When you vomit something that looks like coffee grounds, or pass black, tarry stools, it’s not just indigestion. It’s a medical emergency. Upper GI bleeding isn’t rare-it happens to about 100 people per 100,000 every year in the U.S., and it can kill if not handled fast. The bleeding comes from the esophagus, stomach, or first part of the small intestine. The two biggest culprits? Peptic ulcers and esophageal varices. And the difference between life and death often comes down to how quickly you get stabilized and diagnosed.
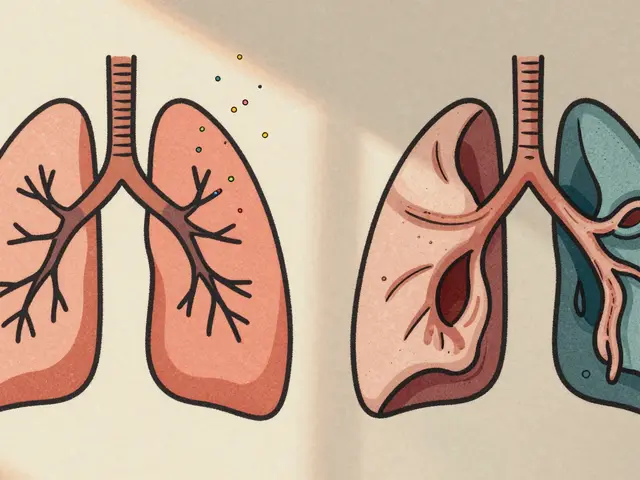
What Does Upper GI Bleeding Look Like?
You don’t need to be bleeding out to know something’s wrong. The signs are specific-and they’re hard to ignore once you’ve seen them.
- Hematemesis: Vomiting blood. Bright red means fresh bleeding. Coffee-ground vomit means the blood has been sitting in the stomach, partially digested.
- Melena: Black, sticky, foul-smelling stools. This is digested blood passing through the gut. It’s not from eating beets or iron pills-it’s a red flag.
- Hematochezia: Maroon or bright red stools. This usually means massive bleeding, where blood moves too fast to darken.
- Physical signs: Dizziness, fainting, rapid heartbeat (over 100 bpm), low blood pressure (below 90 systolic), pale skin. These mean your body is going into shock from blood loss.
One patient in a 2023 Reddit thread described waking up at 3 a.m. coughing up coffee-ground material. By the time he got to the ER, he’d lost three units of blood. He spent eight days in the hospital. That’s not unusual. Delayed care turns manageable bleeding into life-threatening collapse.
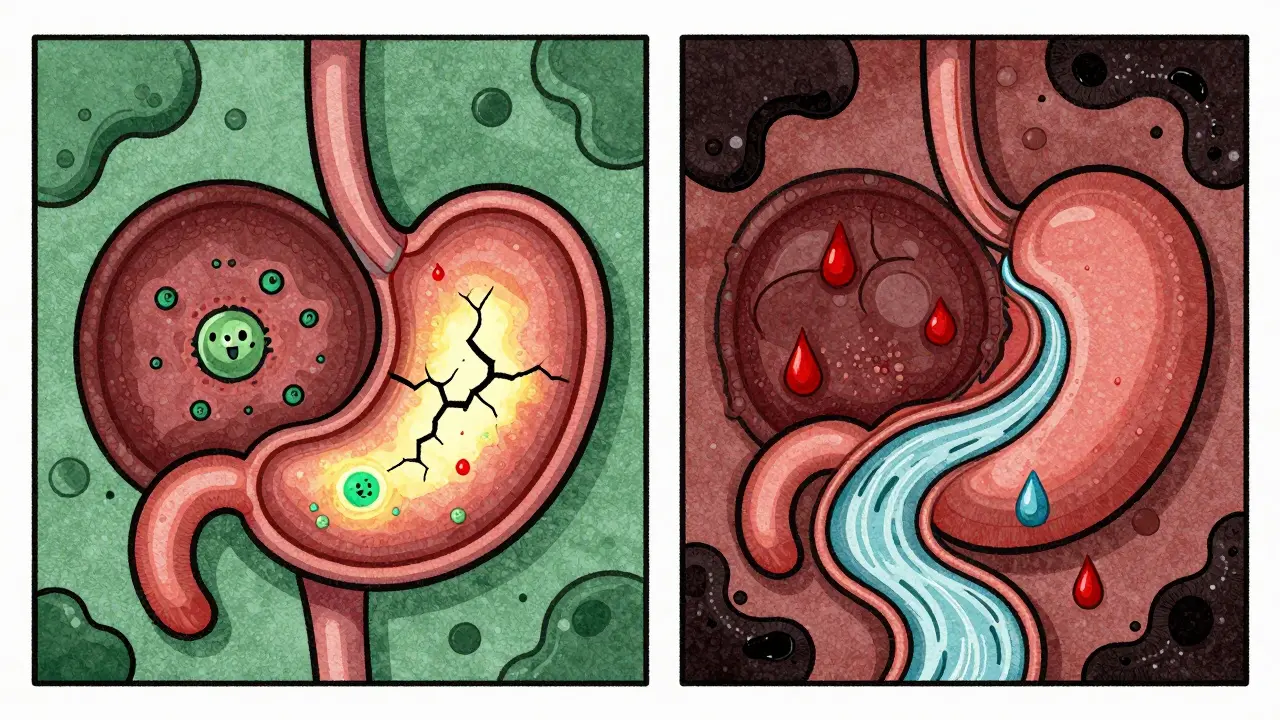
Ulcers vs. Varices: The Two Main Causes
Not all upper GI bleeding is the same. The cause changes everything-from treatment to survival odds.
Peptic ulcers (40-50% of cases) are open sores in the stomach or duodenum. Most are caused by H. pylori bacteria or long-term NSAID use (like ibuprofen or naproxen). Duodenal ulcers bleed more often than gastric ones. A bleeding ulcer doesn’t always hurt. Some people have no pain at all-just sudden weakness or black stools.
Esophageal varices (10-20% of cases) are swollen veins in the esophagus, usually from liver disease like cirrhosis. These veins are thin-walled and under high pressure. One small tear can cause massive bleeding. Mortality is high: 20% die within six weeks. Unlike ulcers, varices often bleed without warning. Patients may have no abdominal pain, just sudden vomiting of bright red blood.
