When your gut feels off-bloating after a light meal, gas that won’t quit, diarrhea or constipation that comes and goes-you might blame stress, food sensitivities, or just bad luck. But for millions of people, the real culprit is something hidden in plain sight: Small Intestinal Bacterial Overgrowth, or SIBO. It’s not a buzzword. It’s a real, measurable condition where bacteria that belong in the large intestine creep into the small intestine and start causing chaos.
What Exactly Is SIBO?
Your small intestine is meant to be mostly clean. It’s where nutrients get absorbed, not where bacteria hang out. Normally, only a few thousand bacteria per milliliter live there. In SIBO, that number jumps to over 100,000. That’s not just a little extra. That’s a full-blown microbial invasion.It happens when the natural defenses break down. Your stomach acid, which kills most swallowed bacteria, gets turned down by long-term use of acid blockers like omeprazole. Your gut moves too slowly-common in diabetes, Parkinson’s, or after abdominal surgery. Or you’ve had a bowel obstruction, a hernia, or even just years of poor motility. The result? Bacteria multiply where they shouldn’t, fermenting carbs into gas, damaging the gut lining, and stealing nutrients you need.
It’s not rare. Studies show up to 85% of people diagnosed with IBS actually have SIBO. And while it’s often dismissed as "just IBS," the treatment is completely different. Get the diagnosis right, and relief can be dramatic.
How Do You Know If You Have It?
You can’t see SIBO on a scan. Blood tests won’t catch it. The only practical way to test is through a breath test. There are two main types: the glucose breath test and the lactulose breath test.The glucose test uses 10 grams of glucose dissolved in water. Glucose is absorbed quickly in the first part of the small intestine. So if you’re producing hydrogen or methane gas within 90 minutes, it likely means bacteria are already there-fermenting the sugar before it can be absorbed. This test is more specific-about 83% accurate-but misses a lot of cases because it only detects overgrowth in the upper small intestine.
The lactulose test uses a sugar your body can’t digest. It travels further down the small intestine before bacteria break it down. That means it can detect overgrowth deeper in the gut. But it’s less specific. Some people with fast digestion will show a false positive because the sugar zips through too quickly. The sensitivity? Around 62%. That’s why many clinics run both tests.
A positive result? A rise of 20 parts per million (ppm) in hydrogen, or 10 ppm in methane, within two hours. Methane is especially important. It’s linked to constipation-predominant symptoms, and it’s harder to treat. About 30-40% of SIBO patients produce methane instead of-or in addition to-hydrogen.
But here’s the catch: breath tests aren’t perfect. About 15-20% of people don’t produce hydrogen at all. They’re "non-hydrogen producers," and their SIBO might go undetected. That’s why labs now test for methane too. And even then, false positives happen. If you ate fiber the day before, took antibiotics recently, or didn’t fast long enough, your results could be wrong.

What Does a Breath Test Really Tell You?
A breath test doesn’t tell you which bacteria are overgrown. It doesn’t tell you if they’re resistant to antibiotics. It doesn’t tell you why the overgrowth happened in the first place. It just tells you that gas is being made where it shouldn’t be.That’s why some doctors, like Dr. Hisham Hussan at UC Davis Health, argue breath tests alone aren’t enough. He says up to 40% of SIBO diagnoses based on breath tests are wrong. His team uses endoscopy to collect fluid directly from the small intestine and culture the bacteria. That’s the old gold standard-counting colony-forming units (CFU/mL). If it’s over 10^5, you’ve got SIBO.
But endoscopy is expensive, invasive, and not widely available. It costs 10 times more than a breath test. Most insurance won’t cover it unless everything else fails. So for now, breath tests are the default. They’re the best tool we have for screening, even if they’re not perfect.
Experts like Dr. Mark Pimentel say breath tests are "the most practical diagnostic tool." Dr. Eamonn Quigley, former president of the American College of Gastroenterology, says they’re better as a screening tool than a definitive diagnosis. The truth? They’re a starting point. Your symptoms, your history, your response to treatment-they all matter more than a single number on a graph.
How Is SIBO Treated?
Once you have a positive test, treatment is straightforward-but not always simple. The first-line antibiotic is rifaximin, taken at 1,200 mg per day for 10 to 14 days. It’s not absorbed into the bloodstream. It stays in the gut, killing bacteria without wrecking your whole microbiome.Studies show 40-65% of people improve after one round. But here’s the problem: over 40% come back within nine months. Why? Because antibiotics don’t fix the root cause. If your gut motility is slow, your stomach acid is low, or you’ve got a structural issue, the bacteria will return.
For methane-dominant SIBO, rifaximin alone often isn’t enough. You need a combo: rifaximin plus neomycin. That combination improves outcomes significantly. Some doctors also use metronidazole or herbal antibiotics like oregano oil, berberine, or allicin. Herbal protocols can be just as effective as antibiotics, with fewer side effects-and they’re popular among patients who want to avoid pharmaceuticals.
