Why Calibration and Validation Aren’t Just Paperwork
Think of a scale in a medical device factory that’s off by just 0.5 grams. Sounds small? That’s enough to make a pill too strong-or too weak-to be safe. This isn’t hypothetical. In 2023, 37.2% of FDA warning letters to medical device manufacturers cited inadequate calibration. Calibration isn’t about checking boxes. It’s about making sure every measurement your equipment gives you is trustworthy. And validation? That’s proving the whole system works the way it’s supposed to-for your specific product, in your specific environment.
Calibration: The Foundation of Trust
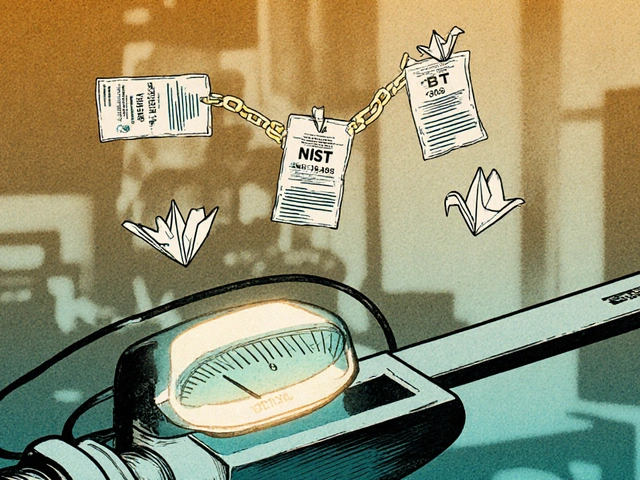
Calibration means comparing your device-like a thermometer, torque wrench, or laser sensor-to a known standard that traces back to the International System of Units (SI). This isn’t guesswork. ISO 13485:2016 requires it. So does FDA 21 CFR Part 820. The standard says your calibration must be done at specified intervals or before use, and the reference standard must be traceable through an unbroken chain of certified labs. No shortcuts.
Here’s what that looks like in practice: A micrometer used to measure implant components gets calibrated every 90 days. The lab that does it uses a reference gauge block certified by NIST, which itself was calibrated by a lab certified by BIPM. That chain of traceability is documented. Every time. If you can’t prove it, you’re not compliant.
And it’s not just about the tool. Environmental conditions matter. Calibration labs typically require 20°C ±2°C and 40% RH ±10%. If your factory floor hits 30°C during summer shifts, your tools drift. NIST Technical Note 1900 found 57.8% of out-of-tolerance incidents happened when temperatures fluctuated more than ±5°C from calibration conditions. That’s why some companies install climate-controlled calibration rooms. Others use IoT sensors to monitor real-time conditions and flag readings taken outside safe zones.
How Often Should You Calibrate?
There’s no universal answer. The manufacturer’s recommendation? A starting point, not a rule. ISO 9001 lets you determine intervals based on risk. ISO 13485 says you must justify your choice.
Here’s how smart companies do it:
- High-precision tools in aerospace or medical device assembly? Calibrate every 3 to 6 months.
- Basic thermometers in food processing? Every 12 to 24 months.
- Point-of-care glucose meters under CLIA? Only if verification is done daily with NIST-traceable controls.
One biomedical lab extended electronic scale calibration from quarterly to biannually after collecting 18 months of stability data. Saved $18,500 a year. That’s risk-based calibration in action. But if your equipment lives in a humid, dusty, or vibrating environment? You might need to calibrate more often than the manual says. Mark Rodriguez, a lab tech, found his pH meters drifted every month in high-humidity conditions-even though the manufacturer said 6 months. He adjusted. He stayed compliant.
Validation: Proving It Works for Your Use
Calibration says your scale reads 100.000 grams accurately. Validation says: “Will this scale consistently deliver pills weighing exactly 250 mg ±2 mg, every time, under real production conditions?” That’s the difference.
Validation follows GAMP 5 guidelines: three phases.
- Installation Qualification (IQ): Did you install the equipment correctly? Are all parts present? Is the software version correct? Is the environment suitable?
