why many people with diabetes don’t improve with diet and pills alone-they need to fix their sleep first.
Diabetes → Sleep Apnea: High blood sugar damages nerves, including those that control throat muscles. Weak muscles collapse more easily during sleep, making apnea worse. It’s not just fat causing the problem-it’s nerve damage too.
Sleep Apnea → Heart Disease: The repeated drops in oxygen and spikes in blood pressure lead to irregular heart rhythms. Severe sleep apnea increases the risk of atrial fibrillation (AFib) by 2-5 times. And because AFib raises stroke risk, it’s no surprise that people with obesity, diabetes, and sleep apnea have the highest rates of heart failure.
And here’s the kicker: heart disease makes it harder to lose weight. Fatigue from poor sleep and heart strain reduces physical activity. Medications for diabetes and high blood pressure can cause water retention or increased appetite. The cycle tightens.
Who’s at Risk? The Real Numbers Behind the Triad
The numbers don’t lie. In the U.S., 42.4% of adults have obesity. Of those, 86% with type 2 diabetes also have sleep apnea. And nearly half of all people with sleep apnea have diabetes or high blood pressure.
But it’s not just about BMI. Someone with a BMI of 32 and a waist size of 102 cm has a higher risk of sleep apnea than someone with a BMI of 35 but a waist of 90 cm. Abdominal fat is the real culprit. That’s why doctors now look at waist circumference as closely as BMI.
Women with obesity are less likely to be diagnosed with sleep apnea than men, even when symptoms are the same. They’re more often told they’re just “tired” or “stressed.” A 2022 survey found that 68% of obese women with diabetes waited 5-7 years before being tested for sleep apnea. By then, the damage was already done.
And the economic toll? People with all three conditions pay $12,300 more per year in medical bills than those with obesity alone. Most of that comes from hospital visits for heart attacks, strokes, and complications from uncontrolled diabetes.
What Actually Works? Breaking the Cycle
The good news? This cycle can be broken. And it doesn’t always require surgery or expensive drugs.
Weight loss is the most powerful tool. Losing just 10% of your body weight can cut sleep apnea severity by half. A study in the Diabetes Care journal found that obese patients with diabetes who lost 10-15% of their weight saw their AHI (apnea-hypopnea index) drop from 40 to under 20 events per hour. That’s the difference between severe and mild sleep apnea.
But how do you lose that weight when you’re tired from poor sleep and your blood sugar is all over the place? The answer is structure.
Start with sleep. If you snore loudly, wake up gasping, or feel exhausted even after 8 hours in bed, get tested for sleep apnea. The STOP-Bang questionnaire-a simple 8-question tool used by doctors-can screen you in under a minute. If your score is 3 or higher, you need a sleep study.
If you’re diagnosed with sleep apnea, CPAP therapy is the gold standard. It’s not perfect-many people find the mask uncomfortable, and 55% quit within a year. But for those who stick with it, the results are dramatic. A 2023 study showed consistent CPAP use reduced HbA1c (a measure of long-term blood sugar) by 0.8% on average. That’s the same drop you’d get from adding a second diabetes medication.
And then there’s medication. New GLP-1 drugs like semaglutide don’t just help you lose weight-they directly reduce fat in your airway. In the 2024 LEADER-OSA trial, people using semaglutide lost nearly 15% of their body weight and saw their sleep apnea improve even before they lost much weight. That’s because the drug reduces fat deposits around the throat.
Bariatric surgery is another option. For people with severe obesity and diabetes, gastric bypass leads to remission of sleep apnea in 78% of cases within a year. The 30-day risk of death is less than 0.3%. For many, it’s life-saving.
What Doctors Are Starting to Do Differently
Five years ago, a doctor might treat your diabetes with pills, your high blood pressure with another pill, and your snoring as a nuisance. Today, guidelines from the American Diabetes Association and the American Heart Association say the same thing: Screen for sleep apnea in every obese person with diabetes.
Hospitals like Kaiser Permanente are now using integrated care teams. One person tracks your weight, another your blood sugar, a third your sleep study results. Electronic records flag when someone’s AHI is rising or their HbA1c isn’t improving. The goal? Catch the cycle early.
And it’s working. In one program, hospitalizations dropped by 22% and ER visits fell by 18% in the first year. That’s not just better health-it’s lower costs and more life.
What You Can Do Today
You don’t need to wait for a doctor’s appointment to start breaking the cycle.
- If you’re overweight and have diabetes, ask your doctor: “Could I have sleep apnea?” Don’t wait for them to bring it up.
- Measure your waist. If it’s over 88 cm for women or 102 cm for men, you’re at higher risk for all three conditions.