Other causes? Erosive gastritis (15-20%), Mallory-Weiss tears (from violent vomiting), esophagitis, and even cancer (2-5%). And yes-SSRIs (common antidepressants) double your risk of bleeding. If you’re on one and notice black stools, don’t wait.
Stabilization: The First 30 Minutes Matter
Before you even get to endoscopy, you need to stabilize. This isn’t optional. It’s the foundation of survival.
Step one: Check vital signs. Heart rate over 100? Systolic BP under 90? That’s shock. Start IV fluids immediately. Oxygen if needed. Position the patient flat, legs elevated.
Step two: Blood tests. Hemoglobin, INR (to check clotting), and BUN-to-creatinine ratio. A ratio above 30:1 has a 69% chance of indicating upper GI bleeding. It’s not perfect, but it’s fast and cheap.
Step three: Don’t wait for endoscopy to give PPIs. For suspected ulcers, give an 80mg IV bolus of pantoprazole or omeprazole, then an 8mg/hour infusion. The COBALT trial showed this cuts rebleeding from 22.6% to 11.6%. That’s half the chance of needing another surgery or transfusion.
Step four: Transfuse only if needed. Target hemoglobin between 7 and 9 g/dL. Giving too much blood can worsen outcomes. One unit of packed red cells raises hemoglobin by about 1 g/dL. Don’t aim for normal-aim for stable.
Step five: For varices, start vasoactive drugs immediately. Terlipressin or octreotide. Add antibiotics-ceftriaxone 1g daily. This combo cuts death by 25%. Don’t delay. Every minute counts.
Diagnosis: Endoscopy Is Non-Negotiable
Lab tests and symptoms point you in the right direction. Only endoscopy confirms it.
All major guidelines agree: Get an esophagogastroduodenoscopy (EGD) within 24 hours. Better yet-within 12 hours. A 2022 study showed that doing it within 12 hours reduces death by 25% compared to waiting longer.
During the procedure, doctors use the Forrest classification to judge bleeding risk:
- Class Ia: Spurting blood. 90% chance of rebleeding without treatment.
- Class Ib: Oozing. 50% risk.
- Class IIa: Visible vessel. Also 50% risk.
- Class IIb: Adherent clot. Lower risk, but still needs treatment.
- Class III: Clean base. No active bleeding. Low risk.