But antibiotics aren’t the whole story. After treatment, you need to keep the bacteria from coming back. That means:
- Fixing motility issues with prokinetics like low-dose naltrexone or prucalopride
- Reducing acid blockers if possible
- Following a low-FODMAP or SIBO-specific diet for a few months
- Supporting stomach acid with betaine HCl if it’s low
- Rebuilding the gut lining with nutrients like L-glutamine
Some people need long-term, low-dose antibiotics or periodic herbal rounds. Others get lucky and never have another flare. It depends on what caused it in the first place.
Why Do So Many People Keep Getting SIBO?
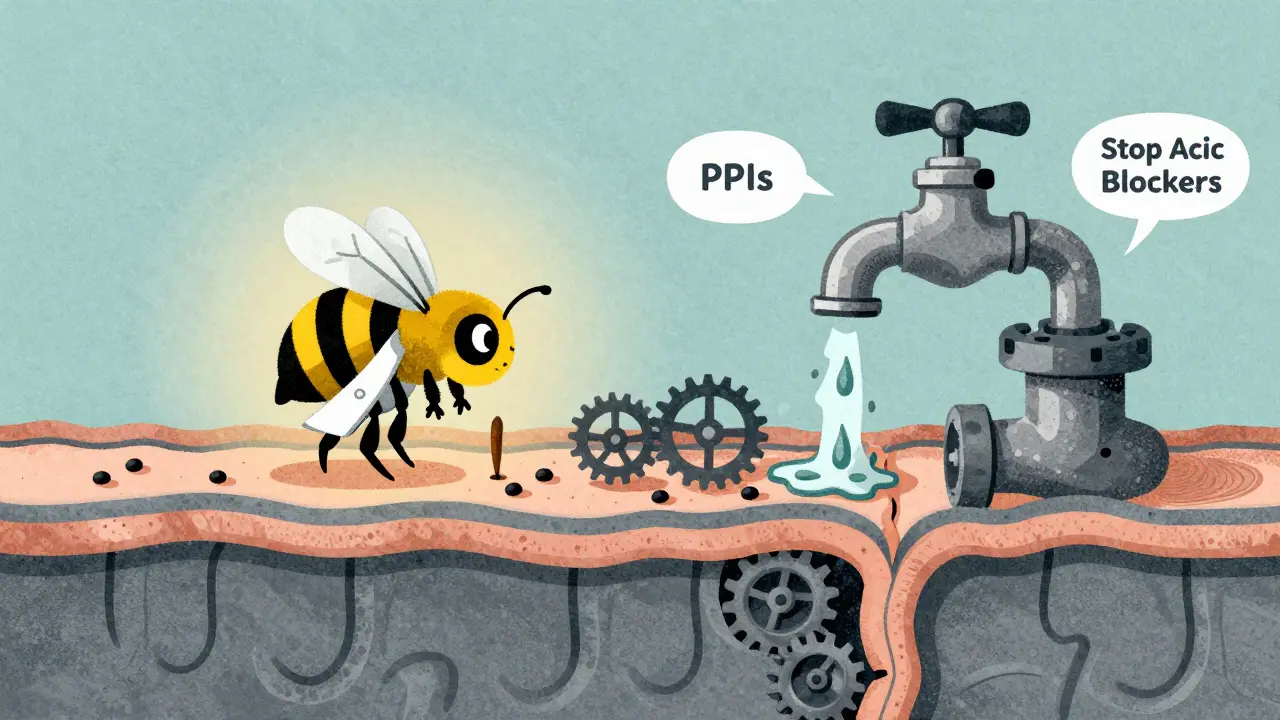
Because most treatment plans ignore the "why." If you treat the overgrowth but don’t fix the cause, it’s like mopping up water while the faucet is still running.Think about this: 30-50% of post-surgery patients develop SIBO. Why? Scar tissue, adhesions, or altered anatomy slow down the gut’s natural cleaning waves. If you had gastric bypass, ileostomy, or even a gallbladder removal, your risk goes up.
Proton pump inhibitors (PPIs)-the common heartburn meds-double or triple your risk. They kill stomach acid, which is your first line of defense against bacteria. A 2017 JAMA study found a clear link between long-term PPI use and SIBO.
And let’s not forget IBS. The overlap is massive. In fact, many people are diagnosed with IBS for years before someone finally tests them for SIBO. Once they treat the SIBO, their "IBS" symptoms vanish.
That’s why the best outcomes happen when treatment is personalized. A 60-year-old woman with hypothyroidism and chronic constipation needs a different plan than a 30-year-old man with post-infectious IBS after food poisoning. One might need prokinetics and dietary changes. The other might need a single antibiotic course and a gut-healing protocol.
What’s Next for SIBO Testing and Treatment?
