GI Bleeding Risk Calculator
Key Takeaways
- Combining systemic corticosteroids with non‑steroidal anti‑inflammatory drugs (NSAIDs) can raise upper GI bleeding risk up to 12‑fold.
- Risk spikes with high‑dose NSAIDs, multiple NSAID use, or added anticoagulants.
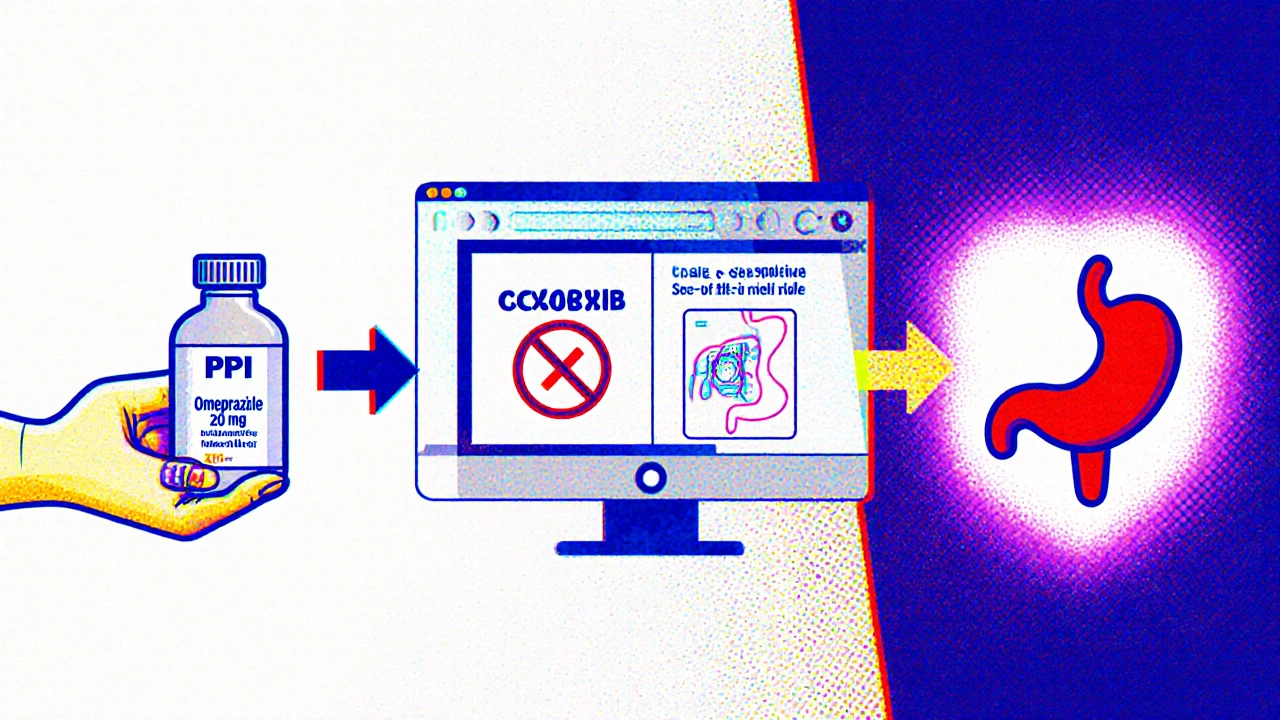
- Proton pump inhibitors (PPIs) are the preferred gastro‑protective strategy; H2‑receptor antagonists are markedly less effective.
- COX‑2‑selective NSAIDs cut bleeding events by about 50 % versus traditional NSAIDs, but they still need a PPI when steroids are on board.
- Using a validated risk calculator and automatic PPI co‑prescribing can slash preventable bleeds by two‑thirds.
When a patient ends up on both a steroid burst and an NSAID for pain, the gut pays the price. The combo doesn’t just add two risks together - it multiplies them. Below you’ll find the science behind that multiplication, the groups most likely to suffer, and a step‑by‑step plan to keep bleeding off the table.
