Statin Rechallenge Decision Calculator
Statin Rechallenge Eligibility Assessment
This tool uses the Statin-Associated Muscle Symptom Clinical Index (SAMS-CI) to help determine if you're a good candidate for statin rechallenge. Based on clinical evidence, patients with low scores have a 91% chance of successful rechallenge.
Your Result
/5 points
Stopping statins because of muscle pain is common. But for many, it’s not the statin’s fault-it’s the fear of it. If you’ve had muscle aches after starting a statin and quit, you’re not alone. About 7 to 29% of people stop taking statins because of muscle symptoms. But here’s the twist: in clinical trials, muscle pain happened just as often in people taking sugar pills as those taking statins. That’s not a coincidence. It’s called the nocebo effect-when you expect side effects, your body starts to feel them, even if the drug isn’t causing them.
What Exactly Is Statin-Induced Myopathy?
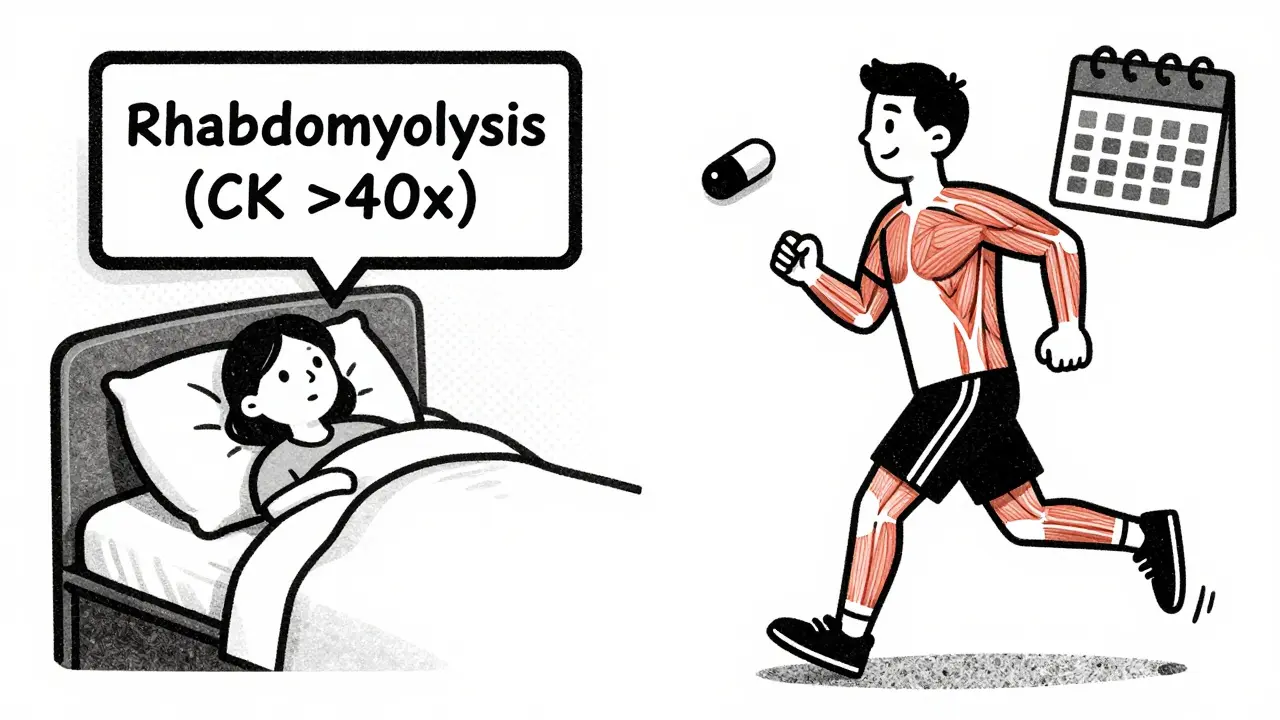
Statin-induced myopathy isn’t one thing. It’s a range of muscle-related issues. On the mild end, you might feel soreness or fatigue-common, but not dangerous. On the serious end, you could develop rhabdomyolysis, where muscle tissue breaks down and leaks into the blood, risking kidney failure. That’s rare-less than 1 in 1,000 people. Most cases are mild and go away when you stop the statin.
The key is knowing what you’re dealing with. If your creatine kinase (CK) levels are only slightly raised, or not raised at all, and your symptoms cleared after stopping the statin, you’re likely a candidate for rechallenge. But if your CK was more than 40 times the normal limit, or if you tested positive for anti-HMGCR antibodies (a sign of immune-mediated muscle damage), then restarting a statin isn’t safe. Those cases need different treatment.
When Can You Try Again?
