Quick Takeaways
- Chronic stress disrupts the hormonal cascade that controls ovulation and sperm production.
- Cortisol, the primary stress hormone, interferes with the HPA axis and reproductive hormones like LH and FSH.
- Both men and women experience lower fertility rates when stress levels stay high for weeks or months.
- Improving sleep, nutrition, and regular mind‑body practices can restore hormonal balance.
- Track stress and fertility markers together; small lifestyle tweaks often yield measurable gains.
What We Mean By "Stress" and "Fertility"
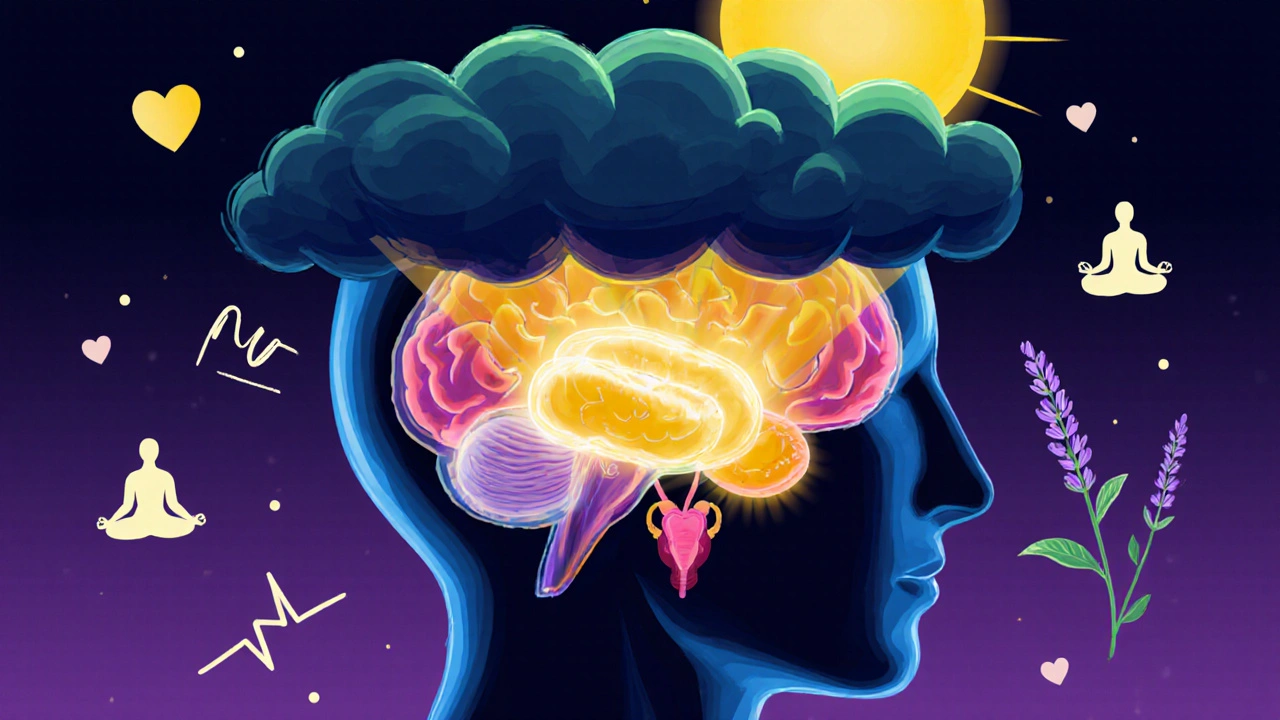
When we talk about Stress is the body’s physiological and psychological response to perceived threats or challenges, triggering the release of hormones like cortisol and adrenaline, we’re not just describing a fleeting feeling. Stress can be acute (a one‑off deadline) or chronic (ongoing financial pressure). Both forms send signals to the brain that ripple through the endocrine system.
Fertility is the capacity of a person’s reproductive system to conceive and sustain a pregnancy, measured by markers such as ovulation regularity, sperm count, and hormone levels. For couples trying to conceive, fertility isn’t just about the reproductive organs; it’s a whole‑body state governed by hormones, metabolism, and even emotional wellbeing.
The Hormonal Highway: How Stress Hijacks Reproduction
The link between stress and fertility runs through a set of key players:
- Cortisol is the primary stress hormone produced by the adrenal glands that rises sharply during stressful events.
- The HPA Axis is the hypothalamic‑pituitary‑adrenal system that regulates cortisol release and interacts with reproductive hormones.
- LH and FSH are luteinizing hormone and follicle‑stimulating hormone, the main drivers of ovulation and sperm maturation.
- Endocrine System is the network of glands (pituitary, thyroid, adrenal, gonads) that secrete hormones controlling growth, metabolism, and reproduction.