For ulcers: Endoscopic therapy means epinephrine injection + either thermal coagulation or hemoclips. Success rate? 90-95%.
For varices: Band ligation is the gold standard. It cuts rebleeding from 60% to 25%. Sclerotherapy? Outdated. Less effective, more complications.
Who Can Go Home? The Glasgow-Blatchford Score
Not every person with GI bleeding needs a hospital bed. That’s where the Glasgow-Blatchford score comes in.
This scoring system uses six simple things:
- Hemoglobin (below 12.9 for men, 11.9 for women)
- Systolic blood pressure (below 100)
- Pulse rate (above 100)
- Melena
- Syncope (fainting)
- History of liver or heart disease
A score of 2 or higher? Hospitalize. A score of 0 or 1? You can probably go home safely. A 2019 study of over 3,000 patients showed this score correctly identifies 15% of patients who don’t need intervention. That saves money, reduces hospital exposure, and avoids unnecessary stress.
But here’s the catch: Don’t rely on PPIs alone to rule out bleeding. A Johns Hopkins doctor found that 30% of low-risk patients get unnecessary PPI treatment because doctors skip endoscopy. That’s dangerous. PPIs mask symptoms-they don’t fix the cause.
What’s New in 2026?
Technology is changing how we treat this.
Hemospray, an inorganic powder sprayed during endoscopy, works like a bandage over bleeding spots. It’s not for everyone-but for tricky cases where clips or bands won’t stick, it’s a game-changer. Studies show it stops bleeding in 92% of tough cases.
AI-assisted endoscopy is coming fast. A 2023 trial showed AI systems spotted bleeding signs 94.7% of the time. Human endoscopists? Only 78.3%. That’s a huge jump. But there’s a problem: AI trained mostly on white patients misses signs in Black and Hispanic patients 15% more often. Validation across diverse populations is still lagging.
And the NIH is running a massive study called UGIB-360, tracking 10,000 people to build personalized risk models using DNA, gut bacteria, and clinical data. Results won’t be out until late 2025-but when they are, we’ll finally know who’s at highest risk before they even bleed.
What Happens After?
Surviving the bleed is only half the battle.
A 2022 study found 68% of patients felt anxious about bleeding again within 30 days. Nearly half changed their diet-cutting caffeine, alcohol, spicy food. One in three stopped NSAIDs without telling their doctor. That’s risky. Stopping cold turkey can cause rebound pain or worsen arthritis. Talk to your provider.
If you had an ulcer: You’ll need H. pylori testing. If positive, antibiotics + PPI for 14 days. If you took NSAIDs, you’ll need to switch to acetaminophen or use a PPI long-term.
If you had varices: You’ll need beta-blockers (like propranolol) to lower pressure in the veins. You’ll need follow-up endoscopies every 1-2 years. And you’ll need to avoid alcohol completely.
Rebleeding? It’s common. And it’s deadly. Each rebleed raises your hospital cost by 65%. The goal isn’t just to stop the first bleed-it’s to prevent the next one.
Bottom Line
Upper GI bleeding is serious. But it’s not mysterious. Know the signs. Act fast. Get endoscopy within 12 hours. Use the Glasgow-Blatchford score to avoid overtreating. Treat ulcers with PPIs and endoscopy. Treat varices with drugs and bands. Don’t guess. Don’t wait. And don’t ignore black stools or coffee-ground vomit. They’re not normal. They’re a scream for help.
The systems that save lives now-rapid assessment, risk scoring, early endoscopy, targeted treatment-are proven. They’re not futuristic. They’re here. And they work-if you use them.







15 comments
Susie Deer
Black stools? Coffee ground vomit? That's not a suggestion to see a doctor that's a siren
TooAfraid ToSay
Wait so you're telling me if I drink too much whiskey and puke blood it's not just a bad night but a "medical emergency"? Sounds like someone got too excited about their med school textbook
Allison Deming
It is both concerning and regrettable that the public continues to conflate anecdotal experiences with clinical reality. The normalization of alarmist terminology such as "scream for help" undermines the professionalism of medical communication and fosters unnecessary panic among laypersons who may lack the contextual understanding to interpret symptoms accurately. The gravity of upper GI bleeding must be acknowledged, but the manner in which it is presented should reflect evidence-based precision rather than sensationalized dramatization.
says haze
Let’s be real - the entire medical industrial complex thrives on fear. You get black stools? You’re not bleeding, you’re just digesting your existential dread. The PPI industry is worth billions. The endoscopy machine manufacturers? They’re lobbying hard. And don’t even get me started on how they turned a physiological process into a crisis narrative. The real emergency is how we’ve outsourced our bodily intuition to algorithms and profit-driven guidelines. H. pylori? Maybe it’s just your gut saying you need to stop eating processed crap and start breathing.
