When it comes to skin cancer, melanoma is the one you can’t afford to ignore. It makes up less than 2% of all skin cancer cases, but it causes more than 80% of skin cancer deaths. The difference between life and death often comes down to one thing: when you catch it. If found early, the 5-year survival rate is over 99%. Once it spreads, that number drops to just 32.1%. That’s not a statistic-it’s a wake-up call.
How Melanoma Is Caught Early-Now
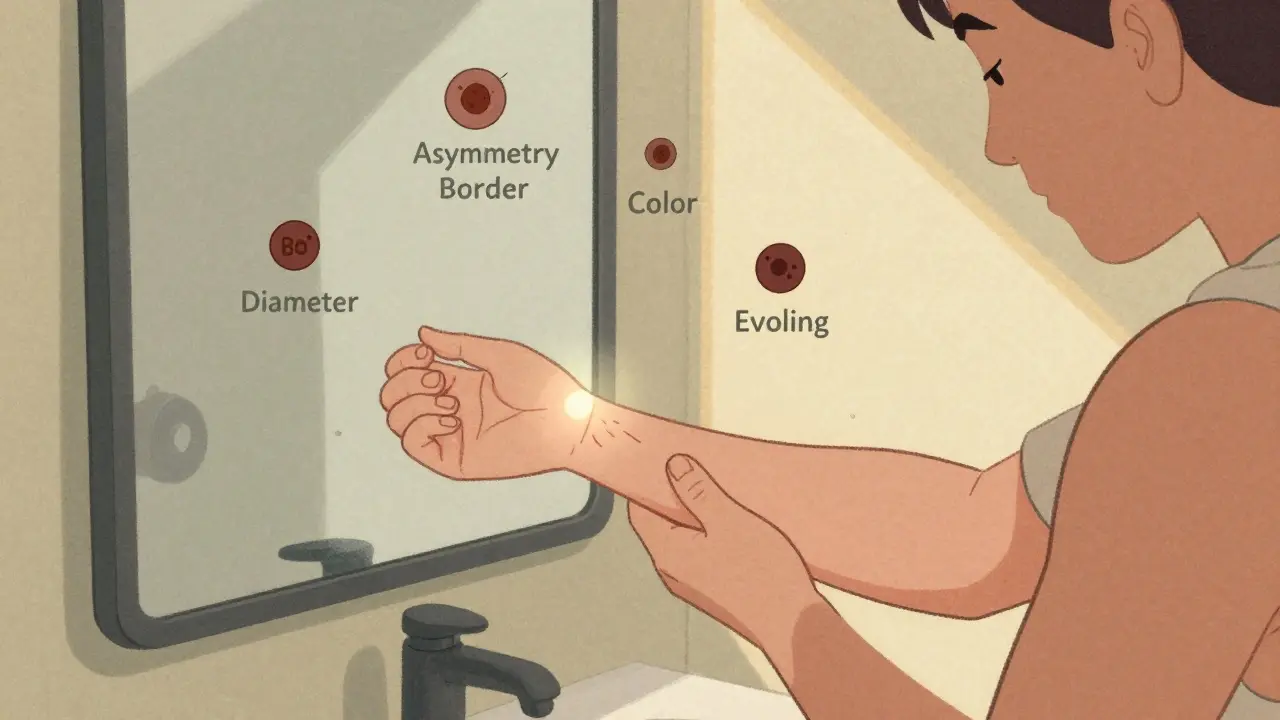
For decades, the only tool doctors had was the naked eye. A suspicious mole, the ABCDE rule-Asymmetry, Border irregularity, Color variation, Diameter larger than 6mm, Evolving over time. But human eyes miss things. Studies show primary care providers detect melanoma correctly only 60-70% of the time. That’s why dermoscopy, a handheld magnifying tool with polarized light, became the next step. Still, even dermatologists can struggle with tricky lesions, especially on darker skin tones where melanoma often looks different. Now, AI is changing everything. Systems like Northeastern University’s SegFusion combine image segmentation and deep learning to isolate suspicious areas before classifying them. It hits 99% accuracy in controlled tests, with 95% sensitivity. That means it catches almost every real melanoma. But here’s the catch: most AI tools are trained on datasets that are mostly light skin tones. A 2025 JAMA Dermatology study found these models perform 12-15% worse on darker skin. That’s not just a technical flaw-it’s a health equity crisis.New Tools Beyond the Dermatoscope
Beyond AI-powered imaging, a wave of new devices is entering clinics. The FDA approved DermaSensor in January 2024. It uses elastic scattering spectroscopy-shining near-infrared light on a mole and measuring how it bounces back. It’s simple: a doctor holds it against the skin, clicks a button, and gets a risk score. Primary care providers using it reported 87% higher confidence. But specificity? Only 26-40%. That means for every 100 patients flagged as high risk, 60-74 are false alarms. More biopsies. More stress. More cost. Then there’s the wearable patch from Wake Forest. No batteries. No wires. Just a small patch you stick on a mole. It measures bioimpedance-the way skin tissue conducts electricity. Cancer cells behave differently than healthy ones. The patch picks up that difference and sends data to a handheld reader. Early tests on 10 people showed clear statistical differences. The next version will use conductive hydrogel to improve contact. Imagine checking your moles at home every morning while brushing your teeth. The iToBoS project, funded by the EU and led by Fraunhofer Institute, takes it further. A full-body scanner walks you through a six-minute scan. It takes hundreds of images, maps every mole, flags anomalies, and explains its reasoning using explainable AI (XAI). Dermatologists in 12 European clinics tested it. They loved the coverage-but 35% of its alerts were false positives. That’s still too high. But the system keeps learning. And it’s the first to show real-time risk scores for every lesion, not just the obvious ones.Why AI Isn’t Perfect-Yet