- Operational Qualification (OQ): Does it work across its full range? Test it at minimum, maximum, and normal settings. Does the oven heat evenly? Does the mixer blend uniformly at 100 RPM and 500 RPM?
- Performance Qualification (PQ): Does it perform as expected with actual product? Run three consecutive batches. Measure output. Document everything. This is where you prove the machine doesn’t just work-it works for your product.
Validation isn’t cheap. For complex production lines, it can cost between $25,000 and $500,000. But skipping it? That’s how you get a recall. One company skipped PQ on a tablet coating machine. The batch looked fine. But the coating thickness varied. The drug dissolved too fast. The FDA issued a Class II recall. Cost: $2.1 million.
ISO 13485 vs. CLIA vs. FDA: What’s the Real Difference?
It’s not about which standard is “better.” It’s about which one applies to you.
| Standard | Calibration Traceability | Calibration Intervals | Validation Requirements | Special Notes |
|---|---|---|---|---|
| ISO 13485:2016 | Must trace to SI units. No exceptions. | Based on risk, but must be justified. Manufacturer recommendations are a baseline. | Required for all production and test equipment. Must include IQ, OQ, PQ. | Records kept for product lifecycle + 2 years. |
| CLIA (Clinical Labs) | For waived tests: manufacturer calibration accepted if verification is done. | 6 months minimum for moderate/high complexity tests. Daily verification for high-complexity analyzers. | Verification of control materials required, not full validation. | 98.7% of labs use daily NIST-traceable controls for chemistry analyzers. |
| FDA 21 CFR Part 820 | Same as ISO 13485. Traceable to SI. | Must be established and documented. No fixed intervals. | Validation required for processes affecting product quality. | Electronic records required by Dec 31, 2026, for Class II/III devices. |
| EU MDR 2017/745 | Must trace to BIPM standards. | Same as ISO 13485. | Same as ISO 13485. | Companies selling in EU and US often maintain dual calibration systems. |
Biggest takeaway? If you’re making medical devices, ISO 13485 is your baseline. If you’re running a clinical lab, CLIA rules apply. But if you’re global? You might need to meet both. McKinsey found multinational firms spend 18.7% more to maintain dual systems.
What’s Changing Right Now?
Calibration isn’t standing still.
In March 2024, ISO updated ISO 13485 to require calibration of AI/ML-based measurement systems. That means if your quality control uses machine learning to detect defects, you can’t just calibrate the camera-you have to validate the algorithm’s output over time. Continuous monitoring is now mandatory.
FDA’s 2024 Calibration Modernization Initiative requires all Class II and III device manufacturers to switch to electronic records by December 31, 2026. That’s over 14 million paper records eliminated. Companies using cloud-based calibration software like GageList or Trescal are already ahead-they cut audit prep time by 63.2%.
And NIST is working on quantum-based standards. By 2030, electrical measurements could be 100 times more accurate. That’ll shrink calibration intervals for critical devices. But here’s the catch: 83.6% of calibration labs report technician shortages. And 47 accredited labs shut down in 2023 because they couldn’t hire qualified staff.
Common Mistakes and How to Avoid Them
- Mistake: Using manufacturer’s default interval without data. Solution: Collect performance data for 6-12 months. Adjust intervals based on actual drift.
- Mistake: Not tracking environmental conditions. Solution: Install sensors. Log temperature and humidity during calibration and use.
- Mistake: Validation only happens once. Solution: Re-validate after major repairs, software updates, or if you change the product.
- Mistake: Calibration records are messy or incomplete. Solution: Use software that auto-generates certificates and links them to equipment IDs. One company reduced record management from 15.2 hours per week to 4.1.
- Mistake: Assuming off-the-shelf software is “validated.” Solution: Even if the vendor provides a certificate, you still need to validate it works in your environment.

Who Should Do This?
You don’t need a PhD in metrology. But you do need trained people.
ASQ’s Certified Calibration Technician (CCT) credential is held by over 14,000 professionals globally. Those with the certification earn 22.5% more than non-certified peers. Training programs like NCSL International’s MET-101 course cover the fundamentals: uncertainty calculations, traceability chains, documentation standards.
