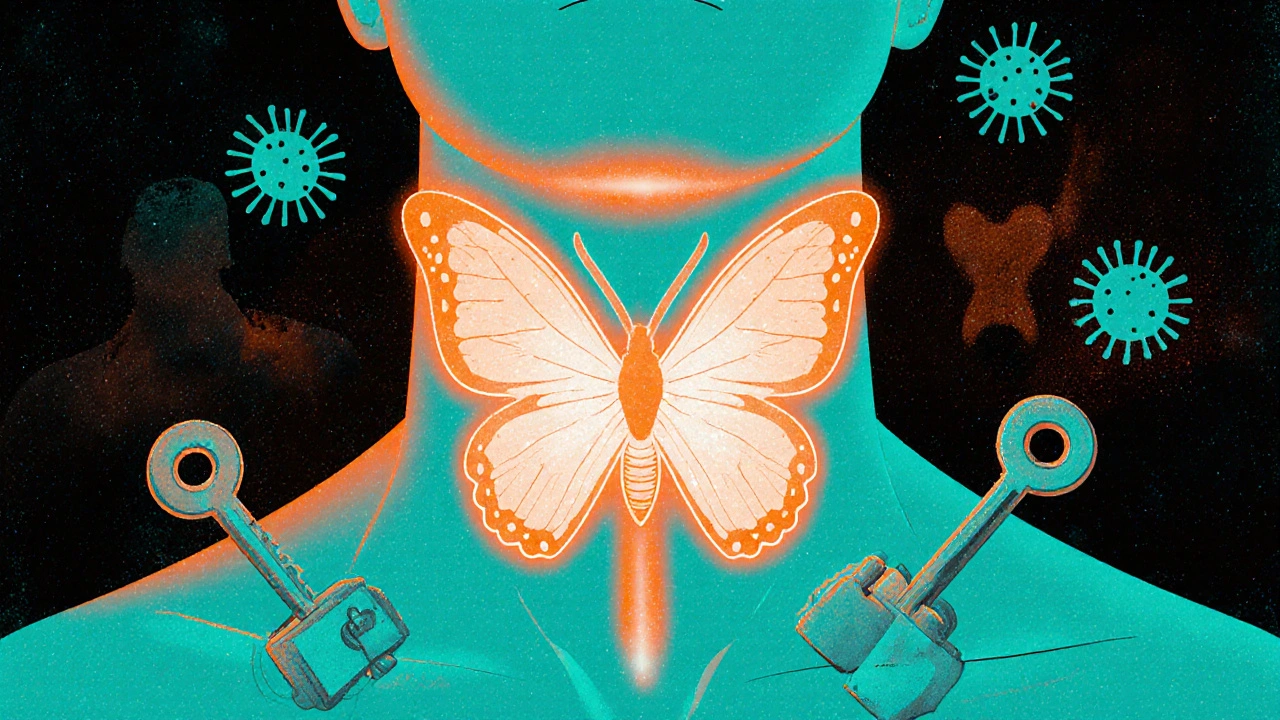
Graves' disease isn't just an overactive thyroid. It's your immune system turning against you. Instead of protecting your body, it sends out rogue antibodies that trick your thyroid into producing too much hormone. This isn't a minor glitch-it’s a full-blown malfunction that can wreck your energy, your heart, your eyes, and even your pregnancy. About 80% of all hyperthyroidism cases are caused by Graves' disease, making it the most common reason your thyroid goes haywire. And while it can strike anyone, it’s far more likely in women-seven times more likely-especially between the ages of 30 and 50.
What Happens When Your Immune System Attacks Your Thyroid
Your thyroid is a small butterfly-shaped gland in your neck. It controls how fast your body uses energy, how you feel, even how your heart beats. In Graves' disease, your immune system makes something called thyroid-stimulating immunoglobulins (TSI). These antibodies latch onto your thyroid like keys in a lock, forcing it to churn out way more thyroid hormone than your body needs. The result? Your metabolism goes into overdrive.
That means you might lose weight even when you’re eating more. Your heart races. You can’t sleep. Your hands shake. You feel anxious, hot, and exhausted all at once. These aren’t just "stress symptoms." They’re biological signals your body is drowning in thyroid hormone. Blood tests will show TSH (the brain’s signal to slow down the thyroid) crushed below 0.4 mIU/L, while free T4 and T3 levels soar above normal-often above 1.8 ng/dL and 4.2 pg/mL respectively.
But Graves’ doesn’t stop at the thyroid. About half of people with the disease develop eye problems-Graves’ ophthalmopathy. Eyes bulge. They feel gritty, painful, or swollen. In 3 to 5% of cases, vision is at risk because the optic nerve gets squeezed. A smaller number get skin changes on their shins-thick, red, bumpy patches called pretibial myxedema. These aren’t random side effects. They’re direct results of the same autoimmune attack hitting tissues around the eyes and skin.
