SSRI Hyponatremia Risk Estimator
This tool estimates your risk of hyponatremia (low sodium) while taking SSRIs. Risk increases with age, female gender, low body weight, and specific medications.
Estimated Risk:
Based on:
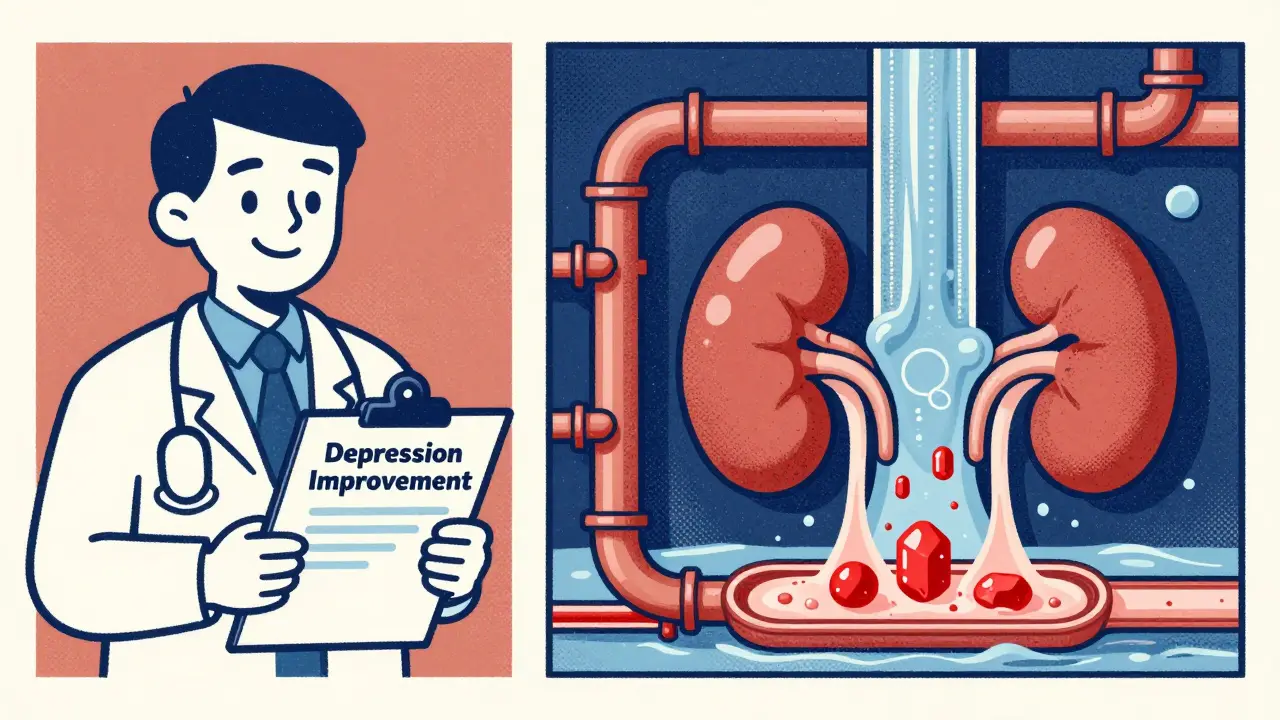
When you start an SSRI for depression, you expect to feel better - not worse. But for some people, especially older adults, the very medication meant to lift their mood can quietly mess with their body’s sodium balance, leading to confusion, dizziness, and even hospitalization. This isn’t rare. It’s a well-documented, often missed side effect: hyponatremia - dangerously low sodium in the blood.
What Is Hyponatremia, and Why Does It Happen with SSRIs?
Hyponatremia means your blood sodium level drops below 135 mmol/L. Sodium isn’t just table salt - it’s critical for nerve function, muscle control, and fluid balance. When levels fall too far, your brain swells. That’s when symptoms like confusion, headaches, nausea, and seizures start showing up. In severe cases, sodium can dip below 120 mmol/L - a medical emergency. SSRIs - drugs like citalopram, sertraline, fluoxetine, and paroxetine - cause this by overstimulating the hormone that tells your kidneys to hold onto water. It’s called SIADH: Syndrome of Inappropriate Antidiuretic Hormone Secretion. Your body keeps drinking water, but doesn’t flush out the excess. The result? Diluted blood. Sodium gets spread too thin. This isn’t a guess. A 2024 meta-analysis of over 30 studies confirmed it: SSRIs trigger hyponatremia in 1.9% to 4.4% of users. For people over 65? That jumps to nearly 1 in 6. And it usually shows up within two to four weeks of starting the drug - right when patients and doctors are celebrating early antidepressant progress.Who’s Most at Risk?
