Acromegaly isn’t something you wake up with overnight. It creeps in slowly-your rings don’t fit anymore, your shoes feel tighter, your jawline seems heavier. At first, you blame aging. Maybe it’s just weight gain. But over time, the changes become impossible to ignore. This is acromegaly: a rare hormonal disorder caused by too much growth hormone in adults, usually from a benign tumor on the pituitary gland. Left untreated, it doesn’t just change how you look-it changes how long you live.
What Exactly Is Acromegaly?
Acromegaly happens when your body makes too much growth hormone (GH) after your growth plates have closed-meaning after puberty. In kids, excess GH causes gigantism: they grow tall, proportional, and fast. In adults, there’s nowhere left to grow upward, so the body grows outward. Fingers thicken. Jaw protrudes. Skin gets oily and coarse. Organs enlarge. The result isn’t just cosmetic-it’s dangerous.
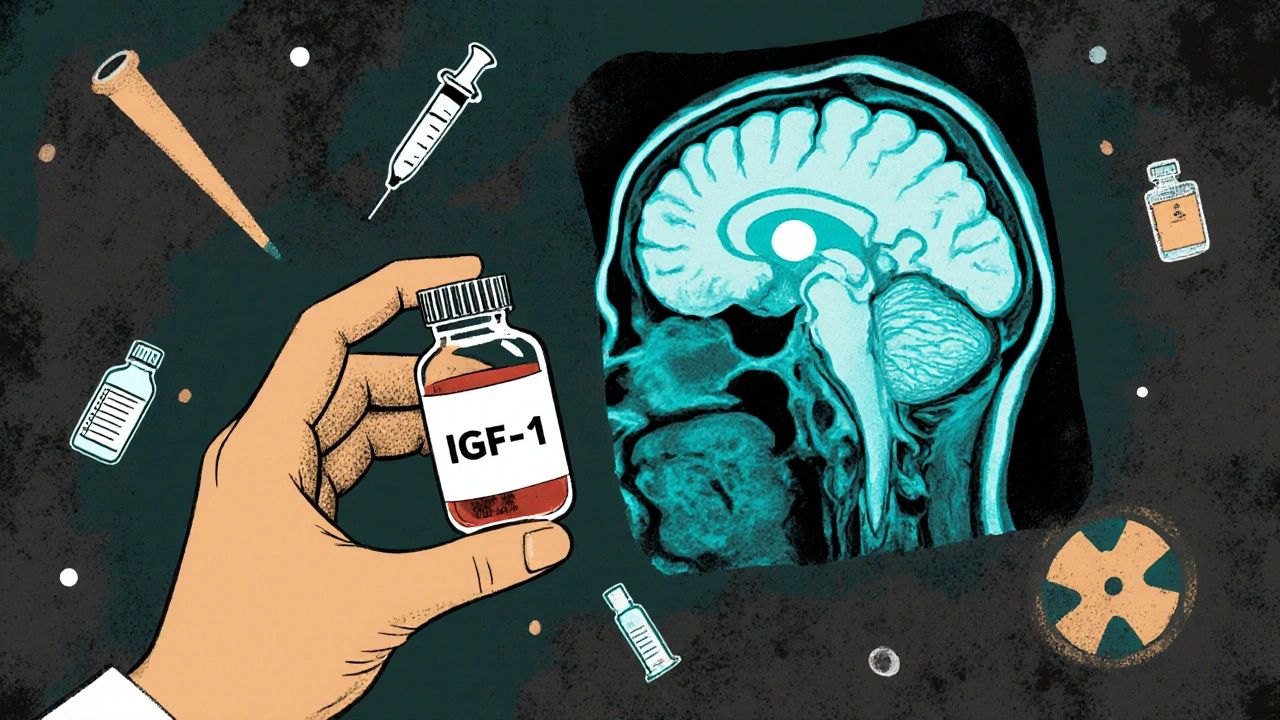
Only about 3 to 4 new cases occur per million people each year. Most are diagnosed between ages 30 and 50. The cause? In 95% of cases, it’s a noncancerous pituitary adenoma. This small tumor, often less than a centimeter wide, sits at the base of your brain and churns out GH like a broken faucet. The liver responds by pumping out insulin-like growth factor-1 (IGF-1), which drives the tissue overgrowth. That’s why doctors test IGF-1 levels-it’s a more stable marker than GH, which spikes and crashes throughout the day.
How Do You Know If You Have It?
Diagnosing acromegaly is hard because the signs show up over years. Many people wait seven to ten years before getting a correct diagnosis. A 2023 survey by Seeing Differences UK found that 68% of patients saw 10 or more doctors before being told what was wrong.
Here’s what to watch for:
- Hands and feet: Ring size increases. Shoe size goes up. You can’t wear your old gloves.
