Candidemia: What It Is, How You Spot It, and How to Treat It
If you’ve ever heard the word “candidemia” and wondered what it means, you’re not alone. It’s simply a bloodstream infection caused by the Candida fungus. While Candida lives on skin and inside the gut harmlessly, it can turn dangerous when it gets into the blood. Below we break down the basics so you know what to watch for and what doctors do about it.
How Candidemia Happens
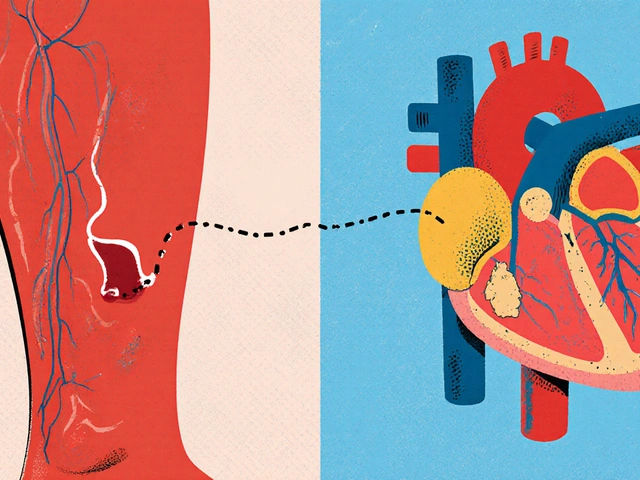
Most cases start when a catheter, IV line, or surgical wound lets the fungus slip from the skin or gut into the bloodstream. People in intensive care, those on long‑term antibiotics, or anyone with a weakened immune system are most at risk. Birth control pills, diabetes, and even uncontrolled blood sugar can make it easier for Candida to spread.
In hospitals, the fungus can hitch a ride on equipment or on the hands of staff. That’s why strict cleaning and hand‑washing rules matter a lot. If you’ve had recent surgery or a central line, keep an eye on any new symptoms.
Typical Signs and When to Call the Doctor
Candidemia doesn’t have a single tell‑tale sign, but most people notice a mix of fever, chills, and a rapid heartbeat that won’t go away with usual antibiotics. You might also feel tired, have muscle aches, or notice a sudden drop in blood pressure. In severe cases, the infection can spread to the eyes, heart, or brain, causing vision problems, heart rhythm issues, or confusion.
If you’re in the hospital and develop a fever that pops up out of nowhere, let the staff know right away. Outside the hospital, any persistent high fever—especially if you have a catheter or recent surgery—should trigger a call to your doctor.Doctors will usually order blood cultures to see if Candida is growing. These tests can take a day or two, but they’re the gold standard for confirming candidemia.
Treatment Options You’ll Hear About
Once Candida is confirmed, treatment starts fast. The first‑line drugs are antifungal medications like fluconazole or an echinocandin (caspofungin, micafungin, or anidulafungin). The exact choice depends on the Candida species and how sick the patient is.
Typical treatment lasts about two weeks after the blood cultures turn negative, but doctors may extend it if the infection has moved to other organs. Removing or replacing any infected catheter is a must—an untreated line can keep feeding the fungus.
Side effects of antifungals can include stomach upset or liver‑enzyme changes, so doctors will check blood work regularly. Most people finish the course without major problems, and the infection clears up.
Preventing Candidemia Before It Starts
Prevention is mostly about good hygiene and smart medical care. If you have a central line, ask the nursing team how often they change dressings and whether they follow sterile technique. For patients on long‑term antibiotics, discuss with your doctor whether a probiotic or antifungal prophylaxis is appropriate.
Keeping blood sugar under control, staying hydrated, and eating a balanced diet also help your immune system stay strong. If you’re on chemotherapy or steroids, stay alert for any new fever and report it early.
In short, candidemia is a serious but treatable bloodstream infection. Knowing the risk factors, spotting the symptoms early, and getting prompt antifungal therapy are the keys to a full recovery. Keep these points in mind, and you’ll be better equipped to handle the situation if it ever arises.

- Sep 2, 2025
- Posted by Cillian Osterfield
Candidemia, Disseminated Candida, and Antifungal Resistance: What Clinicians Need to Know
Clear guide on how candidemia spreads, why resistance is rising, and what to do-from diagnosis to therapy choices, source control, and practical checklists.
Categories
- Health and Wellness (71)
- Medications (68)
- Health and Medicine (28)
- Pharmacy Services (12)
- Mental Health (9)
- Health and Career (2)
- Medical Research (2)
- Business and Finance (2)
- Health Information (2)
Latest Posts
©2026 heydoctor.su. All rights reserved