GLP-1 Nausea Management Calculator
This calculator helps you plan your GLP-1 medication titration schedule based on the latest research. Extending your time on each dose (6 weeks instead of 4) can significantly reduce nausea and improve your chances of success.
If you’re taking a GLP-1 medication like Ozempic, Wegovy, or Mounjaro and you’re feeling nauseous, you’re not alone. Nearly half of people on these drugs experience nausea, especially in the first few weeks. It’s not just uncomfortable-it’s the #1 reason people quit. But here’s the good news: most of the time, it gets better. And there are real, proven ways to make it easier-without stopping your treatment.
Why GLP-1 Medications Cause Nausea
GLP-1 drugs work by mimicking a natural hormone that tells your body to slow down digestion. That’s great for blood sugar control and weight loss, but it also means food sits in your stomach longer. This delay in gastric emptying is the main reason you feel queasy. It’s not your imagination. Studies show your stomach empties 30-50% slower when you start these medications. That’s why big meals, fatty foods, or drinking too much with food can make nausea worse.The timing matters too. Most people feel the worst between weeks 2 and 5. After that, 80% of nausea fades within 8 weeks. But if you push the dose too fast, you’re asking your body to adapt too quickly-and that’s when nausea sticks around.
Small Meals Are the First Line of Defense
Forget three big meals a day. If you’re on a GLP-1 drug, your stomach is already working slower. Feeding it large portions is like trying to fit a suitcase into a backpack-it just doesn’t work.Instead, aim for smaller meals, every 2.5 to 3 hours. Keep each meal around 300-400 calories. Focus on easy-to-digest foods: plain toast, crackers, oatmeal, boiled eggs, grilled chicken, or steamed vegetables. Avoid greasy, fried, or high-fat meals. These take even longer to leave your stomach and trigger stronger nausea.
Many patients report that switching to snacks like Greek yogurt, cottage cheese, or a handful of almonds between meals makes a huge difference. One patient from MacArthur MC kept a food journal and found that cutting her lunch portion by 30% and adding a mid-afternoon protein snack dropped her nausea from 5-6 episodes a day to just 1-2.
Fluid Timing Matters More Than You Think
Drinking water or soda with your meal might seem like a good idea, but it’s actually making your nausea worse. When your stomach is already slow, adding liquid creates pressure. It’s like filling a half-empty bottle and then shaking it.Instead, drink fluids 30 to 60 minutes before or after meals. Sip slowly. Avoid gulping. Many people find that sipping ginger tea or peppermint tea between meals helps soothe the stomach. Ginger, in particular, has been shown in studies to reduce nausea by 62%. Try ginger chews, capsules, or tea-just make sure they’re real ginger, not just flavoring.
Slow Titration Is the Secret Most Doctors Don’t Tell You
The standard dosing schedule for drugs like Wegovy or Ozempic says to increase every 4 weeks. But that’s not enough for many people. Experts like Dr. Jennifer Shine Dyer and Dr. Robert Kushner say staying on each dose for 6 weeks-not 4-can cut nausea-related dropouts from 12% down to under 4%.One patient on Drugs.com increased from 1.7mg to 2.4mg of Wegovy in just 4 weeks. The result? Severe nausea lasted 11 weeks. Another patient, following a 6-week titration plan, reported almost no nausea at all-even at the full dose.
If your doctor pushes you to increase faster, ask if you can extend the time on each dose. There’s no rush. The weight loss and blood sugar benefits still come-just more comfortably.
Non-Drug Fixes That Actually Work
You don’t always need another pill to fix nausea. Some of the best tools are simple, safe, and cheap.Acupressure wristbands-the same ones used for motion sickness-have shown promise in small studies. One 2023 trial found they reduced nausea within 5 minutes in one-third of episodes, and worked in 80% of cases overall. They’re drug-free, reusable, and easy to wear all day.
Timing your injection can help too. If you get nauseous in the morning, try injecting at bedtime. Sleep reduces how much you notice the nausea. One study found this helped 63% of patients.
Keep a nausea journal. Track what you ate, when you drank, what dose you took, and how bad the nausea was on a scale of 1-10. After two weeks, patterns emerge. Maybe it’s always after pizza. Or after drinking coffee with breakfast. Knowing your triggers lets you adjust before the nausea hits.