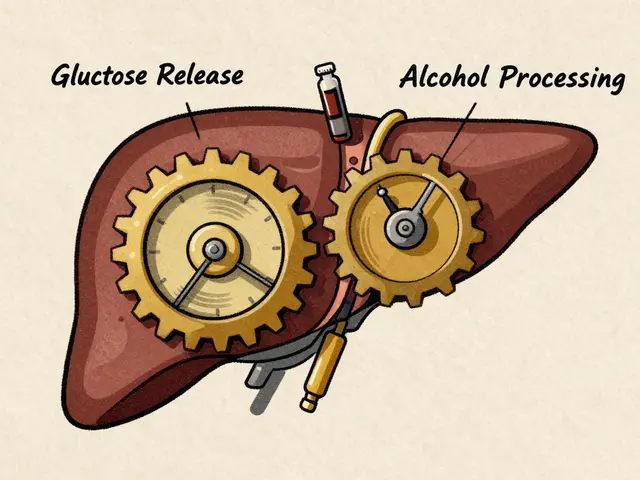
When cortisol spikes, it sends a negative feedback signal to the hypothalamus, reducing the secretion of gonadotropin‑releasing hormone (GnRH). Less GnRH means the pituitary releases less LH and FSH. In women, this can blunt the surge that triggers ovulation; in men, it can dampen the signals that stimulate testicular spermatogenesis.
Research from the University of Auckland (2024) showed that couples with average cortisol levels 30% above baseline experienced a 20% drop in successful conception over six months, even after controlling for age and BMI.
Women’s Fertility Under Stress
For the female reproductive system, the most obvious stress‑related disruptions involve the menstrual cycle:
- Irregular Ovulation: Elevated cortisol can delay or prevent the LH surge, leading to missed or late ovulation.
- Shortened Luteal Phase: Stress may truncate the post‑ovulation phase, reducing progesterone support for implantation.
- Polycystic‑like Symptoms: Chronic stress can increase insulin resistance, mimicking PCOS patterns that hinder ovulation.
Another subtle effect is the impact on the uterine lining. Progesterone, essential for a receptive endometrium, can drop when the HPA axis is overactive, making implantation less likely even if a viable embryo reaches the uterus.

Men’s Fertility Under Stress
Male reproductive health is equally vulnerable, though the signs differ:
- Sperm Count: Chronic cortisol elevates reactive oxygen species (ROS) in the testes, damaging sperm DNA and reducing total count.
- Sperm Motility: Hormonal imbalance can impair the flagellar beat, leading to slower swimming sperm.
- Testosterone Levels: Cortisol competes with testosterone for precursor molecules, often lowering free testosterone by 10‑15% in stressed individuals.
A 2023 meta‑analysis of 15 studies involving over 2,000 men found a consistent 12% reduction in total motile sperm count among those reporting high perceived stress for more than three months.
Lifestyle Stressors That Sneak Into Your Reproductive Health
Not all stress comes from big life events. Everyday habits can generate a low‑grade cortisol drip that erodes fertility over time:
| Stress Level | Key Hormone Change | Typical Fertility Impact |
|---|---|---|
| Low (adequate sleep, balanced diet) | Normal cortisol, balanced LH/FSH | Regular ovulation, healthy sperm parameters |
| Moderate (occasional overtime, intermittent insomnia) | ↑ Cortisol 10‑15% | Occasional cycle irregularities, slight dip in sperm motility |
| High (chronic work pressure, poor sleep, high caffeine) | ↑ Cortisol >30%, ↓ LH/FSH | Missed ovulation, lowered progesterone, reduced sperm count |
Other hidden culprits include excessive caffeine, irregular exercise (either over‑training or sedentary lifestyle), and continuous exposure to digital screens that mess with melatonin production.
Mind‑Body Strategies to Re‑Balance the System
Good news: the same pathways that stress harms can be nudged back into harmony with relatively simple interventions.
- Sleep Hygiene: Aim for 7‑9 hours of uninterrupted sleep. Dark rooms, no screens 30 minutes before bed, and a consistent wake‑time keep cortisol rhythms stable.
- Physical Activity: Moderate aerobic exercise (30minutes, 4‑5 times/week) lowers resting cortisol by up to 20% while boosting circulation to the reproductive organs.
- Mindfulness & Meditation: Daily 10‑minute breathing sessions have been shown to drop cortisol levels by an average of 12nmol/L (about 15%).
- Nutrition: Incorporate omega‑3 rich foods (salmon, walnuts), antioxidants (berries, leafy greens), and adequate zinc (pumpkin seeds) to combat oxidative stress in sperm and support hormone synthesis.