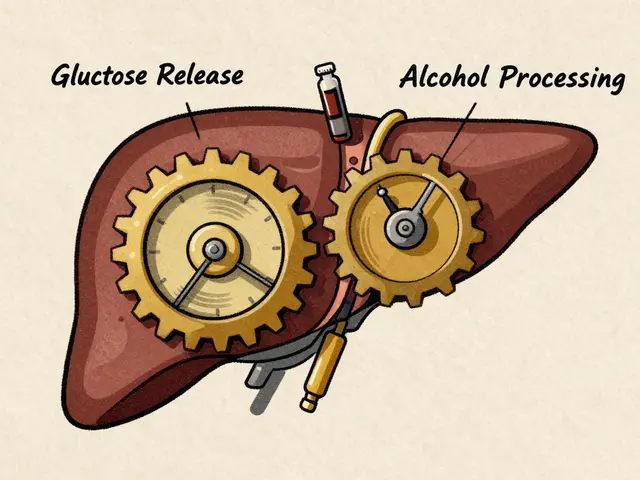
Why the Combination Is Dangerous
corticosteroids blunt the body’s natural repair processes. They curb mucus production, slow ulcer healing, and mute the pain that would otherwise signal a brewing ulcer. NSAIDs assault the stomach lining in two ways: the drug itself irritates the mucosa, and it blocks cyclooxygenase‑1 (COX‑1), cutting the prostaglandins that protect the gut.
When both drugs are present, three pathways line up:
- Reduced mucus and blood flow (NSAID effect).
- Impaired tissue repair and hidden pain (steroid effect).
- Potentially added anticoagulant exposure, which further weakens clot formation.
Large epidemiology studies from 2001 to 2014 show an odds ratio (OR) of 8.9 for upper GI bleeding when steroids and NSAIDs are used together, versus 1.8 for steroids alone. High‑dose NSAID regimens push that OR past 12.
Who Is Most at Risk?
The risk isn’t uniform. The American College of Gastroenterology (2021) lists seven red‑flag factors that push a patient into the high‑risk bucket:
- Age > 65 years.
- History of peptic ulcer or prior GI bleed.
- Concurrent anticoagulant (warfarin, DOACs).
- High‑dose or multiple NSAID use.
- Systemic corticosteroid therapy (any dose lasting > 14 days, or short bursts with high potency).
- Serious systemic disease (e.g., chronic kidney disease, liver cirrhosis).
- Smoking or alcohol excess.
Hospitalized patients carry the highest absolute rates, but even ambulatory patients with a short prednisone burst and occasional ibuprofen can develop a bleed within a week of starting the combo.
Drug‑Specific Bleeding Profiles
Not all NSAIDs are created equal. Traditional NSAIDs (tNSAIDs) such as naproxen and ibuprofen have the worst ulcer record. COX‑2‑selective agents (celecoxib, etoricoxib) lower the odds of an upper GI event by roughly 55 % but never eliminate it.
Below is a quick comparison of the most common agents.
| Drug class | Typical dose | OR for upper GI bleed (vs. no NSAID) | Effect of adding steroids |
|---|---|---|---|
| Traditional NSAIDs (naproxen, ibuprofen) | Ibuprofen ≥ 1200 mg/day | 4.0 | OR ≈ 12.7 |
| COX‑2‑selective (celecoxib) | 200 mg/day | 2.0 | OR ≈ 6.5 |
| Aspirin (low‑dose) | 81 mg/day | 1.5 | OR ≈ 4.2 |
Prevention: Gastro‑Protective Strategies
The AGA (2020) and ACG (2021) both make a crystal‑clear recommendation: any patient on a steroid‑NSAID combo should get a proton pump inhibitor (PPI) unless contraindicated.
Why PPIs over H2‑receptor antagonists (H2RAs)? Meta‑analyses show PPIs cut the ulcer risk to about a quarter of what H2RAs achieve (OR 0.27 vs 0.52). H2RAs also lose potency at night when most NSAID‑induced damage happens.