Why PTU Is Still Used Despite the Risks
There are three main ways to treat Graves’ disease: drugs, radioactive iodine, or surgery. Antithyroid medications are usually the first step. Two drugs are used: methimazole and propylthiouracil (PTU). Methimazole is the go-to for most adults. It’s taken once a day, works well, and has fewer serious side effects.
So why use PTU at all?
Because in the first three months of pregnancy, methimazole can cause rare but serious birth defects. PTU crosses the placenta less and carries a lower risk to the baby. For that reason, it’s the drug of choice during early pregnancy-even though it comes with its own danger: liver damage. About 1 in 500 people on PTU develop severe liver injury. That’s rare, but it’s real. The FDA requires a black box warning on PTU for this reason. Doctors monitor liver enzymes monthly in patients taking it. If you get yellow skin, dark urine, or feel nauseous, stop it immediately and call your doctor.
PTU also works faster than methimazole. In thyroid storm-a life-threatening surge of thyroid hormone that can kill 20 to 30% of people if untreated-PTU is often the first-line drug because it blocks hormone production and stops new hormone from being released from the gland. That dual action can be lifesaving.
Still, for non-pregnant adults, methimazole is preferred. PTU is reserved for first-trimester pregnancy, severe disease, or thyroid storm. Most patients take it three times a day, starting at 100 to 150 mg per dose. Doses can go up to 600-800 mg daily in extreme cases. It’s not a cure-it’s a bridge. You take it for 12 to 18 months and hope your immune system calms down.
What Happens When the Drugs Don’t Work
One in two people with Graves’ disease eventually go into remission after 12 to 18 months of antithyroid drugs. That means their thyroid returns to normal without needing more medication. But the flip side? Half of them come back. Relapse rates hit 40 to 60% within a year of stopping treatment. That’s why many patients end up choosing definitive treatments: radioactive iodine or surgery.
Radioactive iodine (I-131) is swallowed as a pill. It’s absorbed by the thyroid and destroys the overactive cells. In 80 to 90% of cases, one dose cures the hyperthyroidism. But there’s a catch: you’ll likely become permanently hypothyroid. That means you’ll need to take thyroid hormone replacement for the rest of your life. It’s predictable. It’s manageable. But it’s lifelong.
Surgery-removing most or all of the thyroid-is the fastest way to fix the problem. It works in 95% of cases. But it’s invasive. Risks include damage to the nerves controlling your voice (1% chance of hoarseness) or the parathyroid glands (1-2% chance of low calcium). You’ll need lifelong hormone replacement too.
Cost-wise, antithyroid drugs run $10 to $50 a month. Radioactive iodine costs $300 to $1,500. Surgery? $5,000 to $15,000. Insurance usually covers all three, but the long-term cost of lifelong hormone replacement adds up.
The Hidden Struggles: Eye Disease and Mental Health
Most people don’t talk about the eyes. But if you have Graves’ disease, you’re 50% more likely to have bulging eyes, dryness, double vision, or pain. In severe cases, you need more than thyroid meds. You need an ophthalmologist. Treatments include steroids, orbital radiation, or even surgery to decompress the eye socket. The drug teprotumumab, approved in 2021, can reduce eye bulging by 70% in clinical trials-but it costs $150,000 per course. Most patients can’t access it without insurance approval.
And then there’s the mental toll. A 2023 survey of over 1,200 patients found that 78% struggled with severe anxiety and insomnia before diagnosis. Many were misdiagnosed with panic disorder or menopause. One Reddit user wrote: "I went to six doctors before someone said, ‘Your thyroid is off.’ I thought I was losing my mind." Weight loss, tremors, and heart palpitations are physical-but the fear, the fatigue, the brain fog? Those are real too.
Patients on PTU report extra stress from monthly blood tests. One woman shared: "I had ALT levels hit 120 when they should’ve been under 40. I cried in the parking lot after the lab. I was terrified I’d lose my liver and my baby." That’s the hidden burden of PTU: constant monitoring, fear of side effects, and the emotional weight of managing a disease that can flare up at any time.
What You Need to Know If You’re on PTU
- Take it exactly as prescribed-three times a day, with food if it upsets your stomach.
- Get blood tests every 4 to 6 weeks at first. Liver tests (ALT, AST) and white blood cell counts are non-negotiable.
- If you get a sore throat, fever, or mouth ulcers, stop PTU and call your doctor. You could be developing agranulocytosis-a dangerous drop in white blood cells.
- If you feel nauseous, yellow skin, or dark urine, stop immediately. Liver damage can happen fast.
- Don’t stop PTU just because you feel better. Stopping too soon increases relapse risk.
- Smoking makes eye problems worse. Quitting is part of your treatment plan.
