Pharmacies lose up to $15,000 yearly from unused medications due to poor inventory management. medication budgeting systems and auto-refill alerts prevent this by tracking costs and automating refills. Here's how to set them up.
Understand What Medication Budgeting and Auto-Refill Alerts Do
Medication budgeting systems are structured financial planning frameworks that help healthcare institutions track pharmaceutical expenditures and optimize drug costs. These systems, along with Auto-Refill Alerts, automate prescription renewals and prevent stockouts, ensuring patients receive timely medication. Without these tools, pharmacies risk overspending, facing shortages, or wasting money on expired drugs.
Step 1: Assess Your Current Medication Costs
Start by tracking every medication cost. The ASHP Guidelines state that this means recording both ongoing expenses and inventory assets. Brigham and Women's Hospital reduced costs by 12.3% in three years by breaking down drug costs into categories like infusions, outpatient, and inpatient drugs. This step is critical because you can't manage what you don't measure. U.S. hospital drug expenditures grew from $37.5 billion in 2009 to $128.2 billion in 2021, a 242% increase. Without proper budgeting, pharmacies risk overspending.
Step 2: Choose the Right System for Your Pharmacy
Your pharmacy's existing infrastructure matters. Most systems integrate with Electronic Health Records (EHRs) like Epic or Cerner. Epic handles 32% of hospital EHRs in the U.S., while Cerner covers 28%. Check compatibility with your current setup. ASHP recommends systems with HL7/FHIR Interfaces for smooth data exchange. For example, Omnicell and Pyxis pharmacy systems work well with most EHRs. Avoid standalone tools that can't sync with your inventory database.
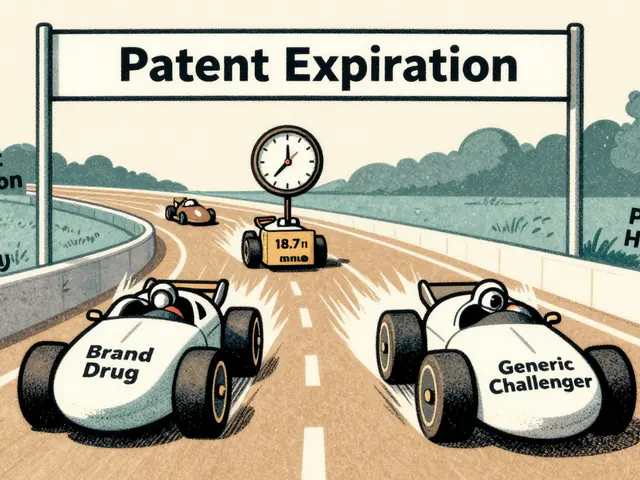
| Approach | Best For | Cost Savings | Implementation Time |
|---|---|---|---|
| Traditional Annual Budgeting | Stable environments with predictable drug usage | 8-10% | 3-6 months |
| Rolling Forecasts | Volatile periods like pandemics | 15-20% more accurate projections | 4-8 months |
| Zero-Based Budgeting | Long-term cost reduction | 15-18% | 6-12 months |

Step 3: Configure the Budgeting Module
Once installed, set up your budgeting module. Track drug utilization line by line. Dr. Sarah Churchill, Pharmacy Director at Brigham & Women's Hospital, advises 'carving out infusion drugs, operating room drugs, inpatient drugs, and outpatient take-home drugs' for precise budgeting. This helps spot where costs are rising. For instance, if a new antibiotic is used more than expected, adjust your budget before it's too late. The system should collect Drug Utilization Data from EHRs and pharmacy records. This data drives decisions, like whether to switch to generic alternatives when prices rise.
Step 4: Set Up Auto-Refill Alerts
Configure alerts to trigger when inventory drops below a set threshold. University HealthSystem Consortium data shows enterprise systems reduce stockouts by 27% compared to basic systems. Set alerts for 7-day supply to prevent shortages. For example, Johns Hopkins Hospital saved $1.2 million yearly by auto-refilling when stock hit 7 days' worth. Make sure alerts integrate with your pharmacy's workflow so staff get notifications without extra steps. Systems like Vizient offer real-time benchmarking against UHC data, helping pharmacies adjust refill schedules based on actual usage patterns.
