Every year, the U.S. Food and Drug Administration approves hundreds of generic drugs. These aren’t just cheaper versions of brand-name pills-they’re massive cost-savers for patients, insurers, and the whole health system. But how much money do they actually save? And does it change from year to year? The numbers tell a clear story: generic drug approvals are one of the biggest drivers of affordable healthcare in America.
What Counts as a Generic Savings?
There are two ways to measure savings from generic drugs, and they show different sides of the same coin. The FDA looks at what happens in the first year after a new generic hits the market. If a brand-name drug costs $500 a month and a generic comes in at $50, the savings come from two places: the new patients switching to the cheaper version, and the brand-name company lowering its price to compete. That’s what the FDA tracks. The Association for Accessible Medicines (AAM) takes a broader view. They add up all the money saved by every generic drug sold in a year-not just the new ones. That includes generics that have been on the market for five years or more. The AAM’s numbers are much bigger because they reflect the full impact of decades of generic competition. So if you see $7 billion in one report and $400 billion in another, it’s not a contradiction. One is about new entries. The other is about the entire system.Year-by-Year Breakdown: New Generic Approvals (FDA Data)
The FDA’s numbers for first-time generic approvals show wild swings. It’s not a steady climb. It’s more like a rollercoaster based on which big drugs lose patent protection. In 2019, savings from new generic approvals hit $7.1 billion-the highest in recent years. That was because several blockbuster drugs, including a major cholesterol medication and a top-selling antidepressant, went generic all at once. The market reacted fast. Prices dropped 70% or more within months. Then came 2020. Savings plummeted to just $1.1 billion. Why? No major patents expired that year. It wasn’t that fewer generics were approved-it’s that none of them were for high-revenue drugs. The system doesn’t save billions unless a drug with billions in sales goes generic. 2021 brought $1.37 billion in savings from new generics. Still low, but not a disaster. Then in 2022, it jumped again to $5.2 billion. The FDA noted this was due to several approvals in large markets-meaning drugs used by millions of people, like diabetes or blood pressure medications. Here’s the pattern: when a high-demand drug loses exclusivity, savings spike. When it doesn’t, they drop. That’s why 2018 ($2.7B), 2019 ($7.1B), and 2022 ($5.2B) stand out. The other years? They’re the quiet ones.Total Savings: The Real Impact of All Generics
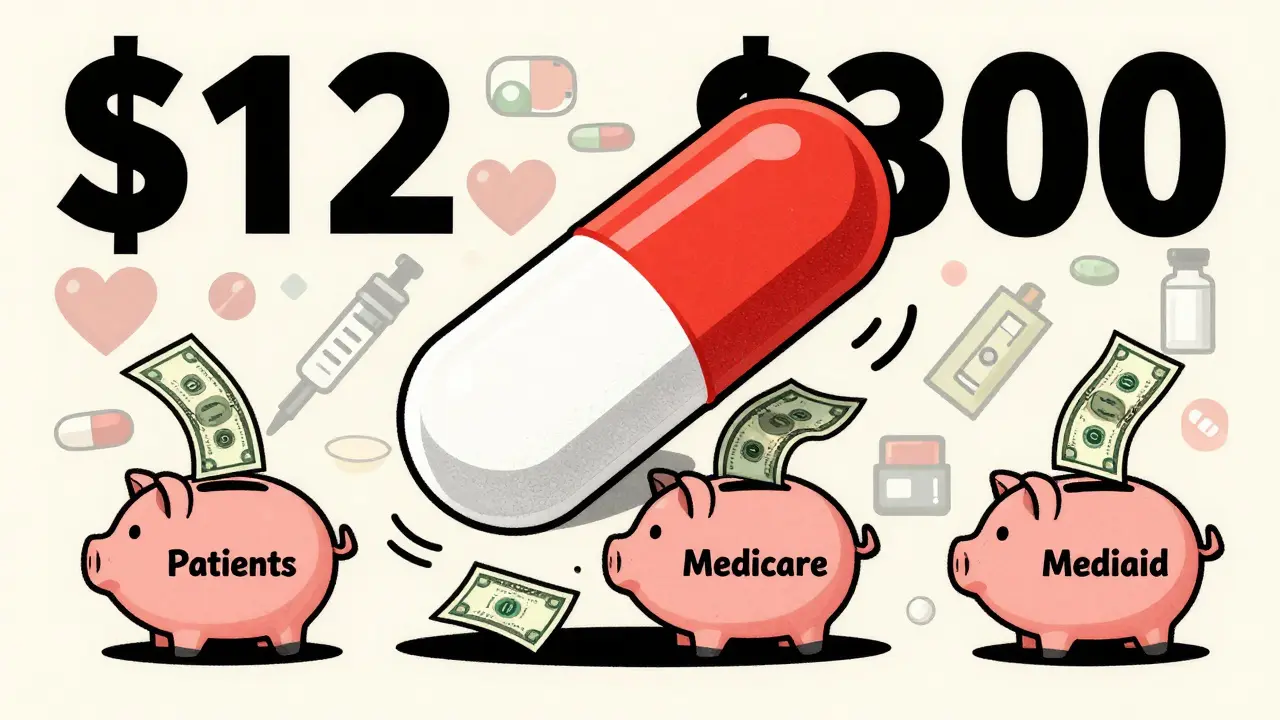
While the FDA tracks new entries, the AAM shows the full picture. In 2023 alone, generic drugs saved the U.S. healthcare system $445 billion. That’s more than the entire annual budget of the Department of Education. This isn’t a one-year fluke. Since 2014, generics have saved $3.1 trillion. And that’s just small-molecule generics-not even counting biosimilars yet. Where does that money go? Medicare saved $137 billion in 2023. That’s an average of $2,672 per beneficiary. Commercial insurers saved $206 billion. Medicaid saved the rest. In California alone, generics saved $38 billion. In Alaska, it was $354 million. The scale matches population size. Therapeutic areas show where the biggest wins are:- Heart disease: $118.1 billion saved