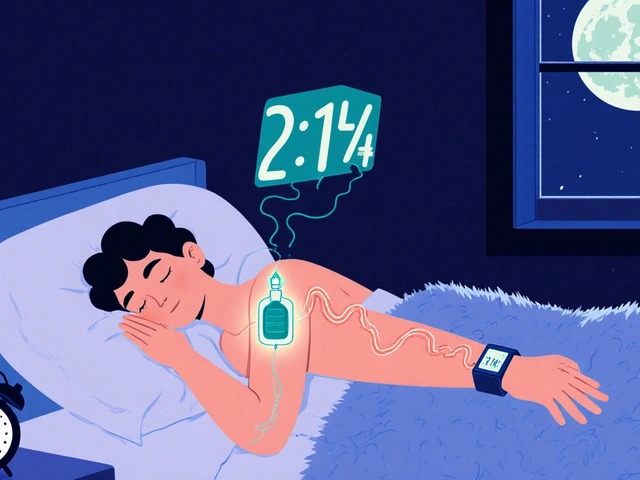
Don’t rush. Wait until symptoms fully disappear. That usually takes 2 to 4 weeks. Some people feel better in days. Others take longer. Your doctor should check your CK levels before you restart. If they’re still high, wait. Also, get your thyroid checked. Low thyroid function can mimic statin side effects.
Timing matters. The longer you’re off statins, the more your cardiovascular risk climbs. Plaques in your arteries can become unstable after just 4 weeks without treatment. That’s why experts say: minimize time off. Don’t wait 6 months just because you’re scared. Two weeks is enough if you’re feeling better.
How to Rechallenge: The MEDS Approach
The International Lipid Expert Panel recommends the MEDS strategy. It’s simple, practical, and backed by data.
- Minimize time off statins: Restart as soon as symptoms are gone, ideally within 2-4 weeks.
- Education: Understand the nocebo effect. Many muscle symptoms aren’t caused by the drug. Knowing this reduces fear.
- Diet and nutraceuticals: Consider coenzyme Q10 (CoQ10), vitamin D, or omega-3s. They don’t cure myopathy, but they may help some people tolerate lower doses.
- Systematic monitoring: Check symptoms and CK levels 2-4 weeks after restarting. If you’re fine, keep going.
This isn’t guesswork. Studies show that using MEDS increases successful rechallenge rates from 30% to over 70%.
Which Statin Should You Try?
Not all statins are the same when it comes to muscle risk. Some are more likely to cause problems than others.
| Statin | Myopathy Risk | Typical Starting Dose |
|---|---|---|
| Pravastatin | Lowest | 10-20 mg daily |
| Fluvastatin | Low | 20-40 mg daily |
| Pitavastatin | Low | 1-2 mg daily |
| Atorvastatin | Moderate | 10-20 mg daily |
| Simvastatin | Higher | 5-10 mg daily |
| Rosuvastatin | Moderate to High | 5-10 mg daily |
Start with the lowest possible dose of the lowest-risk statin. Pravastatin and fluvastatin are your best first bets. Avoid high-dose simvastatin (80 mg) entirely-it’s been linked to higher muscle injury rates.
Dosing Strategies That Work
Once you pick a statin, you don’t have to take it daily. There are proven alternatives:
- Every-other-day dosing: Take the statin every 48 hours instead of every day. This cuts exposure by half but still lowers LDL enough for most people.
- Reduced daily dose: If you were on 40 mg of atorvastatin, try 10 mg. Many patients tolerate this fine.
- Intermittent dosing: For some, taking it twice a week (e.g., Monday and Thursday) works well enough.
One study found that 72% of patients who switched from daily to every-other-day dosing stayed on therapy for over a year without symptoms. The key? Don’t assume you need full daily dosing. Your body can still respond to less.
What If You Still Can’t Tolerate Statins?
If you’ve tried three different statins at low or intermittent doses and still get muscle pain, it’s time to consider alternatives.
- PCSK9 inhibitors (evolocumab, alirocumab): These injectable drugs lower LDL by 50-60%. They’re not cheap-around $5,850 a month-but they work. And if you’re at high risk for heart attack or stroke, they’re worth it.
- Ezetimibe: A pill that blocks cholesterol absorption in the gut. It lowers LDL by 15-20%. Often used with a low-dose statin, but it can be used alone.
- Bile acid sequestrants (like colesevelam): These bind cholesterol in the gut. Less effective, but useful for some.
Here’s the trade-off: statins cost $4-$10 a month. PCSK9 inhibitors cost 500 times more. But if you’re truly intolerant, the cost of a heart attack is far higher.
What the Experts Say
Dr. Paul Ridker, who led the JUPITER trial, points out: in 12 trials with 100,000 patients, muscle symptoms were no more common with statins than with placebo. That means for many, the pain isn’t the drug-it’s the expectation.