The field is changing fast. Researchers at Cedars-Sinai and Mayo Clinic are working on next-gen breath analyzers that can detect multiple gases at once with higher accuracy. One new device, currently in phase 2 trials, claims 85% accuracy-far better than today’s tools.There’s also interest in stool DNA tests that could identify specific bacterial strains, and even intraluminal gas sensors that measure gas directly inside the gut. These aren’t available yet, but they’re coming.
Meanwhile, the market is booming. The global SIBO diagnostics market is expected to hit $310 million by 2028. Companies like Genova Diagnostics and Quest Diagnostics are rolling out standardized tests. But here’s the problem: no one regulates how results are interpreted. One lab says 10 ppm hydrogen is positive. Another says 20 ppm. That’s why two people with the same symptoms can get opposite diagnoses.
The bottom line? Breath tests are the best tool we have right now-but they’re not foolproof. Treat the person, not just the test. And if you’ve been told you have "IBS" and nothing helps, ask for a breath test. It could change everything.







11 comments
John Pope
Okay but let’s be real-SIBO isn’t even a real diagnosis, it’s just Big Pharma’s way of selling you $200 breath tests and antibiotics you don’t need. I’ve had ‘IBS’ for 12 years, tried everything, and the only thing that fixed me was cutting out gluten and doing yoga. Breath tests? More like guess tests. They’re measuring gas like it’s a weather report. 🤡
Priyanka Kumari
This is one of the clearest explanations of SIBO I’ve ever read. The breakdown of glucose vs. lactulose tests is especially helpful. I’ve seen so many patients misdiagnosed as IBS when they actually had methane-dominant SIBO-constipation, bloating, and zero relief from fiber. The key is treating the root cause, not just the gas. Prokinetics + dietary changes + targeted antimicrobials = real healing.
Nelly Oruko
So… breath tests are kinda like a smoke alarm that goes off when you burn toast. It tells you something’s wrong, but not if it’s a fire or just bad toast. And nobody’s fixing the toaster.
vishnu priyanka
Man, I had this after my appendix surgery back in 2018. No one believed me until I did the lactulose test. Methane levels were through the roof. Took 3 rounds of herbal stuff-oregano, berberine, garlic extract-and now I eat kimchi like it’s candy. Gut’s a jungle, but it’s my jungle now.
Angel Tiestos lopez
Bro. I did the breath test. Hydrogen spiked like a rocket. Took rifaximin. Felt like a new person. Then I ate a damn avocado and it was back. 😭 Now I’m on low-FODMAP, taking naltrexone at night, and drinking bone broth like it’s water. It’s a lifestyle now. Not a cure. But hey, I can eat dinner without feeling like a balloon. 🙏
Alan Lin
The clinical negligence here is staggering. Breath tests are being used as definitive diagnostics despite 40% false-positive rates. This is not medicine-it’s algorithmic guesswork masquerading as science. If you’re not using endoscopic aspirate cultures as the gold standard, you’re not treating patients-you’re gambling with their health. Insurance companies are complicit. This is a systemic failure.
Trevor Whipple
lol breath tests are trash. I did one and they said I had SIBO. I didn’t even have symptoms. Probably just ate a burrito the day before. Also, why are people taking antibiotics for gas? Sounds like a scam. My grandma had bloating and she just drank peppermint tea. Problem solved. 💅
Lethabo Phalafala
I’ve been through this hell. Four years of doctors telling me it was anxiety. Four. Years. Then I found a functional doc who did the lactulose test-methane positive. I cried when I read the results. Not because I had SIBO, but because someone finally saw me. Rifaximin + prucalopride + no dairy = I can now go to a birthday party without hiding in the bathroom. This isn’t just medicine. It’s liberation.
Lance Nickie
So SIBO’s real? Cool. So’s ghosts. Show me the bacteria under a microscope. Not a gas spike. Not a graph. Actual bugs. Otherwise it’s just fancy IBS.
Milla Masliy
As someone from a culture where fermented foods are daily staples-kimchi, idli, kefir-I find it wild that we’re treating gut bacteria like invaders. Maybe it’s not about eradicating them, but restoring balance. I tried the low-FODMAP diet for 3 months. Felt like I was eating cardboard. Then I added back small amounts of garlic and onions slowly-my gut adapted. No antibiotics needed. Sometimes the body just needs time and trust.
sam abas
Look, I get it. Breath tests are convenient. But here’s the thing nobody wants to admit: the whole SIBO industry is built on a foundation of shaky science and marketing. The diagnostic criteria vary wildly between labs. One says 20 ppm hydrogen is positive, another says 12. One uses glucose, another lactulose, another does both. And then they slap a $400 price tag on it. Meanwhile, the real issue-motility, vagus nerve dysfunction, bile acid malabsorption-is ignored. You treat the symptom, not the cause. And then you wonder why 70% of people relapse. It’s not SIBO that’s the problem. It’s the system that’s broken. And now we’ve got venture capitalists funding breath test startups because ‘gut health’ is the new wellness goldmine. Wake up. This isn’t medicine. It’s a business model dressed in lab coats.