Not everyone on SSRIs gets hyponatremia. But certain people are far more vulnerable:- Age 65+: Risk triples compared to younger adults. Their kidneys don’t handle fluid shifts as well.
- Women: Nearly two-thirds of cases occur in women, possibly due to body composition and hormonal factors.
- Low body weight (<60 kg): Less total fluid means even small water gains cause bigger sodium drops.
- Already on diuretics: Thiazide diuretics (like hydrochlorothiazide) increase hyponatremia risk by over four times.
- Chronic kidney disease: An eGFR under 60 means your kidneys can’t regulate sodium properly.
- Starting or increasing the dose: The biggest spike in risk happens in the first 30 days.
Which SSRIs Are Riskiest?
Not all SSRIs are created equal when it comes to sodium risk. The 2024 study ranked them:- Citalopram: Highest risk (odds ratio 2.37)
- Sertraline: Very high risk (OR 2.15)
- Fluoxetine: High risk (OR 1.98)
- Paroxetine: Moderate risk (OR 1.82)
What Are the Alternatives?
If you’re over 65, have kidney issues, or take diuretics - there’s a safer option: mirtazapine. Mirtazapine isn’t an SSRI. It works differently - blocking certain serotonin receptors instead of boosting serotonin levels. And it doesn’t trigger SIADH. The same 2024 study found mirtazapine carries less than half the risk of SSRIs. For every 1,000 patients treated, SSRIs cause 18.6 cases of hyponatremia. Mirtazapine? Only 6.5. That’s a number needed to harm (NNH) of 82 - meaning you’d have to treat 82 people with an SSRI to cause one case of low sodium. Bupropion (Wellbutrin) is another alternative. It doesn’t affect serotonin much at all. Its hyponatremia risk is nearly the same as placebo. SNRIs like venlafaxine and duloxetine carry moderate risk - higher than mirtazapine, lower than citalopram. The American Geriatrics Society now lists SSRIs as potentially inappropriate for older adults - specifically because of hyponatremia. Their official recommendation? Start with mirtazapine or bupropion if depression is the main issue.How Is It Diagnosed and Treated?
Doctors don’t always test for hyponatremia. But they should. Here’s what they look for:- Serum sodium below 135 mmol/L
- Urine sodium above 30 mmol/L (your kidneys are holding onto salt - a sign of SIADH)
- Urine osmolality above 100 mOsm/kg (your urine is concentrated, meaning your body is retaining water)
- Normal volume status - no swelling or dehydration (euvolemic)
What Should You Do Before Starting an SSRI?
If you’re over 65, or taking diuretics, or have kidney problems - ask for a baseline blood test before starting any antidepressant. Then get sodium checked again at two weeks. Most doctors don’t do this. A 2023 survey found 63% of primary care physicians didn’t know hyponatremia typically appears within 2-4 weeks. Only 29% of patients were warned about this risk before starting SSRIs. Don’t assume your doctor knows. Ask: “Could this medication lower my sodium? Should I get a blood test before and after starting it?” If you’re already on an SSRI and notice new confusion, nausea, headaches, or unexplained falls - get your sodium checked. Don’t wait. Don’t blame it on aging.
Why Is This Still Overlooked?
Hyponatremia from SSRIs is invisible. It doesn’t show up on scans. It doesn’t cause rashes. It doesn’t make you vomit. It just makes you slow, forgetful, off-balance. In older adults, those symptoms are often written off as “just getting older.” But they’re not. In one study, the average time from symptom onset to correct diagnosis was over 7 days. By then, brain damage can already be happening. The cost? In the U.S. alone, SSRI-induced hyponatremia costs $1.27 billion a year - mostly from ER visits and hospital stays. And that’s just the recorded cases. Experts estimate nearly 40% of mild cases go undetected in primary care.What’s Changing Now?