- Face changes: Brow ridge sticks out. Lower jaw juts forward. Nose and lips thicken.
- Skin: Oily, thickened, with deep creases. Excessive sweating.
- Voice: Becomes deeper and hoarser due to vocal cord thickening.
- Joints: Pain, stiffness, arthritis-often mistaken for regular wear and tear.
- Headaches and vision: If the tumor presses on nerves, you may lose peripheral vision or get constant headaches.
- Other symptoms: Sleep apnea (60% of patients), high blood pressure (up to 50%), type 2 diabetes (up to 36%), and erectile dysfunction in men.
Doctors confirm it with two key tests. First, a blood test for IGF-1. If it’s high, they do an oral glucose tolerance test. Normally, sugar intake suppresses GH. In acromegaly, GH stays high-even after drinking a sugary solution. If both tests point to excess GH, an MRI shows the tumor.
Why Timing Matters
Every year without treatment increases your risk of early death. Studies show people with uncontrolled acromegaly are two to three times more likely to die prematurely than the general population. The main culprits? Heart disease, stroke, and breathing problems from sleep apnea.
But here’s the good news: if you get treatment early and bring GH and IGF-1 levels back to normal, your life expectancy can return to normal too. Penn Medicine data shows 90% of patients who achieve biochemical control live as long as people without the disease. That’s not a small win-it’s life-changing.
Treatment Options: Surgery, Medication, Radiation
There are three main ways to treat acromegaly-and they’re often used together.
1. Surgery: The First Step
Transsphenoidal surgery is the go-to first treatment. A neurosurgeon removes the tumor through the nose or upper lip, avoiding brain incisions. Success depends on tumor size. For small tumors (microadenomas, under 10mm), remission rates are 80-90%. For larger ones (macroadenomas), it drops to 40-60%.
Recovery takes 2-4 weeks. Most people notice improvements in facial swelling and headaches within days. But it can take years for joint pain and skin changes to fully reverse. One patient on Reddit shared that it took 18 months for their ring size to drop from 13 to 10-and three years for the joint pain to ease.
2. Medications: Controlling Hormones
If surgery doesn’t fully remove the tumor-or if surgery isn’t an option-medications step in. There are three types:
- Somatostatin analogs: Octreotide (LAR injection) and lanreotide (monthly shots). They block GH release. About 60% of patients see IGF-1 levels drop into normal range. Cost: $6,200-$7,800 per month in the U.S.
- Dopamine agonists: Cabergoline. Less effective than somatostatin analogs, but cheaper-$150-$300/month. Best for patients with mild GH excess or small tumors.
- Growth hormone receptor antagonist: Pegvisomant. It doesn’t reduce GH-it blocks its effect on the liver. Very effective at normalizing IGF-1 (up to 90% of patients), but doesn’t shrink tumors. Cost: $12,000-$15,000/month. Often used when other drugs fail.
Insurance can be a hurdle. In the U.S., 32% of patients report delays of over 30 days for prior authorization on these drugs. Newer formulations, like quarterly pasireotide (Signifor LAR), are now available and may improve compliance.
3. Radiation: Last Resort
Radiation is rarely used first. It’s slow-takes 5-10 years to work-and carries big risks. About 30-50% of patients develop hypopituitarism after radiation, meaning they lose other vital hormones like cortisol, thyroid hormone, or sex hormones. That means lifelong replacement therapy.
It’s usually reserved for cases where surgery and meds haven’t worked. Newer techniques like stereotactic radiosurgery (Gamma Knife) target the tumor more precisely, lowering side effects.
What Happens After Treatment?
Getting GH and IGF-1 levels normal isn’t the end-it’s the beginning. Many patients still struggle with fatigue, joint pain, and sleep apnea even after biochemical control. A 2023 study in the European Journal of Endocrinology found 58% of treated patients still felt tired all the time.
That’s why ongoing care matters. You need:
- IGF-1 blood tests every 3-6 months
- Annual MRI scans to check for tumor regrowth
- Monitoring for hypopituitarism-especially if you had radiation or surgery
- Cardiology and sleep studies to manage heart and breathing issues
- Regular check-ins with an endocrinologist, neurosurgeon, and primary care doctor
Patients treated at high-volume centers (those doing more than 25 acromegaly surgeries a year) report 74% satisfaction. At low-volume centers? Only 49%. Specialization makes a difference.

What’s New in Treatment?
The field is moving fast. In July 2023, the FDA approved a new quarterly version of pasireotide. That’s one shot every three months instead of monthly-big help for people struggling with frequent injections.
Researchers are also testing AI tools. The AcroPEARL study showed facial recognition software could spot acromegaly with 89% accuracy by analyzing subtle changes in photos. Imagine a phone app that flags early signs before you even see a doctor.
Upcoming trials like SONICS are testing whether combining pegvisomant with octreotide works better than either drug alone. Early results suggest it could help patients who’ve hit a wall with current treatments.