Here’s a practical algorithm most clinicians follow:
- Identify risk factors using the ACG GI Risk Calculator (age, ulcer history, anticoagulant, steroid dose, NSAID type/dose).
- Prescribe a standard‑dose PPI (omeprazole 20 mg daily) for low‑to‑moderate risk.
- Escalate to double‑dose PPI (omeprazole 40 mg daily) for high risk (previous ulcer, age > 65, concurrent anticoagulant).
- Choose a COX‑2‑selective NSAID when possible; if a traditional NSAID is required, pair it with a PPI immediately.
- Re‑assess every 4‑6 weeks; continue PPI for the entire NSAID/steroid course, not just the first few days.
For patients already on an anticoagulant, the combination of warfarin + NSAID + steroid can push the OR above 13. In those cases, a double‑dose PPI plus close INR monitoring is essential.
Real‑World Gaps and How to Close Them
Data from 2022 shows only 38 % of hospitalized patients receiving both drugs were prescribed gastro‑protection. Outside rheumatology, the rate drops to 22 %. The main culprits:
- Clinicians forgetting the steroid component when ordering an OTC NSAID.
- Electronic health records (EHR) lacking automated PPI alerts for steroid‑NSAID orders.
- Substituting H2RAs out of habit or cost concerns.
Institutions that built a “PPI‑by‑default” order set reduced bleeding events by 68 %. Simple steps you can take now:
- Add a quick‑fire note in the prescription: ‘Start PPI 20 mg daily.’
- Use the built‑in risk calculator before signing the order.
- Educate patients: tell them why a stomach‑protectant matters, even if they only need a 5‑day steroid burst.
Future Directions and Emerging Tools
Two developments are likely to reshape how we manage this risk:
- Vimovo (naproxen/esomeprazole) received FDA approval in 2023. It bundles a PPI with the NSAID, cutting endoscopic ulcers by more than half.
- Pharmacogenomic testing for CYP2C9 and PTGS1 variants may one day predict who is especially vulnerable to NSAID‑steroid GI injury, allowing truly personalized prescribing.
Until those tools are commonplace, the safest route remains systematic risk assessment and routine PPI co‑therapy.
Quick Checklist for Clinicians
- Confirm patient is on a systemic corticosteroid and an NSAID.
- Run the ACG GI Risk Calculator.
- Prescribe a PPI (standard or double dose) unless contraindicated.
- If a traditional NSAID is required, consider switching to a COX‑2‑selective agent.
- Document the indication and the gastro‑protective plan in the same medication order.
- Re‑evaluate risk every month and taper both agents when possible.
Frequently Asked Questions
Does a short‑term steroid burst still increase bleeding risk?
Yes. Studies show a measurable rise in upper GI bleeding within 7 days of starting a prednisone burst, even when the course lasts only 5 days. The risk climbs if the patient is already taking an NSAID.
Are over‑the‑counter (OTC) NSAIDs included in the risk calculation?
Absolutely. The GI risk calculator treats OTC ibuprofen, naproxen, and aspirin the same as prescription versions because the pharmacologic effect is identical.
Can H2‑receptor antagonists be used if a patient can’t take PPIs?
They’re a fallback, but evidence shows a 48 % higher ulcer rate compared with PPIs. If an H2RA is the only option, use the highest approved dose and schedule endoscopic monitoring.
What dose of PPI is considered double‑dose for protection?
For most agents, 40 mg of omeprazole (or equivalent) once daily qualifies as double dose. Some clinicians split it into 20 mg twice daily for faster acid suppression.
Should I stop the NSAID if the patient develops mild dyspepsia?
Mild dyspepsia alone isn’t a reason to stop therapy, but it should trigger a prompt endoscopic evaluation if the patient also has risk factors. Often, intensifying PPI therapy resolves symptoms.
Bottom line: the steroid‑NSAID combo is a ticking time bomb for the gut. By spotting the high‑risk patients, automatically pairing a PPI, and using COX‑2‑selective agents when appropriate, clinicians can prevent the majority of avoidable bleeds.