Small manufacturers (<50 employees) pay 22.3% more per device to comply because they can’t negotiate bulk rates with calibration labs. That’s why many outsource calibration-but even then, they must manage the process, track certificates, and ensure traceability.
Where to Start
If you’re starting from scratch, here’s your 6-month plan:
- Month 1-2: Inventory every measurement device. Assign unique IDs. Note manufacturer, model, location, and criticality.
- Month 3: Classify each device by risk. High-risk = critical to product safety. Medium = affects efficiency. Low = non-critical.
- Month 4: Set initial calibration intervals based on manufacturer specs and risk. Document your rationale.
- Month 5: Choose a calibration management system. Pick one that integrates with your ERP. Avoid paper logs.
- Month 6: Train your team. Start calibration. Begin validation on your most critical machine.
Don’t try to do everything at once. Focus on the tools that directly impact product safety. Get those right. Then expand.
Final Thought: It’s Not About Compliance. It’s About Confidence.
Calibration and validation aren’t costs. They’re insurance. Insurance that your product won’t harm someone. Insurance that your audit won’t end in a shutdown. Insurance that your customers trust you.
Companies that treat this as a compliance chore end up paying more in recalls, delays, and lost reputation. Those that treat it as a core quality discipline? They sleep better. And they grow.
What’s the difference between calibration and validation?
Calibration checks if a device reads accurately against a known standard-like making sure your scale shows exactly 100 grams when it should. Validation proves the entire system works correctly for its intended use-like confirming that your filling machine consistently dispenses 250 mg pills within tolerance, under real production conditions. Calibration is about measurement accuracy. Validation is about process reliability.
How often should I calibrate my equipment?
There’s no universal answer. Start with the manufacturer’s recommendation, then adjust based on risk and real-world performance. High-precision tools in medical device manufacturing often need calibration every 3-6 months. Basic tools like thermometers may only need it every 12-24 months. Use historical data to justify longer intervals. If your environment is harsh-hot, humid, or vibrating-you may need to calibrate more often.
Do I need to validate every piece of equipment?
No. Only equipment that directly affects product quality, safety, or regulatory compliance needs full validation (IQ, OQ, PQ). A simple ruler used to measure packaging dimensions might only need calibration. But a robotic arm that places components inside a pacemaker? That needs full validation. Focus your resources on what matters most.
What happens if I don’t calibrate or validate?
You risk product failures, regulatory action, and recalls. In 2023, nearly 4 out of 10 FDA warning letters cited calibration failures. A single out-of-tolerance measurement can lead to defective products reaching patients. Beyond safety, non-compliance can halt production, trigger audits, and damage your reputation. The cost of fixing it later is always higher than preventing it.
Can I use software to manage calibration and validation?
Yes-and you should. Cloud-based calibration software like GageList, Trescal, or MasterControl automates scheduling, generates certificates, tracks equipment status, and stores records securely. Companies using these tools cut audit prep time by over 60%. They also reduce human error and ensure traceability. Look for software that integrates with your existing systems and meets FDA 21 CFR Part 11 requirements for electronic records.
Is calibration required for software or AI systems?
Yes, starting with the March 2024 update to ISO 13485. If your quality system uses AI to inspect parts or analyze data, you must validate the algorithm’s performance over time. This includes monitoring for drift, retraining the model with new data, and documenting that it continues to meet specifications. It’s no longer enough to calibrate the camera-you must validate the AI’s decision-making process.




11 comments
Michael Fitzpatrick
Man, I’ve seen so many shops skip calibration because ‘it’s been fine for years.’ Then the FDA shows up, and suddenly everyone’s scrambling to write up 3 years of missing logs. It’s not just compliance-it’s protecting real people. That 0.5g drift? Could be a kid getting the wrong dose of insulin. No joke.
And honestly? The environmental stuff is the silent killer. I worked at a lab where the AC died for three days in July. We didn’t realize our micrometers had drifted until the next batch of pacemakers failed QC. Never again.
