Multicultural Healthcare: Bridging Cultural Gaps in Medication Safety and Treatment
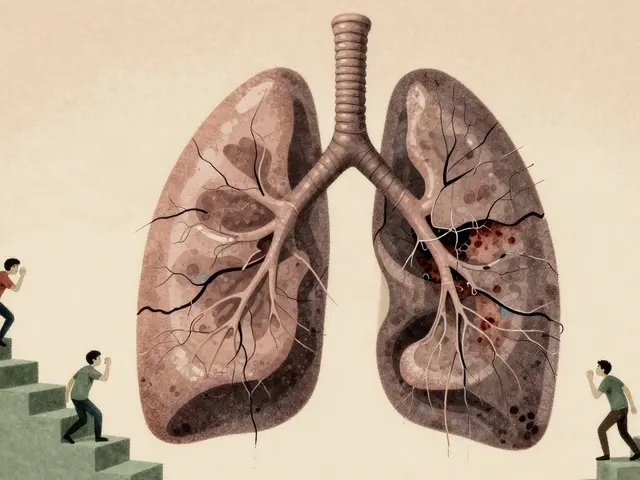
When we talk about multicultural healthcare, the practice of delivering medical care that respects and responds to the cultural, linguistic, and social needs of diverse patient populations. Also known as culturally competent care, it’s not optional—it’s essential for safety, effectiveness, and trust. A patient from Mexico may avoid insulin because they believe it’s a "Western cure" that disrupts natural balance. A Somali elder might skip blood pressure pills after hearing a neighbor say they caused kidney damage. These aren’t just misunderstandings—they’re life-threatening gaps in care.
Language barriers, the challenge of communicating medical information when patient and provider don’t share a common language directly impact medication safety. Studies show patients with limited English proficiency are 30% more likely to have adverse drug events. But it’s not just about translators. It’s about whether the pharmacist explains "take once daily" in a way that fits the patient’s daily rhythm—whether they work nights, pray five times a day, or rely on family to manage pills. Medication adherence, how consistently a patient takes their medicine as prescribed drops sharply when instructions feel foreign, confusing, or disrespectful. A Vietnamese woman might hide her warfarin because her grandmother warned that blood thinners cause "cold blood"—a belief tied to traditional yin-yang balance. Without understanding that, you’re just giving pills, not care.
Health disparities, differences in health outcomes tied to race, ethnicity, immigration status, or socioeconomic background aren’t random. They’re built into systems. A Black patient with diabetes is more likely to be prescribed metformin, but less likely to get a continuous glucose monitor—even when they qualify. Why? Bias in referral patterns, lack of trust from past mistreatment, or clinics that don’t offer culturally tailored education. Meanwhile, a South Asian patient on azathioprine for lupus might stop taking it because they don’t understand why they need it for years when they feel fine—something their doctor never explained in terms they connected with.
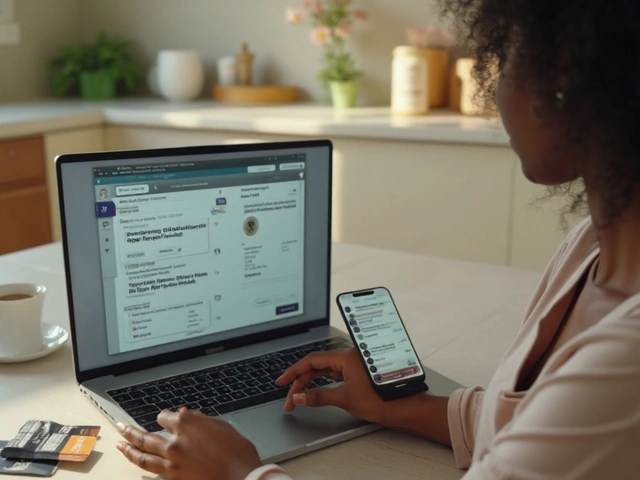
Good multicultural healthcare doesn’t mean memorizing every cultural belief. It means asking: "What do you believe about this medicine?" and listening. It means using community health workers who speak the same language and share the same values. It means knowing that for some, the pharmacy isn’t just a place to pick up pills—it’s a place where they’ve been ignored, rushed, or judged. The posts below show how these real-world issues play out: how warfarin interacts with herbal teas some use for spiritual cleansing, how refill labels confuse non-native speakers, how older adults from different cultures interpret side effects like dizziness or fatigue. You’ll see how stigma, tradition, and mistrust shape whether a treatment works—or fails.

- Dec 1, 2025
- Posted by Cillian Osterfield
Multicultural Perspectives on Generics: How Culture Affects Patient Trust and Adherence
Cultural beliefs about pill appearance, ingredients, and trust shape how patients use generic medications. Learn why color, gelatin, and language matter-and how healthcare providers can improve adherence across diverse communities.
Categories
- Health and Wellness (72)
- Medications (70)
- Health and Medicine (28)
- Pharmacy Services (12)
- Mental Health (9)
- Health and Career (2)
- Medical Research (2)
- Business and Finance (2)
- Health Information (2)
©2026 heydoctor.su. All rights reserved