Most people on PTU do fine. But you need to be vigilant. Your doctor isn’t being paranoid-they’re trying to catch a rare but deadly side effect before it’s too late.
The Future: What’s Next for Graves’ Disease?
Treatment is changing. Doctors now test for TRAb (thyrotropin receptor antibody) at diagnosis and again after treatment. If levels stay above 10 IU/L, your chance of relapse is 80%. That helps decide whether to keep drugs longer or move to radioactive iodine.
New tools are emerging. A home thyroid monitor called ThyroidTrack, approved in 2022, lets you check your TSH with a finger-prick test-accuracy matches lab results. It’s not widely available yet, but it’s coming.
Researchers are testing drugs that block the thyroid-stimulating receptor directly. One called K1-70 normalized thyroid function in 85% of patients without causing hypothyroidism. That could be a game-changer.
And then there’s the hope of precision medicine. Scientists are studying genes like HLA-DR3, which triples your risk of Graves’ disease. In the next five years, we may be able to predict who responds best to PTU, who needs surgery, and who’s likely to relapse-all based on your DNA.
For now, PTU remains a critical tool. It’s not perfect. But for pregnant women, for those in thyroid storm, for some who can’t tolerate methimazole-it’s the difference between life and death. And while new drugs are on the horizon, the basics still matter: early diagnosis, careful monitoring, and knowing your body well enough to speak up when something’s wrong.
Is PTU safe during pregnancy?
PTU is the preferred antithyroid drug during the first trimester of pregnancy because it crosses the placenta less than methimazole, lowering the risk of birth defects. After the first trimester, most doctors switch back to methimazole because PTU carries a higher risk of liver damage. Always work with an endocrinologist and obstetrician to manage this carefully.
Can Graves’ disease be cured?
Graves’ disease can go into remission, meaning thyroid function returns to normal without medication. About 30 to 50% of patients achieve remission after 12 to 18 months of antithyroid drugs. But relapse is common-up to 60% of people experience it within a year of stopping treatment. Definitive treatments like radioactive iodine or surgery remove the overactive thyroid, effectively "curing" hyperthyroidism, but they cause permanent hypothyroidism that requires lifelong hormone replacement.
What are the warning signs of PTU liver damage?
Signs of liver injury from PTU include yellowing of the skin or eyes (jaundice), dark urine, nausea, vomiting, unusual fatigue, abdominal pain, and loss of appetite. If you experience any of these, stop taking PTU immediately and contact your doctor. Liver damage can develop quickly and requires urgent medical attention.
Why do some people with Graves’ disease have bulging eyes?
The same autoimmune antibodies that attack the thyroid also target tissues behind the eyes. This causes inflammation, swelling, and fat buildup, pushing the eyeballs forward-a condition called Graves’ ophthalmopathy. It affects 25 to 50% of patients. Smoking greatly increases the risk and severity. Treatment may include steroids, radiation, or surgery, depending on how advanced it is.
How long do you need to take PTU?
PTU is typically taken for 12 to 18 months, similar to methimazole. The goal is to control thyroid hormone levels until the immune system settles down. Your doctor will gradually lower the dose as your thyroid function improves. Some people need to stay on it longer if they have severe disease or are pregnant. Stopping too early increases the chance of relapse.
Can Graves’ disease come back after treatment?
Yes. Even after successful treatment with drugs, radioactive iodine, or surgery, the autoimmune process can persist. Relapse is most common after stopping antithyroid medications, with 40 to 60% of patients experiencing symptoms again within a year. After radioactive iodine or surgery, the hyperthyroidism won’t return-but you’ll need lifelong thyroid hormone replacement. Regular checkups and TRAb testing help predict who’s at higher risk.
What to Do Next
If you’ve been diagnosed with Graves’ disease and your doctor recommends PTU, ask: Why PTU over methimazole? Is it because I’m pregnant? Is my disease severe? What are the signs I need to watch for? Don’t be afraid to ask for a referral to an endocrinologist or a thyroid eye disease clinic if you have eye symptoms.
If you’re on PTU, keep your blood tests. Track your symptoms. Write down changes in your energy, weight, mood, or eyes. Bring that list to every appointment. You’re not just a patient-you’re the most important part of your care team.
Graves’ disease doesn’t define you. But understanding it-knowing how PTU works, why it’s risky, and what to expect-gives you control. And that’s the most powerful medicine of all.