11 comments
junior garcia
When steroids and NSAIDs meet, it’s like a perfect storm for the gut – brace yourself!
Kester Strahan
Yo, the synergistic pharmacodynamics between glucocorticoid‑mediated mucus suppression and COX‑1 inhibition by NSAIDs creates a super‑additive OR upward of 12× – don’t overlook the PK/PD interplay.
Doreen Collins
I totally get how scary it can feel when you see those bleeding stats.
The key is to break down the risk into manageable chunks.
First, always identify if the patient is over 65 or has a prior ulcer – those are red flags.
Second, check whether they’re on an anticoagulant like warfarin or a DOAC, because that pushes the odds even higher.
Third, look at the NSAID dose; anything above 1200 mg of ibuprofen per day is considered high‑risk.
Fourth, remember that even a short burst of prednisone can blunt mucosal repair for a full week after the last dose.
Fifth, the choice of NSAID matters – COX‑2‑selective agents shave the risk roughly in half compared with traditional agents.
Sixth, the universal recommendation is to add a proton‑pump inhibitor unless there’s a clear contraindication.
Seventh, a standard‑dose PPI like omeprazole 20 mg daily is enough for low‑to‑moderate risk patients.
Eighth, for high‑risk patients, double the dose or split it twice daily for more robust acid suppression.
Ninth, education is crucial – tell patients that even over‑the‑counter ibuprofen needs a stomach protector when combined with steroids.
Tenth, use the ACG GI risk calculator before signing the order to make sure you’re not missing any hidden factors.
Eleventh, if your EHR supports it, set up an automatic “PPI‑by‑default” order set to close the gap.
Twelfth, follow‑up endoscopically if any dyspeptic symptoms arise in a high‑risk individual.
Finally, keep reassessing every few weeks and taper both drugs as soon as clinically feasible to eliminate the lingering danger.
HILDA GONZALEZ SARAVIA
Great points – just remember to run the ACG calculator, double‑check the NSAID dose, and then auto‑prescribe a PPI; that workflow alone cuts preventable bleeds dramatically.
Amanda Vallery
Just add a PPI – it’s that simple.
Marilyn Pientka
While simplicity is appealing, the evidence shows that a standard‑dose PPI may be insufficient for high‑risk cohorts; you need a double‑dose regimen.
Moreover, substituting H2‑RAs simply to save cost is a negligent practice that jeopardizes patient safety.
In academic medicine we must adhere to guideline‑driven prophylaxis, not cut corners for convenience.
Jordan Levine
Steroid‑NSAID combos are a GI nightmare 😂
Carla Taylor
Totally agree keep the PPI on board it saves lives
Kathryn Rude
One might argue that the medical establishment has long ignored the subtle art of gastro‑protection, preferring to rely on patient compliance as a crutch :/.
Yet the data are unambiguous – without a PPI, the steroid‑NSAID duet becomes lethal in a matter of days.
Let us not be complacent; let us demand that every prescription be accompanied by a protective agent.
The moral imperative is clear, and the cost of inaction is measured in blood loss.
Lindy Hadebe
The statistics speak for themselves – bleed risk skyrockets.
Implementing automatic alerts is a pragmatic solution.
Ekeh Lynda
From a systems‑level perspective, the failure to embed gastro‑protective protocols within electronic order sets reflects a deeper governance lapse.
When clinicians are forced to remember a secondary medication amidst a barrage of alerts, the likelihood of omission rises exponentially.
Moreover, the heterogeneity of OTC NSAID consumption patterns complicates risk stratification, necessitating patient‑centered education initiatives.
In low‑resource settings, the cost differential between PPIs and H2‑RAs may drive suboptimal prescribing, yet generic PPIs are widely available and should be the default.
Future research should focus on real‑world effectiveness of bundled therapies like Vimovo versus isolated PPI co‑prescribing.
Until such data mature, the safest bet remains a disciplined, algorithm‑driven approach that flags every steroid‑NSAID pairing for prophylaxis.