Proton Pump Inhibitor Prophylaxis: When and Why It’s Used
When you're seriously ill in the hospital—especially in the intensive care unit, a specialized hospital unit for patients with life-threatening conditions requiring constant monitoring—your body is under extreme stress. That stress can trigger dangerous stomach bleeding, even if you never had stomach problems before. That’s where proton pump inhibitor prophylaxis, the use of acid-reducing drugs to prevent stress-related stomach ulcers in high-risk patients comes in. It’s not for everyone, but for certain patients, skipping it can be risky. Also known as PPI prophylaxis, this practice is standard in many ICUs, emergency departments, and after major surgeries.
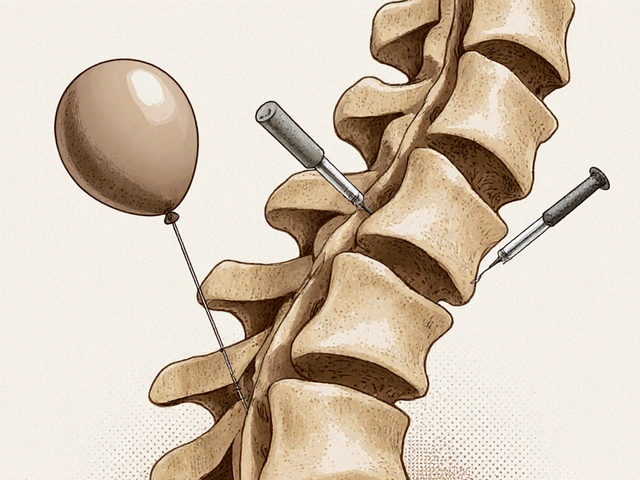
Proton pump inhibitors, or PPIs, a class of medications that block acid production in the stomach lining, are the go-to drugs here. Drugs like omeprazole, pantoprazole, and esomeprazole lower stomach acid enough to protect the stomach lining from damage caused by stress, infection, or long-term breathing tube use. But this isn’t about treating heartburn. This is about preventing something far worse: stress ulcers, deep sores in the stomach or upper intestine that can bleed dangerously in critically ill patients. Studies show that without prophylaxis, up to 15% of ICU patients on ventilators develop these ulcers—and some bleed badly enough to need transfusions or surgery. PPI prophylaxis cuts that risk by more than half.
But here’s the catch: not everyone needs it. If you’re just in the hospital for a broken leg or a routine surgery, you likely don’t need a PPI. Overuse is a real problem. Taking these drugs unnecessarily can raise your risk of pneumonia, C. diff infections, and even bone fractures over time. Doctors now follow strict guidelines: PPI prophylaxis is mostly for patients on ventilators, those with clotting disorders, those with severe burns or trauma, or anyone with multiple risk factors. It’s a targeted tool, not a blanket solution.
The posts below dive into real-world comparisons and safety concerns around medications used in similar settings—from antibiotics like chloramphenicol to sedatives that can interact with acid reducers. You’ll find clear breakdowns of how these drugs work, who they help, and when they might do more harm than good. Whether you’re a patient, caregiver, or just trying to understand hospital protocols, this collection gives you the facts without the fluff.

- Oct 24, 2025
- Posted by Cillian Osterfield
Steroids and NSAIDs: How to Lower the Massive GI Bleeding Risk
Learn why steroids and NSAIDs together dramatically raise GI bleeding risk and how to prevent it with PPIs, risk calculators, and smart drug choices.
Categories
- Health and Wellness (72)
- Medications (69)
- Health and Medicine (28)
- Pharmacy Services (12)
- Mental Health (9)
- Health and Career (2)
- Medical Research (2)
- Business and Finance (2)
- Health Information (2)
Latest Posts
©2026 heydoctor.su. All rights reserved