Sarah -Jane Vincent
AI detects bleeding better than doctors? Sure. But did you know the AI was trained on mostly white patients? So if you're Black or Latino and you're bleeding? The AI might just say "probable beets". And the NIH's UGIB-360? That's just the government trying to track your DNA so they can raise your insurance rates. You think they care about you? They care about data points. And that "Glasgow-Blatchford score"? It's a tool to ration care. If your score is 1, they'll send you home to die quietly while they save the ICU bed for someone with better insurance. Wake up.
Anna Hunger
Thank you for this comprehensive and clinically grounded overview. The emphasis on timely endoscopy, appropriate transfusion thresholds, and risk stratification using validated scoring systems reflects best practices that have been rigorously validated in peer-reviewed literature. It is imperative that healthcare providers, regardless of setting, adhere to these protocols to optimize patient outcomes and reduce preventable mortality. The integration of emerging technologies such as Hemospray and AI-assisted endoscopy, while promising, must be implemented with rigorous validation and equitable access to ensure they serve all populations equitably.
Sarah Triphahn
People think black poop is scary? Try living with a dad who drank himself into cirrhosis and bled out on the bathroom floor while the EMTs argued about insurance. You don’t need a score to know when someone’s dying. You just need to have watched it happen too many times. Stop pretending this is about guidelines. It’s about who gets help and who gets ignored.
Dylan Livingston
Oh, so now we’re supposed to believe that coffee-ground vomit is somehow more legitimate than, say, the kind of vomiting you get after a 3 a.m. taco binge? And you want me to trust a "Forrest classification" like it’s some ancient sacred text? The truth is, most of these cases are just people who took too much ibuprofen after a party and now the medical system is cashing in. I’ve seen five people get endoscopies for "melena" - four of them were just eating too many blueberries. This isn’t medicine. It’s a revenue stream wrapped in white coats.
Andrew Freeman
they say dont wait but what if you cant afford the er? what if you dont have insurance? what if you just gotta get to work? this whole thing feels like a luxury for people who dont have to choose between rent and a ppi
Alvin Bregman
i grew up in a town where the nearest hospital was 90 minutes away. we treated stomach issues with ginger tea and prayer. i lost my uncle to something like this. no one knew what was happening until it was too late. the science here is good but the system? it leaves people behind. we need more clinics not more algorithms
Henry Sy
so you’re telling me my cousin who chugged 12 beers and woke up puking brown sludge didn’t just have a bad night but was basically one step from death? bro that’s not a medical emergency that’s a rite of passage. i’ve seen dudes pass out in the bathroom and wake up like nothing happened. you wanna save lives? stop selling fear and start teaching people how to stop being idiots with ibuprofen and whiskey
Jason Yan
I really appreciate how this breaks down the science without drowning you in jargon. It’s easy to feel overwhelmed by medical info, but when you lay out the difference between ulcers and varices like this - with clear signs, clear steps - it doesn’t just inform, it empowers. And honestly, the part about not rushing to transfuse? That’s the kind of nuance we need more of. Medicine isn’t about doing everything - it’s about doing the right thing at the right time. Thank you for that clarity.
shiv singh
you think this is about bleeding? no its about control. they want you scared so you take their pills, go to their hospitals, let them cut you open with their cameras. your body is not a machine to be fixed by white coats. listen to your gut not their guidelines. stop trusting the system that gave you high blood pressure and depression in the first place
Robert Way
did u mean to type "coffee grounds" or "coffe grounds"? also i think you misspelled "esophagus" somewhere but im not sure
Vicky Zhang
if you're reading this and you've had black stools or coffee-ground vomit - please, please, please don't wait. I've been there. I thought it was just stress. I thought I'd be fine. I wasn't. I spent three days in the ICU. My kids thought I was dying. I almost left them. This isn't fearmongering - it's love. Get help. Now. You're worth it. And your family needs you.