Dr. Maciej Banach, who helped create the MEDS approach, says: "The biggest mistake is giving up too soon." He’s seen patients who stopped statins for years, only to restart successfully after learning about the nocebo effect.
Meanwhile, the American Heart Association and American College of Cardiology both agree: if you have high cardiovascular risk, staying off statins is more dangerous than risking muscle pain.
The SAMS-CI Tool: A Game-Changer
There’s a simple clinical tool called the Statin-Associated Muscle Symptom Clinical Index (SAMS-CI). It’s a 5-question checklist that scores your chance of having true statin-induced myopathy.
It looks at:
- Did symptoms start within 6 months of starting the statin?
- Did symptoms go away after stopping?
- Did they return when you restarted?
- Are you over 70?
- Do you have kidney disease or take interacting drugs?
If your score is low, there’s a 91% chance you won’t have symptoms on rechallenge. That’s powerful. Yet, only 43% of primary care doctors use it.
Ask your doctor: "Can we use the SAMS-CI to decide if I’m a good candidate?" If they haven’t heard of it, ask for a referral to a lipid specialist.
Real Stories, Real Results
On health forums, people share their experiences:
- "I stopped simvastatin after muscle pain. My doctor switched me to pravastatin 10 mg every other day. No pain. Two years later, still going strong."
- "I tried three statins. All caused pain. Then I tried ezetimibe + low-dose rosuvastatin. It worked. I didn’t even notice the pain this time."
- "I was told to never restart. But I got a second opinion. We used MEDS. I’m on fluvastatin 20 mg daily now. My cholesterol is normal."
These aren’t outliers. A 2023 survey found 62% of people who tried rechallenge succeeded with a modified plan.
What to Avoid
Some things are dangerous:
- Never restart statins after rhabdomyolysis (CK >40x ULN). That’s a red flag.
- Avoid gemfibrozil with any statin. It increases muscle injury risk by over 10 times.
- Don’t take high-dose simvastatin (80 mg). It’s been pulled in many countries for this reason.
- Don’t ignore thyroid problems. Hypothyroidism can cause muscle pain that mimics statin side effects.
Final Thoughts: Don’t Quit Without a Plan
Statins save lives. They reduce heart attacks, strokes, and death. But they’re not perfect. Muscle pain is real for some. But for many, it’s a false alarm.
If you stopped a statin because of muscle pain, don’t assume you can never take one again. You might just need a different one, a lower dose, or a different schedule. And if you’re at high risk for heart disease, staying off statins could be more dangerous than the pain.
Ask your doctor: Can we try rechallenge? Can we use the SAMS-CI? Can we switch to pravastatin or fluvastatin? Can we try every-other-day dosing?
You don’t have to choose between your heart and your muscles. With the right strategy, you can have both.
Can I restart a statin after stopping because of muscle pain?
Yes, in most cases. If your muscle pain went away after stopping and your CK levels returned to normal, you’re likely a good candidate for rechallenge. Experts recommend waiting 2-4 weeks after symptoms resolve, then restarting with a lower dose or a different statin like pravastatin or fluvastatin. Studies show 60-80% of people can successfully restart with the right approach.
Which statin has the lowest risk of muscle pain?
Pravastatin, fluvastatin, and pitavastatin have the lowest risk of muscle-related side effects. They’re less likely to build up in muscle tissue, which reduces the chance of myopathy. Simvastatin and rosuvastatin carry higher risk, especially at high doses. Starting with pravastatin 10-20 mg daily is often the safest first step for rechallenge.
Is every-other-day dosing effective for statins?
Yes. For many people, taking a statin every other day (or even twice a week) still lowers LDL cholesterol effectively-often by 30-40%, which is enough for most patients. This approach cuts drug exposure in half, reducing muscle side effects. Studies show over 70% of patients who switched to intermittent dosing stayed on therapy for more than a year without symptoms.
What if I still get muscle pain after trying different statins?
If you’ve tried multiple statins at low or intermittent doses and still have pain, you may have true statin intolerance. In that case, non-statin options like ezetimibe or PCSK9 inhibitors (evolocumab, alirocumab) are effective alternatives. These lower LDL by 15-60% and reduce heart attack risk, even without statins. While more expensive, they’re worth considering if your cardiovascular risk is high.
Can supplements like CoQ10 help with statin muscle pain?
CoQ10 and vitamin D are often tried, but evidence they prevent muscle pain is weak. Some people report feeling better, but large studies haven’t confirmed a clear benefit. They’re safe to try, but shouldn’t replace proven strategies like switching statins, lowering the dose, or using intermittent dosing. Don’t rely on supplements alone to solve the problem.
Why do some doctors say not to restart statins at all?