- Mental health: $76.4 billion saved
- Cancer: $25.5 billion saved

How Do Generics Cut Costs So Much?
A brand-name drug can cost $1,000 a month because the company spent $2 billion on R&D and has a monopoly. Once the patent expires, dozens of companies can make the same pill. They don’t need to recoup R&D. They just need to make enough to cover production and stay competitive. The result? Prices drop by 70% to 90% within a year. The FDA found that after a generic enters the market, the brand-name version often cuts its price too-sometimes by half-to keep customers. In 2021, five generic drugs accounted for nearly half of all first-generic savings. One of them was a cholesterol drug that had been selling for $300 a month. The generic? $12. That’s the kind of change that turns a chronic condition from a financial burden into a manageable cost.Who Benefits the Most?
Patients see the biggest immediate relief. The average generic copay is $6.97. Ninety-two percent of generic prescriptions cost $20 or less. For someone on a fixed income, that’s the difference between taking their medicine and skipping doses. But here’s the catch: not all savings reach the patient. Pharmacy benefit managers (PBMs) negotiate rebates between drugmakers and insurers. A 2023 Senate investigation found only 50% to 70% of generic savings actually lower out-of-pocket costs. The rest gets absorbed in the middle. State Medicaid programs see the clearest benefit. California’s Medi-Cal saved $23.4 billion in one year. That’s money that can go toward other health services instead of paying inflated drug prices.
Why Don’t We See More Savings Every Year?
It’s not that generics aren’t working. It’s that their impact is tied to patent cliffs. If no big drugs expire in a given year, savings drop. That’s why 2020 was so low. There’s also a new challenge: complex drugs. Biologics-like insulin or rheumatoid arthritis treatments-are harder to copy. Biosimilars (the generic version of biologics) are slowly coming online, but they’re still only 59 approved as of August 2024. They’re expensive to develop and slow to get approved. Some brand-name companies also use legal tricks to delay generics. Things like patent thickets, exclusive licensing deals, and REMS (Risk Evaluation and Mitigation Strategies) can block competition-even when the patent is technically expired. The FDA’s 2023 Drug Competition Action Plan is trying to fix this. They’re pushing for faster reviews, clearer rules on complex generics, and more transparency around delays.What’s Next?
By 2033, U.S. generic drug revenue is projected to hit $131.8 billion. That’s not because more people are using generics-it’s because more high-cost drugs are going generic. Drugs like Humira, Enbrel, and others with multi-billion-dollar sales are approaching patent expiry. When they do, we’ll see another spike in savings. The AAM projects that by 2028, cumulative savings from generics and biosimilars will hit $3.9 trillion. That’s almost $500 billion a year. The bottom line? Generics aren’t just a cost-cutting tool. They’re a lifeline. They turn unaffordable treatments into everyday medicines. And every time a new generic is approved, it doesn’t just lower a price-it changes a life.Key Takeaways
- New generic approvals save billions in the first year, but the amount varies wildly based on which drugs go generic.