The FDA now requires all SSRI labels to include hyponatremia warnings. The European Medicines Agency is reviewing SSRI safety with a focus on electrolytes - results expected by late 2025. Prescribing patterns are shifting. Between 2018 and 2023, SSRI use in people over 65 dropped 22%. Mirtazapine prescriptions for that group rose 35%. By 2027, mirtazapine is projected to be used in over 40% of antidepressant starts for older adults. That’s not just a trend - it’s becoming standard.Bottom Line: Safety First
SSRIs work. They save lives. But they’re not risk-free - especially for older adults and those on other medications. If you’re considering an SSRI and you’re over 65, have kidney disease, or take diuretics - ask about alternatives. Mirtazapine works just as well for depression, with far less risk. Bupropion is another solid choice. Get your sodium checked before you start. Get it checked again at two weeks. If you feel confused, dizzy, or unusually tired after starting an antidepressant - don’t ignore it. Ask for a simple blood test. Low sodium doesn’t announce itself with a siren. It whispers. And by the time it shouts, it’s already too late.Can SSRIs cause confusion in elderly patients?
Yes. SSRIs can cause confusion in elderly patients due to hyponatremia - low sodium in the blood. This happens when the medication triggers excessive water retention, diluting sodium levels. Symptoms like disorientation, memory lapses, and dizziness are often mistaken for dementia or normal aging, but they’re signs of a treatable medical condition. If confusion appears within weeks of starting an SSRI, a blood test for sodium is essential.
How long does it take for hyponatremia to develop after starting an SSRI?
Hyponatremia usually develops within two to four weeks of starting an SSRI or increasing the dose. This is why guidelines now recommend checking serum sodium levels at the two-week mark. Cases have been reported as early as five days after starting the medication, especially in high-risk patients like older adults or those on diuretics.
Which antidepressant has the lowest risk of causing low sodium?
Mirtazapine has the lowest risk of causing hyponatremia among commonly prescribed antidepressants. Studies show its risk is less than half that of SSRIs. Bupropion is also a low-risk option, as it doesn’t significantly affect serotonin levels. For patients over 65 or those with kidney issues, these are often preferred over SSRIs like citalopram or sertraline.
Should I get my sodium levels checked before starting an SSRI?
Yes - especially if you’re over 65, have kidney disease, or take diuretics. A baseline sodium test before starting an SSRI is now considered standard of care by major psychiatric guidelines. A second test at two weeks helps catch early drops before symptoms become severe. Many doctors don’t order these tests routinely, so ask for them.
Can hyponatremia from SSRIs be reversed?
Yes, in most cases. If caught early, stopping the SSRI and limiting fluid intake can restore sodium levels within 2-4 days. For severe cases (sodium below 125 mmol/L), hospital treatment with controlled IV saline is needed. The key is avoiding rapid correction - too fast can cause permanent brain damage. With proper management, full recovery is common, but delays in diagnosis can lead to lasting neurological effects.
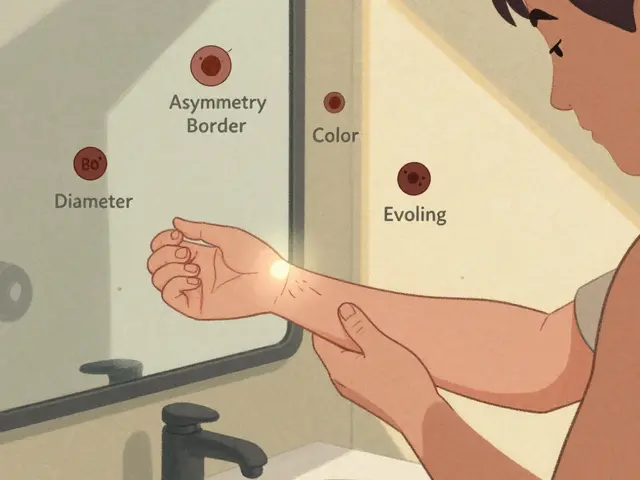
Are there any warning signs before hyponatremia becomes serious?