Step 5: Train Your Team
Training takes 4-8 weeks. Syntellis reports 82% of organizations provide vendor-led training averaging 40 hours per super user. Teach staff how to read variance reports. Common mistakes include ignoring alerts or misinterpreting data. For example, a pharmacy in Ohio wasted $20,000 on expired drugs because staff didn't check alerts for seasonal medications. Regular training sessions prevent these errors. Ensure your team understands how to use the system daily. As Dr. John Murphy, ASHP Policy Director, says, 'Effective budgeting requires starting early with staff engagement and monthly performance assessments.'
Step 6: Monitor and Adjust Your Budget
Review monthly variance reports. ASHP guidelines recommend monthly performance assessments. If your budget shows a 10% overspend on a specific drug, investigate why. Maybe a new supplier has higher prices, or usage spiked. Adjust the budget accordingly. For instance, when drug prices rose 15% due to inflation, a clinic in Texas reduced costs by switching to generic alternatives. Continuous monitoring keeps your budget on track. Systems like Red Book and Medi-Span provide real-time drug pricing data, helping you stay ahead of cost changes.
Common Pitfalls and How to Avoid Them
Many pharmacies fail because they rely too much on historical data. David Johnson, a healthcare finance expert, warns that 'over-reliance on historical data during rapid drug price inflation' caused 78% of hospital formularies to overspend in 2022. Also, budgets disconnected from clinical workflows cause resistance. A 2023 study found 63% of physicians ignore budget constraints when not integrated into order entry systems. Always align your budget with real-time clinical needs. For example, if a new treatment protocol increases drug use, update your budget immediately instead of waiting for next year's plan.
Frequently Asked Questions
How long does it take to implement a medication budgeting system?
Implementation typically takes 3-6 months. This includes 8-12 weeks for data collection, 6-10 weeks for system configuration, 4-8 weeks for staff training, and 4-12 weeks for go-live support. Brigham & Women's Hospital required 14 FTE weeks for pharmacy staff and 8 FTE weeks for finance personnel during their 2022 implementation.
What's the cost of a medication budgeting system?
Implementation costs vary. Enterprise systems like Epic or Cerner average $285,000, while mid-tier solutions cost around $185,000. Annual maintenance fees are typically 15-20% of the initial cost. However, most pharmacies see a return on investment within 12-18 months due to cost savings from reduced waste and optimized purchasing.
Can small pharmacies use these systems?
Yes, but they may need simpler solutions. Community hospitals with under 200 beds often use rolling forecast systems instead of zero-based budgeting. Standalone tools like StrataJazz offer affordable options for small pharmacies. However, integration with EHRs is still necessary. Many vendors provide scalable plans that start basic and add features as your pharmacy grows.
How do auto-refill alerts prevent stockouts?
Auto-refill alerts trigger when inventory drops below a set threshold, usually 7 days' supply. This ensures orders are placed before stock runs out. For example, Johns Hopkins Hospital reduced stockouts by 27% using enterprise systems that monitor real-time inventory levels. Alerts also account for seasonal demand, like flu season, adjusting refill schedules automatically.
What data does a medication budgeting system track?
The system tracks drug purchase data, utilization data, workload metrics, and financial statements. It monitors costs for specific drug categories like infusions or outpatient drugs. For instance, a system might flag a 20% increase in opioid prescriptions, prompting a review of prescribing patterns. Data sources include EHRs, pharmacy inventory logs, and supplier invoices.






15 comments
lance black
Get the system. Save money. Do it now.
Albert Lua
This is awesome! Let's get everyone on board. We need to share best practices.
Katharine Meiler
Integrating HL7/FHIR interfaces ensures seamless data flow. Critical for accurate budgeting.
Rene Krikhaar
This helps pharmacies save money just set up alerts and monitor works well
Samantha Beye
Good steps outlined. Training is key. Staff need to understand the system.
Johanna Pan
This is really helpful. But make sure to track all costs. Dont forget to check for expired drugs.
Gregory Rodriguez
Wow, finally someone got it right. Or maybe not. This system is just another way to make us jump through hoops. But hey, saving $15k is nice.
Bella Cullen
Meh.
Cole Streeper
This is all part of the government's plan to control our meds. We need to fight back!
Dina Santorelli
Jargon-heavy nonsense. Who has time for this? Just another way for big pharma to suck us dry.
divya shetty
In India, we have better systems. This is just a Western approach that won't work here.
Nancy Maneely
OMG, this is gonna save us billions! But wait, is it really? I don't trust it.
Phoebe Norman
Drug utilization data from EHRs critical for budgeting monitor variances monthly
Matthew Morales
This is 🔥!
Diana Phe
This is a ploy to make us dependent on foreign meds. We need to build our own systems.