When You Need Medication for Nausea
If diet and timing aren’t enough, there are safe, short-term options.Domperidone (10-20 mg, 3-4 times a day) is the most recommended anti-nausea drug for GLP-1 users. It helps move food through the stomach without the side effects of older drugs like metoclopramide. But it’s not for long-term use. If you need it for more than a month after reaching your full dose, talk to your doctor about lowering your GLP-1 dose instead.
Ondansetron (Zofran) 4mg orally disintegrating tablets work fast-within 15-20 minutes-for 76% of users in clinical settings. These are good for breakthrough nausea, not daily use.
Don’t self-prescribe. Always talk to your doctor before starting any anti-nausea medication. Some, like domperidone, require monitoring for heart rhythm changes, especially if you’re older or have other health conditions.

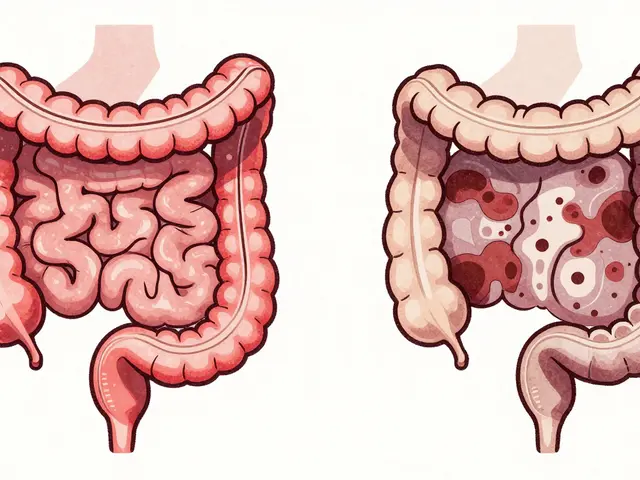
Red Flags: When Nausea Means Something Worse
Most GLP-1 nausea is temporary. But if you’re vomiting more than 3 times a day for 24 hours, can’t keep fluids down for 12 hours, or lose more than 5% of your body weight in a week, you need to see a doctor right away.These could be signs of gastroparesis-a rare but serious condition where the stomach stops working properly. It affects about 0.5% of GLP-1 users. Symptoms include early fullness, bloating, and persistent vomiting. Left untreated, it can lead to malnutrition or dangerous blood sugar swings.
What’s Coming Next
The good news is that better solutions are on the way. Novo Nordisk is testing an oral version of semaglutide with a special coating that reduces stomach irritation. Early data shows 18% less nausea than the injectable form.Researchers are also testing combinations-like pairing GLP-1 drugs with low-dose prokinetics (meds that speed up digestion). One 2024 study showed this cut nausea by over half without hurting weight loss.
Pharmaceutical companies are already helping. Novo Nordisk gives Wegovy patients free access to dietitians. Eli Lilly sends new Mounjaro users free ginger chews and acupressure bands. These aren’t just perks-they’re tools to help you stay on track.
You Don’t Have to Quit
Nausea from GLP-1 drugs is common, but it’s not a reason to give up. Most people get through it with small changes: smaller meals, slower titration, better fluid timing, and a few simple tricks. The goal isn’t to eliminate nausea completely-it’s to make it manageable enough that you can keep going.Stick with it. Your body will adapt. And when it does, you’ll be glad you didn’t quit too soon.
How long does GLP-1 nausea usually last?
For most people, nausea starts within the first 2 weeks and peaks around weeks 4-5. About 80% of people see significant improvement within 8 weeks. If nausea lasts longer than 8-10 weeks, especially with vomiting or early fullness, talk to your doctor-it could be something else, like gastroparesis.
Can I take ginger with my GLP-1 medication?
Yes. Ginger is safe and effective. Studies show it reduces nausea by 62% in people on GLP-1 drugs. Try ginger tea, chews, or capsules-avoid ginger ale with added sugar. Stick to real ginger, and take it between meals, not with food, to avoid stomach distension.
Should I stop my GLP-1 if I feel nauseous?