AI isn’t magic. It’s data. And data is messy. Real-world skin doesn’t look like the clean, well-lit photos in research datasets. Lighting changes. Shadows form. Moles grow under hair. Skin tones vary wildly. Most AI models were trained on images from Europe and North America. They don’t know what melanoma looks like on Black or Brown skin until someone shows them. Then there’s the problem of overdiagnosis. A 2025 paper in Taylor & Francis warned that early detection can lead to catching melanomas that would never have spread. These are slow-growing, harmless lesions. Removing them causes scars, anxiety, and medical bills-with zero survival benefit. The more sensitive the tool, the more of these it finds. That’s why specificity matters as much as sensitivity. Integration is another hurdle. A dermatology clinic in Ohio spent 18 months trying to connect DermaSensor to their electronic health record system. They gave up. Most AI tools don’t talk to EMRs. Doctors have to manually enter results. That’s not efficiency-it’s friction.
What Happens After Diagnosis?
If a biopsy confirms melanoma, the next step depends on how deep it went. Stage I or II? Surgery is usually enough. Stage III? Lymph node removal and maybe immunotherapy. Stage IV? That’s where things get revolutionary. Before 2011, metastatic melanoma meant months to live. Then came ipilimumab, the first immunotherapy to show survival benefit. It worked by releasing the brakes on T-cells-the body’s own cancer fighters. But it had brutal side effects. Then came pembrolizumab and nivolumab, drugs that block PD-1, another brake. Better results. Fewer side effects. Now, the standard is combo therapy: PD-1 + CTLA-4 inhibitors. In clinical trials, over half of patients live five years or more. Some, even ten. Newer drugs are coming fast. Regeneron’s fianlimab (a LAG-3 blocker) paired with a PD-1 drug is showing promise in Phase 3 trials. IMA203, a cell therapy targeting the PRAME protein, achieved a 56% complete response rate in early tests. It’s not a cure, but it’s turning terminal into manageable. The goal now isn’t just survival. It’s quality. These drugs can cause autoimmune reactions-colitis, thyroid issues, rashes. But with careful monitoring, most patients live full lives. One patient I spoke to, a 52-year-old teacher, has been on immunotherapy for 7 years. She hikes, teaches, travels. Her scans are clear. She calls it “living with a timer,” but she’s not waiting to die.What’s Next?