- Social Support: Regular interactions with friends or support groups reduce perceived stress, which translates into measurable hormonal benefits.
For couples actively trying to conceive, tracking both stress (via a simple daily rating) and fertility markers (e.g., basal body temperature, ovulation kits, or semen analysis) creates a feedback loop. When stress spikes, you can pause intense workouts, add a relaxation technique, or adjust sleep habits before it translates into a missed cycle.
Practical Checklist: Turning Knowledge Into Action
- Log your stress level each evening on a 1‑10 scale.
- Record ovulation signs (cervical mucus, temperature) or schedule a monthly semen analysis.
- If stress hits >6 for three consecutive days, insert a 24‑hour “recovery” window: no high‑intensity workout, a short meditation, and an extra half‑hour of sleep.
- Swap one caffeinated drink for an herbal tea rich in L‑theanine (e.g., green tea).
- Schedule a brief “check‑in” with your healthcare provider after six weeks of sustained stress‑reduction efforts to verify hormone levels.
Consistency is key-tiny adjustments add up, and most couples see measurable improvements within two to three menstrual cycles.
Frequently Asked Questions
Can short bursts of stress really affect my chances of getting pregnant?
Yes. Even brief, intense stress spikes can temporarily suppress the LH surge needed for ovulation. In men, a single high‑stress day can increase oxidative stress in sperm, lowering motility for up to 48hours.
Is it safe to continue my regular workout routine while trying to conceive?
Moderate exercise is beneficial. Over‑training (more than 90 minutes of high‑intensity activity daily) can raise cortisol enough to interfere with hormone balance. Aim for moderate cardio and strength sessions, and include rest days.
Do supplements help counteract stress‑induced fertility issues?
Certain nutrients-zinc, selenium, and omega‑3 fatty acids-support hormone production and protect sperm from oxidative damage. They complement lifestyle changes but aren’t a cure‑all. Always discuss dosage with a healthcare professional.
How long does it take for cortisol levels to normalize after a stressful period?
With consistent sleep, nutrition, and stress‑reduction practices, resting cortisol can drop to baseline within 2‑4 weeks. Hormonal recovery for ovulation or sperm production may lag a full cycle behind.
Should I get my hormone levels tested before trying to conceive?
Baseline testing (FSH, LH, estradiol, progesterone for women; testosterone, FSH, LH for men) can identify existing imbalances. Pair this with a stress assessment to see if lifestyle changes are needed before medical interventions.






16 comments
newsscribbles kunle
Listen up, folks – the whole "stress kills fertility" hype is a convenient excuse for people who refuse to take responsibility for their own lifestyle choices. In my country we see countless couples blaming the universe while ignoring the fact that overindulgence in fast food, sleepless nights and endless scrolling on the phone are the real culprits. You can't expect your body to function like a finely tuned engine when you're feeding it junk and staying up till dawn binge‑watching dramas. The hormonal cascade is delicate, and when you treat your body like a trash can, you sabotage the very process that could give you a child. So before you start blaming cortisol, look at the mirror and ask yourself why you let stress become a permanent guest in your home.
Darrin Taylor
All this stress‑fertility research looks suspiciously like a big pharma ploy to sell more antidepressants 🤔💊. They give you a shiny graph about cortisol and then push pills that keep you dependent forever. And don't even get me started on the hidden agenda of fertility clinics – they want you scared so you’ll pay for endless tests. Remember, the brain is designed to keep you alive, not to be manipulated by a corporate lab coat. Keep your eyes open and don't let the narrative control your choices.
Anthony MEMENTO
When one examines the endocrine feedback loops it becomes evident that cortisol exerts a suppressive effect on GnRH secretion ultimately reducing LH and FSH output this cascade is not a myth but a well‑documented phenomenon observed across mammalian species the hypothalamic‑pituitary‑adrenal axis is interwoven with the hypothalamic‑pituitary‑gonadal axis and any chronic elevation of cortisol perturbs the delicate balance of reproductive hormones in both sexes furthermore prolonged cortisol exposure leads to increased oxidative stress within the testes impairing spermatogenesis and DNA integrity in sperm cells similarly in females elevated cortisol can induce luteal phase defects and alter endometrial receptivity thereby compromising implantation the literature from the University of Auckland 2024 provides empirical evidence linking a thirty percent rise in baseline cortisol to a twenty percent decline in conception rates across a six‑month trial period these findings are corroborated by meta‑analyses that report a consistent twelve percent reduction in total motile sperm count among men experiencing high perceived stress for longer than three months the physiological basis for these observations includes cortisol‑mediated inhibition of gonadotropin‑releasing hormone and the resultant downstream hormone deficiencies this is further compounded by cortisol's competition for steroidogenic substrates which diminishes testosterone synthesis and progesterone production respectively the net effect is a reduced probability of successful fertilization and implantation for both partners a comprehensive approach that includes stress reduction techniques such as adequate sleep regular moderate exercise and mindful breathing can mitigate the hyper‑cortisolemic state and restore hormonal equilibrium the body’s ability to recover follows a temporal lag often spanning a full menstrual cycle for women and a spermatogenic cycle of approximately sixty to seventy days for men thus patience alongside lifestyle modifications remains essential for reversing stress‑induced fertility impairments
aishwarya venu
I love how this article breaks down the science into bite‑size pieces and gives practical tips – turns out a simple 10‑minute breathing break can actually lower cortisol and help the ovulation clock get back on track. It’s encouraging to see the mind‑body link backed by data, especially the part about sleep hygiene stabilising hormone rhythms. For anyone feeling overwhelmed, the checklist feels doable and not like another set of impossible goals.