Yes. Early signs include mild nausea, headache, fatigue, and loss of appetite - symptoms easily dismissed as side effects of the medication or general aging. As sodium drops further, confusion, unsteadiness, and muscle weakness appear. If you notice new mental changes or frequent falls after starting an SSRI, don’t wait. Request a blood test. These early signs are your body’s warning before a crisis.






13 comments
Chris Clark
I saw this happen to my uncle after he started sertraline. He got so confused he forgot his own address. Doctors thought he was having early dementia. Turned out his sodium was at 128. Took 3 days in the hospital to fix it. No one asked about meds until we pushed.
Nancy Kou
This is why I always tell my elderly patients to drink water only when thirsty, not on a schedule. SSRIs make your body think it’s drowning even when it’s not. Simple fix: stop forcing fluids and check labs early.
Janelle Moore
They don't want you to know this. Big Pharma knows SSRIs cause brain swelling but they bury the data. Look at the FDA warnings buried in the 47-page insert. They profit off hospital stays. They want you confused so you keep taking it.
Henry Marcus
It's not just SSRIs... it's the entire pharmaceutical-industrial complex. They pump out these drugs like candy, then sell you the antidotes. Sodium levels? That's just the tip of the iceberg. They've been doing this since the 50s with lithium, insulin, you name it. The system is rigged.
Frank Drewery
I'm so glad someone's talking about this. My mom went through this last year. We almost lost her. But now she's on a different med and her sodium's back to normal. It's scary how fast it can happen. Please, if you're on an SSRI and feel off, get a blood test. Don't wait.
Ryan van Leent
People just blame the meds but no one talks about how lazy doctors are. They prescribe SSRIs like they're vitamins. No labs. No follow up. Just here's your script. Go be happy. Meanwhile grandma's brain is swelling and nobody cares
Sajith Shams
This is basic pharmacology 101. SIADH is textbook. If you're over 60 and on an SSRI and you're not getting sodium checked every two weeks, you're being negligent. I've seen 12 patients this year alone with sodium under 125. All of them were told it was 'just aging'.
Adrienne Dagg
I’m so glad this got posted 😔 My aunt had this and no one knew why she was so out of it. They thought it was Alzheimer’s. Turned out it was citalopram. She’s fine now but it took 3 months to figure it out. Please, if you’re on these meds, get tested. It’s easy. It’s free. It could save your life 💔
Chris Davidson
Hyponatremia is a known side effect. It is not rare. It is documented. It is predictable. The failure lies in clinical oversight not in the medication itself. Physicians must monitor electrolytes in at-risk populations. This is not a scandal. It is standard care.
Glen Arreglo
I work in geriatrics. We catch this early now because we check sodium on day 14 of any new SSRI. If you're over 65, female, under 120 lbs, and on paroxetine? You're basically a walking time bomb unless you're monitored. It's not paranoia. It's protocol.
benchidelle rivera
If you're caring for someone on an SSRI, especially an older adult, know the signs: confusion, stumbling, nausea without food poisoning, headaches that don't go away. Don't assume it's dementia or stress. Get a basic metabolic panel. It takes 10 minutes. It could mean the difference between a hospital stay and a walk in the park.
holly Sinclair
It's fascinating how a drug meant to regulate mood ends up disrupting the most fundamental homeostatic mechanisms of the body. Sodium isn't just a mineral-it's the osmotic anchor of cellular life. When SSRIs hijack vasopressin signaling, they don't just alter fluid balance-they subtly rewire the body's perception of its own internal environment. The brain, which evolved to prioritize survival, interprets dilution as threat, triggering cascades of neuroendocrine chaos. We treat depression with a chemical that makes the body think it's dying of thirst while drowning in water. The irony isn't lost on me. We're trying to heal the mind by destabilizing the very chemistry that makes thought possible.
Monte Pareek
I'm a pharmacist and I tell every patient over 60 starting an SSRI: drink when you're thirsty, not because you're told to. And get a basic metabolic panel at 2 weeks. No excuses. I've seen too many people get rushed to the ER because their doc said 'it's fine' and didn't check sodium. It's not complicated. It's not expensive. It's not optional. If you're on an SSRI and you're over 65, this isn't a suggestion-it's your lifeline.