Living With Acromegaly
It’s not just about hormones. It’s about identity. People with acromegaly often feel like strangers in their own bodies. Relationships suffer. Jobs get harder. Depression is common.
Support groups matter. Online forums like the Pituitary Network Association and Reddit’s r/Acromegaly are lifelines. One user wrote: “After surgery, I didn’t recognize myself in the mirror. But slowly, I got back the person I was. Not perfect-but me.”
Early diagnosis, expert care, and persistence pay off. With today’s tools, acromegaly is no longer a death sentence. It’s a manageable condition-if you catch it in time.






13 comments
steffi walsh
Just read this and cried a little. I didn’t know I wasn’t alone. My rings stopped fitting in 2019, and I thought I was just getting older. Turns out, it was this. I’m on octreotide now. It’s expensive as hell, but I can finally wear my wedding band again. Thank you for writing this.
Denny Sucipto
Bro, I had this. Took me 8 years to get diagnosed. Doctors kept telling me I was ‘just carrying extra weight.’ One even said I had ‘bad posture.’ I had to drag my own MRI results to a new endo to finally get help. You’re not crazy if your face feels like it’s changing. It’s real.
Conor McNamara
theyre hiding the truth. pituitary tumors? nah. its the 5g towers in the hospitals. theyre feeding you fake data. i saw a guy on youtube with the same face as me. he said the gov made him sick to test the hormone response. i dont trust meds. i tried apple cider vinegar and now my shoes fit better. maybe its the water? i think the water is poisoned.
Leilani O'Neill
It’s embarrassing how long it takes for people in this country to get diagnosed. In Ireland, we have proper endocrinology units. You’d be on treatment within weeks, not years. Why are Americans so lazy about their health? You wait until you can’t button your shirt and then you cry on Reddit? Get a grip.
Shilpi Tiwari
Interesting. The IGF-1 suppression kinetics under pegvisomant are particularly fascinating-especially the dissociation between GH and IGF-1 dynamics. The pharmacokinetic half-life of the receptor antagonist is ~10-12h, but the downstream suppression of hepatic IGF-1 synthesis persists beyond 24h due to transcriptional downregulation. Has anyone looked at the epigenetic markers of GH-responsive genes in treated patients? I’d love to see a GWAS on this cohort.
Christine Eslinger
Thank you for sharing this. I’ve been an endocrine nurse for 18 years and I still get choked up reading stories like this. The real tragedy isn’t the tumor-it’s the delay. If you’re reading this and your rings don’t fit, your jaw feels bigger, or you’re tired all the time-go to an endocrinologist. Don’t wait. You’re not imagining it.
Kristi Joy
For anyone feeling lost after diagnosis: you’re not broken. You’re not a burden. You’re someone who’s been fighting silently for years. I’ve seen patients go from hiding in mirrors to speaking at conferences. It’s not easy, but you’re stronger than you think. Find your tribe. We’re here.
Louie Amour
Let’s be real-this is all Big Pharma’s fault. Why do you think they make these drugs cost $15k/month? They know you’ll pay it. I saw a guy on TikTok who cured himself with turmeric and breathwork. The FDA banned his video. Coincidence? I don’t think so. Someone’s making billions off your confusion.
Hal Nicholas
I knew a guy with this. He looked like a troll. Not metaphorically. Like, literally. He had a forehead like a gorilla and hands like oven mitts. He died at 48. Heart attack. I told him to get it checked. He said ‘it’s just aging.’ Now I’m scared to look in the mirror.
Kristina Williams
My cousin had this. She said the doctors gave her a pill that made her hair fall out. Then she started getting seizures. They said it was ‘side effects.’ I think they poisoned her. They do this to people who talk too much. I heard the pituitary gland is connected to the CIA’s mind control program. That’s why they never tell you the truth.
Riohlo (Or Rio) Marie
How quaint. You’re all treating this like some tragic personal journey. The real issue is the grotesque commodification of rare disease narratives. The ‘lifeline’ of Reddit forums? A performative grief economy. And the ‘AI facial recognition’? A capitalist veneer over biometric surveillance. We’re not patients-we’re data points with facial geometry. Wake up.
Holly Powell
Let’s not romanticize this. The ‘90% survival rate’ is a misleading statistic. It’s based on biochemical normalization, not functional recovery. Most patients still have chronic pain, depression, and social alienation. The data ignores quality of life. You can be ‘normal’ and still be destroyed. This isn’t a success story-it’s a cautionary tale dressed in hopeful language.
Christine Eslinger
Just want to say to the person who said they cried reading this-you’re not alone. I’ve had patients hug me in the hallway after reading something like this. It’s okay to grieve the body you lost. And it’s okay to celebrate the one you’re rebuilding. One day at a time.