- Track your sleep. Do you wake up with a dry mouth? Do you feel tired even after a full night? These are red flags.
- Start small with movement. A 20-minute walk after dinner improves insulin sensitivity and helps you sleep better.
- If you’re on CPAP and it’s uncomfortable, talk to your sleep clinic. There are 15+ mask types. You just haven’t found the right one yet.
- Ask about GLP-1 medications if you’re struggling to lose weight. They’re not magic, but they change the game.
The biggest mistake people make is thinking they have to fix everything at once. You don’t. Fix your sleep, and your blood sugar gets easier to control. Lower your blood sugar, and your energy improves so you can move more. Move more, and your weight starts to drop. The cycle breaks one step at a time.
Why This Matters More Than Ever
By 2035, the U.S. could save $197 billion a year just by better managing obesity, diabetes, and sleep apnea together. That’s not just a statistic-it’s thousands of people avoiding heart attacks, strokes, and early deaths.
But the real win isn’t money. It’s waking up tired of being tired. It’s walking up stairs without gasping. It’s sleeping through the night without your partner nudging you because you stopped breathing. It’s having energy to play with your kids, go for a hike, or just sit outside without needing a nap.
Obesity isn’t the end of the road. It’s the starting point. And with the right approach, it’s a point you can move past.





10 comments
Fern Marder
This is so real 😭 I’ve been living this cycle for years - diabetes, sleep apnea, and my heart feels like it’s running a marathon just to get up the stairs. I started CPAP last year and my HbA1c dropped 1.2%. Not magic, just… human. 🙏
Saravanan Sathyanandha
In India, we call this ‘desi diabetes’ - but it’s not about rice or ghee alone. It’s the silent suffocation of fat around the organs, the exhaustion that feels like karma. I’ve seen uncles who snore louder than traffic, yet no one tests them. We treat symptoms, not systems. This post? It’s the truth wrapped in science. Thank you.
Girish Padia
People just need to stop eating junk and move their butt. It’s not rocket science. I lost 60 lbs by not eating after 7pm and walking 30 mins a day. No drugs. No masks. Just discipline. Why is this so hard?
Sandi Allen
Wait… so you’re telling me the pharmaceutical industry, the CPAP manufacturers, and the medical-industrial complex are ALL profiting off this ‘cycle’? And they’re pushing GLP-1 drugs like they’re candy? Who funded this study? Who owns the journal? Who controls the sleep clinics? I’ve seen the data - it’s all smoke and mirrors…
Chelsea Moore
MY HUSBAND GOT DIAGNOSED WITH SLEEP APNEA AFTER 12 YEARS OF ‘JUST BEING TIRED’ AND NOW HE’S ON CPAP AND GLP-1 AND I’M CRYING BECAUSE HE’S SLEEPING THROUGH THE NIGHT AND WE’RE HOLDING HANDS AGAIN AND I DIDN’T KNOW HOW MUCH I MISSED THAT… THIS POST MADE ME FEEL SEEN. THANK YOU. I’M TELLING EVERYONE.
John Biesecker
Man… i always thought obesity was just ‘eat less move more’ but this? this is like… your body becomes a broken machine where every part is rusting because of one faulty gear. the fat isn’t just weight, it’s a whole system of sabotage. i get it now. thanks for explaining it like i’m not a doctor 😅
Genesis Rubi
Why do we even let fat people get health care? They made their bed. Now they gotta lie in it. I work 60 hours a week and I’m lean as a rail - why should my taxes pay for their CPAP machines and GLP-1 shots? Just eat a salad and run. Simple.
Doug Hawk
There's a neuroendocrine feedback loop here that's underappreciated - adipose tissue secretes leptin resistance, which dysregulates the hypothalamic-pituitary-adrenal axis, leading to nocturnal sympathetic overdrive, which exacerbates insulin resistance and upper airway collapsibility. The CPAP data is compelling but confounded by compliance bias. We need longitudinal biomarker studies with adipose biopsies to isolate causal pathways.
John Morrow
Let’s be honest - the entire narrative around obesity is a distraction. The real issue is systemic neglect of metabolic health in low-income populations, coupled with aggressive food industry lobbying that has turned high-fructose corn syrup and trans fats into cultural staples. The medical establishment profits from treating the downstream consequences - diabetes, heart disease, apnea - while the root cause remains unaddressed because it’s politically inconvenient. This post is well-researched, but it still avoids the elephant in the room: capitalism doesn’t care if you sleep or not, as long as you keep buying.
Kristen Yates
I’m 58. Diagnosed with diabetes in 2018. Started CPAP in 2021. Lost 22 pounds. I still nap sometimes. But I can play with my grandkids now. No big wins. Just small, quiet ones. That’s enough.