- Total annual savings from all generics reached $445 billion in 2023-far larger than new approval savings alone.
- Heart disease, mental health, and diabetes drugs generate the biggest savings due to high usage and high brand prices.
- Patients pay far less for generics, but not all savings reach them due to PBM rebate structures.
- Future savings depend on complex drug approvals, biosimilars, and breaking down barriers to generic competition.
How much do generic drugs save patients annually?
In 2023, generic drugs saved U.S. patients and the healthcare system a total of $445 billion. The average generic prescription costs under $7 out-of-pocket, compared to hundreds for brand-name versions. For chronic conditions like high blood pressure or diabetes, this means savings of thousands of dollars per year per person.
Why do generic savings vary so much from year to year?
Savings spike when a high-revenue brand-name drug loses patent protection. In 2019, savings hit $7.1 billion because several blockbuster drugs went generic at once. In 2020, savings dropped to $1.1 billion because no major drugs expired. The system depends on patent cliffs, not steady growth.
Do generic drugs save money for Medicare and Medicaid?
Yes. In 2023, Medicare saved $137 billion thanks to generics-about $2,672 per beneficiary. Medicaid saved the remainder of the $445 billion total. State programs like California’s Medi-Cal saved over $23 billion in a single year. These savings allow programs to stretch budgets further.
Are all generic savings passed on to patients?
Not always. While generics cost far less, pharmacy benefit managers (PBMs) often keep a portion of the savings through rebates and contracts with insurers. A 2023 Senate investigation found only 50-70% of the savings reach the patient directly. The rest stays in the middle of the supply chain.
What’s the difference between generics and biosimilars?
Generics are exact copies of small-molecule drugs (like pills for cholesterol or blood pressure). Biosimilars are similar, but not identical, copies of complex biologic drugs (like insulin or cancer treatments). Biosimilars are harder and more expensive to make. As of 2024, the FDA has approved 59 biosimilars, but they’ve contributed far less to total savings than traditional generics.




9 comments
Kelly McRainey Moore
Just saw my grandma fill her insulin prescription for $4 this month. Last year it was $450. Generics aren't just numbers-they're people breathing easier.
Philip Williams
The structural disparity between FDA-reported first-year savings and AAM’s cumulative totals is not merely a matter of scope-it reflects a fundamental misalignment in policy metrics. The FDA’s narrow lens incentivizes short-term patent cliffs while ignoring the compounding, systemic impact of generic market saturation. This isn’t just an accounting difference; it’s a governance failure.
Stephen Rock
PBMs are the real villains here. They take 30% of the savings and call it ‘negotiation.’ Meanwhile, people still choose between food and meds. This whole system is rigged.
Jarrod Flesch
Love this breakdown! 🙌 Just had my blood pressure med go generic last month-went from $120 to $8. Made me cry a little. Thanks for putting the human side out there!
Alex Carletti Gouvea
Generics? More like government-approved price fixing. Why should American companies lose billions just because some foreign factory can copy a pill? We built this innovation-why are we rewarding cheaters?
Dee Monroe
There’s something deeply spiritual about the idea that a simple molecule, once hoarded behind patents and profit margins, can become a shared gift to humanity. When a drug goes generic, it’s not just economics-it’s justice. It’s the moment a life stops being a balance sheet and becomes a person again. The fact that we’ve saved $3.1 trillion in a decade doesn’t surprise me. What surprises me is that we still treat this as a policy debate instead of a moral imperative. We could end chronic medication poverty in this country tomorrow-if we chose to.
Barbara Mahone
The distinction between small-molecule generics and biosimilars is critical and often misunderstood. Biosimilars require extensive analytical characterization due to their structural complexity, which explains both their higher development cost and slower market penetration. Regulatory clarity and reimbursement alignment are the next frontiers.
Andrew Rinaldi
I get why some people are frustrated with PBMs, but blaming them entirely misses the bigger picture. The real problem is that our system ties drug pricing to insurance networks instead of direct cost-to-produce. Maybe the solution isn’t more regulation-it’s rethinking how we pay for medicine altogether.
Gerard Jordan
Just shared this with my sister who’s on 5 meds. She said, ‘I didn’t know I was part of a $445 billion story.’ 💙 Let’s keep talking like this-real people, real savings, real change.