12 comments
Kathryn Ware
Just wanted to say thank you for this post 🙏 I was diagnosed with Graves’ last year and PTU was my first line of defense - I cried in the parking lot after my first ALT spike too. 😭 The monthly blood tests felt like a horror movie, but honestly? Knowing my liver was being watched kept me alive. I’m 14 months in, no relapse yet, and my eyes are finally calming down. PTU isn’t glamorous, but it’s the quiet hero for so many of us. Don’t let anyone tell you it’s outdated - it saved my pregnancy and my sanity.
kora ortiz
If you're on PTU and not getting monthly liver panels you're playing Russian roulette with your organs
Kyle Swatt
It’s wild how medicine still relies on a 70-year-old drug because it’s the only one that doesn’t murder a fetus. PTU is like that one uncle who shows up to every family reunion with a broken leg but somehow keeps everyone from burning the house down. We know he’s dangerous. We know he’s messy. But if you want the baby to live? You let him stay. The real tragedy isn’t the drug - it’s that we’ve got all this fancy science and still can’t make a safer option for pregnant women. We’re treating autoimmune disease like it’s a plumbing problem - fix the leak, don’t ask why the pipe rusted in the first place.
Jessica Healey
omg i was misdiagnosed with anxiety for 2 YEARS. i thought i was just a mess. lost 30 lbs, couldn’t sleep, felt like my heart was gonna explode. then my mom saw a post about Graves’ and was like ‘is that you?’ turns out my TSH was 0.01. i still get panic attacks when i see a lab slip. also i smoked for 10 years and now my eyes look like i’m a raccoon who lost a fight. i quit. but it’s too late for the bulging. 💔
Levi Hobbs
Thank you for the detailed breakdown - I especially appreciate the note about TRAb levels predicting relapse. I’ve been on methimazole for 16 months now, and my TRAb is still at 12.3 IU/L. My endo says that’s a 78% chance of relapse if I stop. I’m considering RAI, but I’m terrified of lifelong hormone replacement. Is it really that bad? I’ve heard people say it’s just a pill and you’re fine. But it feels like trading one chronic condition for another. Any thoughts?
henry mariono
I just wanted to say I read this whole thing. I’m not on PTU. I don’t have Graves’. But I’m glad someone wrote this. I have a cousin who does. She’s 32. She’s scared. She doesn’t know how to ask questions. I’m going to print this out for her. You made something complicated feel human. Thank you.
Sridhar Suvarna
As a physician from India, I have treated over 40 cases of Graves' disease in the last decade. In our resource-limited settings, PTU remains indispensable due to cost and availability. Radioactive iodine is often inaccessible. Surgery requires infrastructure we simply do not have. We rely on PTU not because it is ideal, but because it is the only viable bridge. We monitor liver enzymes religiously - weekly in the beginning. Patients are educated to recognize jaundice as an emergency. This post is accurate and vital. We must not abandon PTU - we must optimize its use.
Joseph Peel
For those wondering about the future: K1-70 isn’t just promising - it’s revolutionary. If it passes Phase III trials, it could eliminate the need for lifelong hormone replacement after treatment. Imagine a world where you treat the autoimmune trigger, not just the symptom. No more thyroidectomy. No more radioactive iodine. No more lifelong levothyroxine. Just a targeted shot at the root cause. We’re not far off. This is the kind of science that deserves funding, not just blog posts.
Kelsey Robertson
Let’s be real - PTU is a relic. A dangerous, outdated relic. And yet, doctors still prescribe it like it’s the only option? Methimazole has been proven safer for non-pregnant adults for decades. Why are we still risking liver failure? Because Big Pharma doesn’t make enough profit off a 1947 drug. And because endocrinologists are too lazy to push for better alternatives. The FDA’s black box warning? That’s not a caution - it’s a confession. We’re poisoning people to save babies. And we call that medicine?
Joseph Townsend
Y’all are talking about PTU like it’s a villain. But let me tell you - it’s the underdog. The scrappy little drug that shows up to the party with a broken nose and a half-empty flask, but still manages to keep the baby alive while everyone else is arguing about who brought the chips. I’ve seen it. I’ve been on it. I’ve cried over my liver results. I’ve stared at my reflection in the mirror wondering if my eyes would ever stop bulging. But here I am - alive, pregnant, and still breathing. PTU didn’t cure me. But it gave me time. And sometimes… that’s all you need.
Bill Machi
Graves’ disease is a liberal conspiracy. It’s just stress. You’re all weak. I’ve never seen a real thyroid problem in my life. You think your body is broken? Try working a 12-hour shift in a factory. Try raising kids without a paycheck. This is all just modern weakness. Stop blaming your thyroid. Start blaming your phone. And stop taking that poison. PTU? That’s just another way Big Pharma makes money off your fear.
Elia DOnald Maluleke
In my country, we do not have access to teprotumumab. We do not have home thyroid monitors. We do not have the luxury of choice. We have PTU. We have hope. We have mothers who take this drug while holding their newborns, terrified of their own liver, but willing to risk it all - because love is louder than fear. I am not a doctor. I am not a scientist. I am a father whose wife survived Graves’ disease because of this drug. So I say: do not call it dangerous. Call it courageous. And do not let anyone silence the quiet heroes who take it - every day - for love.