The future isn’t just better tools-it’s smarter integration. Imagine a system that combines your dermoscopy image, your wearable patch data, your genetic markers (like BRAF or NRAS mutations), and your blood biomarkers-all fed into one AI model. That’s what researchers at Fraunhofer and Northeastern are building. They’re even testing if adding your blood pressure or oxygen levels improves predictions. Point-of-care devices for rural clinics are in development. No need for a dermatologist. Just a tablet, a scanner, and a 5-minute test. The WHO estimates this could cut melanoma deaths by 40-50% in the next decade. But adoption isn’t guaranteed. Reimbursement lags behind innovation. Google Health’s DermAssist had 92% accuracy but pulled out of the market in 2024 because insurers wouldn’t pay for it. The same thing could happen to the wearable patch or the full-body scanner.
What You Should Do Now
You don’t need a scanner to save your life. You need awareness. - Check your skin monthly. Use a mirror. Take photos of moles so you can track changes. - Know your risk. Fair skin? Sunburns as a kid? Family history? More frequent checks. - See a dermatologist if a mole changes shape, color, or bleeds-even if it’s small. - If your doctor uses an AI tool, ask: Is it validated for my skin tone? What’s the false positive rate? - Don’t fear biopsies. A biopsy is not a death sentence. It’s a way to know. The tools are getting better. The science is advancing. But early detection still starts with you. Not a machine. Not a doctor. You.Can melanoma be cured if caught early?
Yes. When melanoma is caught before it spreads beyond the top layer of skin, the 5-year survival rate is over 99%. Surgery alone is often enough to remove it completely. Early detection is the most powerful tool we have.
How accurate are AI tools for melanoma detection?
Top AI systems like SegFusion and DenseNet-201 achieve 94-99% accuracy in research settings. But real-world accuracy drops due to lighting, skin tone, and lesion location. Sensitivity (catching real melanomas) is high, but specificity (avoiding false alarms) varies. DermaSensor, for example, has only 26-40% specificity, meaning many benign moles get flagged.
Is immunotherapy better than chemotherapy for melanoma?
For advanced melanoma, yes. Chemotherapy rarely works. Immunotherapy trains your immune system to find and kill cancer cells. It doesn’t kill every tumor, but it can lead to long-term remission. About half of patients on combination immunotherapy live five years or more. Some live over a decade.
Are there side effects to immunotherapy?
Yes. Because immunotherapy turns up your immune system, it can attack healthy organs. Common side effects include fatigue, rash, diarrhea, and thyroid problems. Most are manageable with medication. Severe reactions are rare but require immediate treatment. Patients are monitored closely during treatment.
Should I get a full-body skin scan?
If you have a personal or family history of melanoma, many moles, or fair skin, yes. Even without risk factors, annual skin checks are recommended after age 40. Full-body scanners like iToBoS are still mostly in research settings, but standard dermatologist exams with dermoscopy are widely available and effective.
Do at-home skin scanners work?
Some apps and handheld devices claim to detect melanoma, but most aren’t FDA-cleared or clinically validated. The only devices proven in trials are DermaSensor (FDA-cleared for clinicians) and the Wake Forest wearable patch (still in testing). Don’t rely on phone apps. They’re not accurate enough.
Can AI replace dermatologists?
No. AI is a tool, not a replacement. It helps spot things humans might miss, but only a trained dermatologist can interpret results in context, decide on biopsies, and manage treatment. The best outcome comes from combining human expertise with AI precision.





14 comments
Leonard Shit
man i just checked my arm and there's this one mole i swear wasn't there last week. i'm not gonna lie, i stared at it for 10 minutes like it's gonna tell me if i'm gonna die. also why does everyone act like ai is gonna save us when half these tools can't even tell a mole from a freckle on brown skin?
Rachel Wermager
Let’s be clear: the sensitivity-specificity trade-off in dermal AI isn’t a bug-it’s a systemic failure of training data diversity. SegFusion’s 99% accuracy is lab-glass performance; real-world heterogeneity in pigmentation, lighting, and anatomical location introduces catastrophic bias. The JAMA Dermatology study isn’t an anomaly-it’s the rule. Without ethnically stratified datasets, we’re engineering diagnostic inequity at scale. And DermaSensor’s 26% specificity? That’s not a feature-it’s a liability cascade leading to unnecessary excisions, patient anxiety, and healthcare inflation. We’re optimizing for detection, not clinical utility.