Amanda Joseph
Wow, stress‑free eggs? Yeah right.
Kevin Aniston
Hey everyone – I totally get where you’re coming from. From my experience coaching couples, the biggest game‑changer is consistency. You don’t have to overhaul your entire life overnight, just add a few small habits. First, make sleep non‑negotiable – set a bedtime alarm if you have to. Second, incorporate a low‑intensity walk after dinner; that’s a natural cortisol reducer. Third, keep a simple stress journal – a line a day about how you felt and any triggers. Over a few weeks you’ll notice patterns and can tweak accordingly. Also, remember to stay hydrated and eat a balanced plate with omega‑3s; they protect sperm DNA. The goal is to create a feedback loop where lower stress leads to better hormones, which in turn makes you feel less stressed. Little wins add up, and you’ll likely see a difference in cycle regularity or sperm parameters within a couple of months. Keep at it and don’t get discouraged if progress feels slow – the body loves consistency above all.
kiran kumar
Yo, while you all are busy sipping herbal tea, remember that the whole "cortisol is bad" story is overhyped. Our ancestors lived under real stress – predators, famine – and they reproduced just fine. Modern life adds noise but the body adapts. If you’re constantly measuring stress levels, you might be creating the problem yourself. Chill out, focus on real basics like decent meals and some fresh air, not endless hormone tracking.
Brian Johnson
Interesting read! I’ve noticed that when my partner and I make a point to unwind together, whether it’s a short walk or just a quiet evening, our stress scores seem to drop and we feel more in sync. It’s amazing how small shared moments can have a ripple effect on our overall wellbeing and, by extension, our fertility journey.
Jessica Haggard
Totally agree with Brian – nurturing the relationship is a huge piece of the puzzle. When the emotional climate at home is supportive, the body’s stress response eases up, making the hormonal environment more favourable for conception.
Poppy Johnston
Building on Kevin’s advice, I’d add that staying hydrated can actually influence cortisol metabolism. I’ve seen many couples underestimate the power of a good water intake routine, especially when they’re juggling work and trying to conceive. Thumbs up for those incremental changes!
Johnny VonGriz
Nice points all around. To keep the conversation moving, I’d suggest setting realistic micro‑goals each week – like a 5‑minute meditation before bed or a tech‑free dinner. Tracking those tiny wins keeps motivation high without adding pressure.
Spencer Riner
One angle many overlook is the role of environmental toxins – think phthalates in plastics or BPA in cans. Even low‑level exposure can subtly disrupt endocrine function, compounding stress‑related effects on fertility. Reducing those sources where possible adds another layer of protection.
Joe Murrey
True, Spencer. I’ve started swapping out plastic containers for glass, and while it’s a small tweak, it feels like taking back control over my health.
Tracy Harris
While the empirical data presented herein is commendable, one must also consider the sociocultural determinants that exacerbate stress beyond mere physiological parameters. The modern work‑life paradigm, often characterized by relentless deadlines and the perpetual connectivity afforded by digital devices, cultivates an environment where cortisol elevations become chronic rather than episodic. Moreover, the psychological burden imposed by societal expectations surrounding parenthood adds a layer of anticipatory anxiety that further dysregulates the hypothalamic‑pituitary‑gonadal axis. Thus, a holistic approach to fertility must integrate not only the biomedical interventions outlined but also a critical reevaluation of societal structures that perpetuate undue stress among prospective parents.
Sorcha Knight
Wow Tracy, that was deep! 🙄 But seriously, all this talk about stress sounds like just another excuse to blame ourselves. Maybe we should just chill and enjoy life instead of turning every heartbeat into a science experiment 😂.
Jackie Felipe
Actually, ignoring the science won’t help. Simple steps like cutting down on caffeine and getting enough sleep are easy wins. We don’t need to overthink it.