Some doctors avoid rechallenge because they fear liability or haven’t been trained in modern protocols. But guidelines from the American Heart Association and American College of Cardiology clearly support structured rechallenge. If your doctor refuses, ask for a referral to a lipid specialist. Many patients who were told "never again" successfully restarted with the right plan.
What’s the nocebo effect, and how does it relate to statins?
The nocebo effect is when expecting side effects causes you to feel them-even if the drug isn’t responsible. In statin trials, muscle pain occurred just as often in people taking sugar pills as those taking statins. This suggests that fear, misinformation, or media reports can trigger symptoms. Understanding this can help patients feel more confident about rechallenge.
Should I get genetic testing before rechallenging?
Genetic testing for SLCO1B1 variants (like the *5 allele) can help. This gene affects how your body clears statins. People with two copies of the *5 variant have much higher statin levels and are at greater risk for muscle pain. Testing isn’t routine, but if you’ve had repeated myopathy, it’s worth discussing with a lipid specialist. It can guide safer statin choices.
Rechallenge after statin myopathy isn’t about taking risks-it’s about using science to find a path back to protection. You don’t have to choose between your heart and your muscles. With the right strategy, you can have both.






13 comments
Jonathan Noe
I've been on atorvastatin for 5 years and never had an issue until last year. Thought I was getting old, but then I read about the nocebo effect. Started reading more, cut out the fear-mongering YouTube videos, and switched to pravastatin 10mg every other day. No pain. LDL down 38%. Mind blown.
Ernie Simsek
I tried CoQ10 for 3 months. Felt like I was taking magic fairy dust. Still got muscle twitches. Then I switched to fluvastatin 20mg daily. Zero issues. Supplements are for people who don't read studies. 🤡
Jim Johnson
yo i was scared to restart too but my doc used the SAMS-CI tool and said i had a 94% chance of being fine. switched to pitavastatin 1mg every other day. 18 months later and i'm still going. my cardiologist said i'm one of the success stories now. don't let fear win. you got this 💪
Sonja Stoces
This whole 'nocebo effect' thing is just pharma's way of gaslighting patients. If statins were so safe, why are 29% of people quitting? Coincidence? Or are they covering up real toxicity? 🤔
Steve DESTIVELLE
The body is not a machine to be optimized with chemical levers. We have forgotten the wisdom of listening to our flesh. Statins are an imposition of modernity upon the natural rhythm of the human organism. To rechallenge is to surrender to the system that made you sick in the first place.
Skilken Awe
The MEDS approach? More like MEDS-Misleading Evidence, Delusional Science. CK levels? Pfft. Who measures those anymore? And CoQ10? You're telling me a $10 supplement is going to fix what Big Pharma broke? Wake up. This is all just a profit engine.
Jack Havard
62% success rate? That’s just cherry-picked data. What about the 38% who had worse pain the second time? They’re not in the studies. And who’s tracking long-term kidney damage from intermittent dosing? No one. Because money talks.
Rachidi Toupé GAGNON
Switched to pravastatin after 2 years off. Every other day. Took 3 weeks to feel normal. Now I’m biking 30 miles on weekends. My doc said I’m a poster child. Seriously, if you’re scared-try the SAMS-CI. It’s not magic, it’s math.
Alyssa Williams
OMG I did this!! I was on simvastatin 80mg, had cramps so bad I couldn't walk. Quit for 8 months. Then tried fluvastatin 20mg every 3 days. No pain. Cholesterol down. I'm so glad I didn't listen to the 'never restart' crowd. Life is better now 😭❤️
Luke Trouten
The nocebo effect is not merely a psychological phenomenon-it is a reflection of the epistemic rupture between medical authority and lived experience. When patients are told their pain is 'in their head,' the system fails to recognize the phenomenological truth of bodily suffering. Rechallenge protocols, while statistically sound, risk reinforcing this alienation.
Kristin Jarecki
As a lipid specialist, I’ve overseen over 200 rechallenges. The key is not just the statin choice-it’s the conversation. Patients need to understand that their fear is valid, but the risk is often exaggerated. We use SAMS-CI, check thyroid, and start with pravastatin or pitavastatin. Success rates exceed 75% when we do it right. Don’t give up.
Autumn Frankart
They say statins save lives. But what about the ones who died after restarting? The ones they never report? The CDC hides this data. And why? Because if people knew how many got rhabdo from rechallenge, they’d riot. You think this is science? It’s a cover-up. Read the FDA adverse event reports. They’re not lying. They’re just not telling you.
Joanne Tan
I was skeptical but tried every-other-day atorvastatin. First week: still sore. Second week: better. Third week: felt like a new person. My cholesterol’s at 112. I’m 57. I’m alive. Don’t quit. Just change the game.