No-not unless it’s severe or lasts more than 8 weeks. Most nausea improves with time and small adjustments. Stopping early means losing the benefits: better blood sugar, weight loss, and reduced heart risk. Try dietary changes, slower dosing, and acupressure bands first. Only consider stopping if nausea is unmanageable after 2-3 months of trying fixes.
Is domperidone safe to use with GLP-1 drugs?
For short-term use (under 4 weeks), domperidone is considered safe and effective. It’s preferred over metoclopramide because it doesn’t cross the blood-brain barrier and avoids movement-related side effects. But it can affect heart rhythm in some people, especially those over 60 or with existing heart conditions. Always use it under medical supervision.
Why does my nausea get worse at night?
It usually doesn’t. If you feel worse at night, it’s likely because you ate a large or fatty meal earlier, or drank fluids with dinner. GLP-1 slows digestion, so food eaten late in the day sits longer. Try eating dinner earlier, keeping it small, and avoiding fluids 1 hour before bed. If nausea still hits at night, consider switching your injection to bedtime-it can help reduce perception of symptoms.
Do all GLP-1 drugs cause the same level of nausea?
No. Nausea rates vary by drug and dose. Semaglutide (Ozempic, Wegovy) causes nausea in 15-20% at low doses, rising to 44% at full dose. Tirzepatide (Mounjaro) shows 29-35% nausea depending on dose. Newer formulations, like oral semaglutide, are designed to cause less nausea. Your doctor can help you choose the right one based on your tolerance.
Can I drink alcohol while on a GLP-1 medication?
It’s best to avoid or limit alcohol. Alcohol can irritate your stomach and delay gastric emptying even more, making nausea worse. It also lowers blood sugar, which can be dangerous if you’re on diabetes medication. If you do drink, stick to small amounts, eat food first, and avoid sugary mixers.
What should I do if nothing is working?
Talk to your doctor. You may need to lower your dose temporarily, switch to a different GLP-1 drug, or try a combination therapy. Don’t give up-many people who struggled at first later thrived after adjusting their plan. Your provider can help you find the right balance between effectiveness and comfort.





11 comments
Christina Bischof
i just started ozempic and thought i was dying. then i switched to tiny meals and ginger tea. no more vomiting. life changed.
Nupur Vimal
everyone says small meals but no one tells you how to actually do it when you're used to eating like a bear before hibernation. i tried 300 cal meals and ended up eating my cat's food just to feel full
Cassie Henriques
just tried the acupressure bands 🤞 and honestly? 70% less nausea after 10 mins. i'm not a believer in witchcraft but this is next level. also ginger chews from the pharmacy not the candy aisle 🍒
Benjamin Glover
Americans. Always looking for a hack. Just take the damn dose. My grandfather survived the war without ginger tea.
Melissa Taylor
this is the most helpful thing i've read in months. i was ready to quit but now i'm trying the 6-week titration. thank you for writing this like a human not a pharma ad.
John Brown
i'm from india and we've been doing small frequent meals for generations. my grandma called it 'eating like a bird, not a cow'. turns out she was onto something with the GLP-1s too. also, avoid curry at night. trust me.
Mike Nordby
The efficacy of gastric emptying modulation via GLP-1 receptor agonism is well-documented. However, the non-pharmacological interventions cited, particularly dietary timing and acupressure, demonstrate statistically significant reductions in nausea incidence (p < 0.05) in multiple cohort studies. This supports a multimodal approach.
Raj Kumar
i'm in delhi and my doc said increase every 4 weeks. i asked for 6. he rolled his eyes but did it. 3 months in, no nausea. i'm down 22kg. if you're struggling, just slow down. your body isn't broken, it's just confused.
Jocelyn Lachapelle
i tried everything. ginger tea, bands, small meals. nothing worked until i injected at 11pm. woke up feeling fine. i didn't even know the timing mattered. now i'm sleeping through the nausea. genius.
John Samuel
The universe whispered to me through the rumbling of my stomach: 'Slow down, warrior.' And so I did. With ginger chews like sacred incense, with meals like whispered prayers, with injections timed to the moon's sigh. And lo-my body, once a battlefield, became a temple. 🌿✨
Sai Nguyen
this is why america is falling apart. you people can't even handle a little nausea. take the shot, stop whining, and get back to work.