Brian Anaz
so we’re letting some tech bro in california train a robot on pictures of white people and now it’s telling black folks they got cancer when they don’t? that’s not innovation. that’s negligence. america’s gonna die because we’re too lazy to collect real data. fix the system before you slap a shiny app on it.
Kelly Beck
you guys are all so focused on the tech but let’s not forget the human part 🥺✨ like, my aunt got diagnosed because she noticed a tiny spot on her back and just said ‘eh, i’ll get it checked’-and now she’s hiking in patagonia at 68. early detection isn’t about fancy scanners, it’s about paying attention to your own body. if you see something weird, don’t ignore it. don’t overthink it. just go. you’ve got this 💪❤️
Katie Schoen
the fact that we’re even having this conversation about ai and skin tone is wild. we’ve had dermatoscopes for decades and still, we act like the only way to catch melanoma is with a $2000 gadget. sometimes the best tool is a mirror and a 30-second glance while you’re brushing your teeth. also, who else is tired of hearing ‘the future is here’ when the future still can’t tell a mole from a pimple?
Beth Templeton
ai is great until it misdiagnoses your mole because it was trained on 98% white skin then you get a biopsy for nothing. also why is no one talking about overdiagnosis? we’re turning benign moles into trauma.
Dana Termini
i think the real issue isn’t the tech-it’s the assumption that better tools automatically mean better outcomes. if the system doesn’t support access, education, or follow-up, then even the most accurate algorithm won’t save lives. we need infrastructure before we invest in shiny gadgets. also, i’ve seen too many people avoid the doctor because they’re scared of what the machine might say.
Isaac Jules
you’re all acting like this is some noble science mission. it’s a profit-driven mess. companies sell scanners to clinics, clinics bill insurers, insurers don’t reimburse, and patients get stuck with bills for false positives. meanwhile, the real solution-regular self-checks and dermatologist visits-is free and proven. stop chasing robots and start looking in the mirror.
Amy Le
let’s be honest-this whole thing is just capitalism wearing a lab coat. ai, wearables, full-body scanners… all of it. meanwhile, the real fix? sunblock. education. access. but none of that makes investors rich. so we get overhyped gadgets that fail on brown skin and then we act surprised when people die. we’re not solving a medical crisis-we’re selling fear as a subscription.
Pavan Vora
in india, we don’t have access to any of this tech… but we do have grandmothers who know every mole on their family’s skin since birth. maybe the real innovation isn’t in the scanner-it’s in the tradition of paying attention. i’ve seen my uncle’s mole change over 12 years… no machine, just memory and care. maybe we don’t need ai… we need community.
Stuart Shield
there’s something almost poetic about the idea of a little patch you stick on your mole like a temporary tattoo-quiet, unobtrusive, watching over you while you live your life. it’s not flashy, it doesn’t scream ‘future!’-it just… is. and maybe that’s the most human kind of tech: not replacing the doctor, but quietly supporting the ritual of self-care.
Indra Triawan
why do we always think the answer is more technology? we’ve lost touch with the body. we’ve outsourced intuition to machines. and now we’re scared to even look at ourselves. what if the cure isn’t in the data-but in the silence before you reach for the mirror?
Lily Lilyy
Thank you for sharing such an important and life-saving message. Every individual has the power to make a difference by being proactive about their health. Regular skin checks, awareness, and open communication with healthcare providers are truly the most effective tools we have. Let’s encourage everyone-especially those in underserved communities-to prioritize their well-being. Small actions lead to big outcomes. You are worth the check. 💕
Susan Arlene
so i’ve been using that app that claims to scan moles… turns out it thought my freckle was stage 4. i deleted it. also why is everyone acting like ai is gonna fix everything when the real problem is we don’t teach kids to look at their own skin? just saying.