Ravi Kumar Gupta
Bro, in India we still use analog torque wrenches from 1998 because ‘why buy new when old works?’ Then we wonder why our exports get rejected. Calibration isn’t luxury-it’s survival. If you’re making medical stuff for the world, you play by the world’s rules. No excuses.
NIST? BIPM? We don’t even know what those acronyms mean half the time. Time to wake up.
Danny Nicholls
Just had a QA audit last week and we switched to GageList last month. Holy crap, it cut our prep time in half 😍
Also, we started logging temp/humidity with cheap IoT sensors from Amazon-$40 each. Now we flag bad readings in real time. No more ‘oops, we forgot to check the room temp’ moments. 🙌
Also, validation doesn’t have to cost $500k. We did ours in-house with a grad student and saved $200k. Just document everything. Even if it’s messy at first.
Mark Williams
Let’s not conflate calibration with validation. Calibration is metrological traceability-SI units, uncertainty budgets, NIST chains. Validation is process capability-PQ runs, worst-case scenarios, statistical process control. One ensures accuracy; the other ensures precision and robustness.
Many organizations treat them as interchangeable, which is why we see so many Class II recalls. You can have a perfectly calibrated machine that’s still producing out-of-spec product if the process isn’t validated. It’s not semantics-it’s systems thinking.
Rahul Kanakarajan
Everyone’s acting like this is groundbreaking. Newsflash: if your calibration records are handwritten on napkins, you’re already in violation. This isn’t ‘best practice’-it’s the bare minimum. If you’re still using paper logs in 2025, you’re not a manufacturer-you’re a liability waiting to happen.
And don’t get me started on ‘we can’t afford software.’ You can’t afford NOT to. One recall wipes out five years of profits.
David Cunningham
Had a similar issue with a UV spectrophotometer in Sydney. Manufacturer said cal every 6 months. We saw drift every 45 days because of the coastal humidity. Changed to 45-day cycle. No issues since. Simple fix. Data > manuals.
Also, NIST’s quantum standards are coming fast. We’re already prepping for it. The labs that wait until the deadline will be left behind.
luke young
Big thanks for laying this out so clearly. I’ve been trying to explain this to my boss for months and he kept saying ‘we’re not a pharma company.’ But we make surgical clips-so yeah, we are. This post just gave me the ammo I needed 😊
manish chaturvedi
In many developing regions, we don’t have access to certified labs. We rely on regional metrology centers that may not be ISO accredited. So we create internal traceability chains using reference standards from trusted suppliers, and we document every step with photos, timestamps, and witness signatures.
It’s not ideal, but it’s what we have. The key is transparency. If you can show your chain-even if it’s not perfect-the regulators will often work with you. But you must be honest. No faking data. That’s the line we don’t cross.
Also, training local technicians matters more than buying expensive gear. One skilled person with a basic kit can outperform ten untrained ones with top-tier tools.
Daniel Jean-Baptiste
Validation is where most companies fail-not because they don’t know how, but because they think it’s a one-time checkbox. I’ve seen teams validate a machine, then upgrade the firmware six months later and never re-validate. That’s like saying your car passed inspection so you never need to change the oil.
Just document the change. Test it. Move on. It takes two days. Not two weeks. And if your QA team says it’s ‘too expensive,’ ask them how much a recall costs. Then shut up and do it.
Robin Johnson
For anyone thinking ‘we’re small, we don’t need this’-you’re wrong. The FDA doesn’t care if you’re a startup or a Fortune 500. If your device touches a human, you’re under the microscope.
Start small. Pick one critical tool. Calibrate it. Log it. Validate the process around it. Build the habit. Then expand. You don’t need to boil the ocean. Just start with one drop. Consistency beats perfection every time.
Danny Nicholls
^^^ this. Also, if you’re still using Excel for calibration logs, you’re one typo away from a 483. I’ve seen ‘100.000’ become ‘100000’ and no one noticed until the audit. Use software. Even the cheap ones. It’s worth it.
Also, shoutout to the guy who said ‘we extended calibration to biannually after data’-that’s the future. Risk-based, not calendar-based. 🙌